Fill Out Your Aetna International Claim Form
The Aetna International Claim Form is an essential document for members seeking reimbursement for various healthcare services, including medical, dental, maternity, vision, and wellness treatments. To ensure a smooth claims process, individuals must complete several sections of the form accurately, including member and patient information, details of other health insurance coverage, and specific claim information. Each family member requires a separate claim form, and it is vital to include itemized bills and receipts. For those submitting claims related to accidental injuries or long-term treatments, additional details and documentation are necessary. Members should also be aware of the importance of submitting their claims within 180 days of the treatment date to avoid processing delays. The form requests information regarding the preferred method of reimbursement, such as bank transfers or checks, and includes sections for declarations concerning the accuracy of the provided information. A comprehensive understanding of this form contributes significantly to minimizing hurdles in receiving owed benefits, thus allowing members to focus on their health and well-being.
Aetna International Claim Example
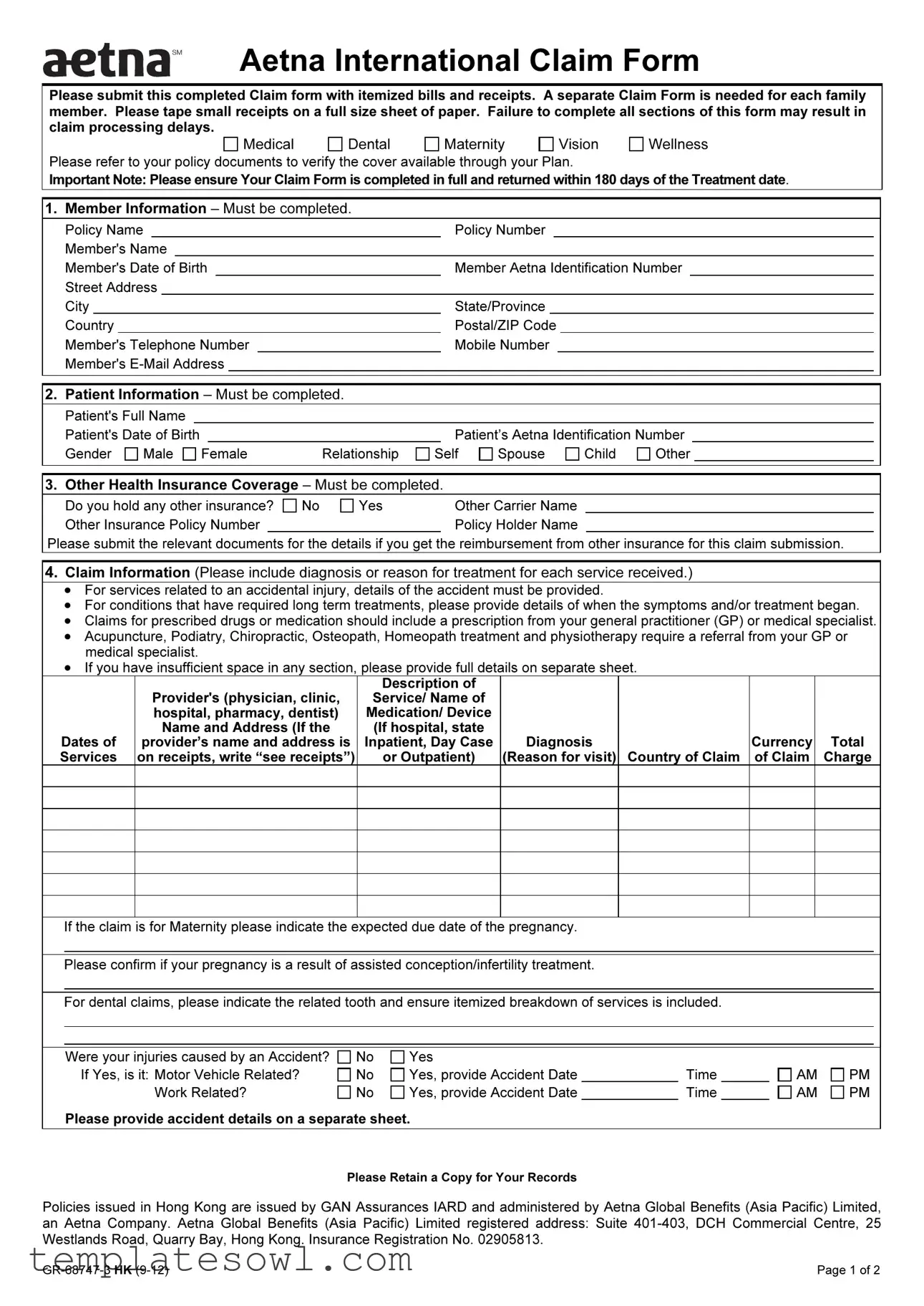
Aetna International Claim Form
Please submit this completed Claim form with itemized bills and receipts. A separate Claim Form is needed for each family member. Please tape small receipts on a full size sheet of paper. Failure to complete all sections of this form may result in claim processing delays.
Medical
Dental
Maternity
Vision
Wellness
Please refer to your policy documents to verify the cover available through your Plan.
Important Note: Please ensure Your Claim Form is completed in full and returned within 180 days of the Treatment date.
1. Member Information – Must be completed.
Policy Name |
|
Policy Number |
|
||||||||
Member's Name |
|
|
|
|
|
||||||
Member's Date of Birth |
|
Member Aetna Identification Number |
|
|
|||||||
Street Address |
|
|
|
|
|
||||||
City |
|
State/Province |
|
||||||||
Country |
|
Postal/ZIP Code |
|
||||||||
Member's Telephone Number |
|
Mobile Number |
|
|
|||||||
Member's |
|
|
|
|
|||||||
|
|
|
|
|
|||||||
|
|
|
|
|
|||||||
2. Patient Information – Must be completed. |
|
|
|
|
|||||||
Patient's Full Name |
|
|
|
Patient's Date of Birth |
|
|
|
Gender |
Male |
Female |
Relationship |
Patient’s Aetna Identification Number
Self |
Spouse |
Child |
Other |
3. Other Health Insurance Coverage – Must be completed.
Do you hold any other insurance? |
No |
Yes |
Other Carrier Name |
|
Other Insurance Policy Number |
|
|
|
Policy Holder Name |
Please submit the relevant documents for the details if you get the reimbursement from other insurance for this claim submission.
4.Claim Information (Please include diagnosis or reason for treatment for each service received.)
•For services related to an accidental injury, details of the accident must be provided.
•For conditions that have required long term treatments, please provide details of when the symptoms and/or treatment began.
•Claims for prescribed drugs or medication should include a prescription from your general practitioner (GP) or medical specialist.
•Acupuncture, Podiatry, Chiropractic, Osteopath, Homeopath treatment and physiotherapy require a referral from your GP or medical specialist.
•If you have insufficient space in any section, please provide full details on separate sheet.
|
|
Description of |
|
|
|
|
|
Provider's (physician, clinic, |
Service/ Name of |
|
|
|
|
|
hospital, pharmacy, dentist) |
Medication/ Device |
|
|
|
|
|
Name and Address (If the |
(If hospital, state |
|
|
|
|
Dates of |
provider’s name and address is |
Inpatient, Day Case |
Diagnosis |
|
Currency |
Total |
Services |
on receipts, write “see receipts”) |
or Outpatient) |
(Reason for visit) |
Country of Claim |
of Claim |
Charge |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
If the claim is for Maternity please indicate the expected due date of the pregnancy.
Please confirm if your pregnancy is a result of assisted conception/infertility treatment.
For dental claims, please indicate the related tooth and ensure itemized breakdown of services is included.
Were your injuries caused by an Accident? |
No |
Yes |
|
|
If Yes, is it: Motor Vehicle Related? |
No |
Yes, provide Accident Date |
|
Time |
Work Related? |
No |
Yes, provide Accident Date |
|
Time |
Please provide accident details on a separate sheet.
AM AM
PM PM
Please Retain a Copy for Your Records
Policies issued in Hong Kong are issued by GAN Assurances IARD and administered by Aetna Global Benefits (Asia Pacific) Limited, an Aetna Company. Aetna Global Benefits (Asia Pacific) Limited registered address: Suite
Page 1 of 2 |
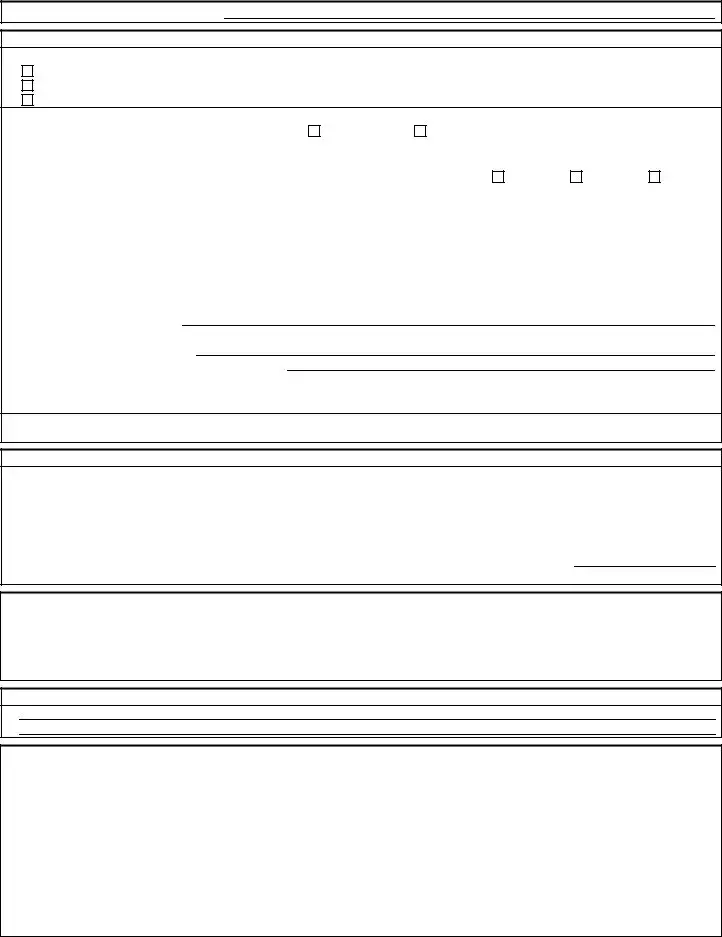
Member’s Name (For faxing purpose):
5. Summary of Payment Details – Must be completed.
Recurring Reimbursement Election – Please check one of the following options if you want to:
Receive future payments using the details provided below
Use the payment information provided below for this claim only
Use the payment details that we already have on file for you
Payment Information
|
Please select your preferred reimbursement method: |
Bank Transfer |
Cheque |
|
|
|
|
|||||||||
|
(If no selection is made, the default method is cheque issued in the member’s name.) |
|
|
|
|
|||||||||||
|
Please indicate your preferred payment currency (If none is indicated, the default currency is US Dollar.) |
|
|
|
||||||||||||
|
Payee Name |
|
|
|
|
Specify if: |
Member |
Provider |
Employer |
|
||||||
|
Claim Settlement Address (if different to Section 1): |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Street |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
City |
|
|
State/Province |
Country |
|
|
|
||||||||
|
If you have selected Bank Transfer as your preferred payment method, the following information is required: |
|
|
|||||||||||||
|
Bank Account Holder Name (as per Bank Statement) |
|
|
|
|
|
|
|
|
|
|
|
||||
|
Bank Account Number |
|
|
|
Sort Code/Branch Code |
|
|
|
|
|
||||||
|
IBAN Code* |
|
|
|
Swift/BIC Code |
|
|
|
|
|
||||||
|
IFSC/ABA/ US Routing Code |
|
|
|
|
|
|
|
|
|
|
|
||||
|
Bank Name |
|
|
|
|
|
|
|
|
|
|
|
|
|||
Bank Address (include Country)
Bank Telephone Number (include Country Code)
*The IBAN is mandatory for bank transfer claim payment transactions in certain countries, such as the United Arab Emirates (UAE). This must be supplied if you are using a bank account in one of these countries. Members should check with their bank to confirm any IBAN requirements.
The most efficient method of receiving your benefits reimbursement is via Bank Transfer. Please check with your bank for help with providing the appropriate instructions to Aetna International.
6.Declaration – Must be completed.
I declare that, to the best of my knowledge, all the information provided on this claim form is truthful and correct. I understand that Aetna will rely on the information provided as such. I agree and accept that this declaration gives Aetna, and its appointed representatives, the right to request past, present, and future medical information in relation to this claim, or any other claim related to the member/covered individual, from any third party, including providers and medical practitioners. I declare and agree
that personal information may be collected, held, disclosed, or transferred (worldwide) to any organization within the Aetna group, its suppliers, providers and any affiliates.
Patient's Signature |
|
Date |
(If patient is under 18 years of age, Parent or Guardian must sign.) |
|
|
Important Note: Please ensure Your Claim Form is completed in full and returned within six months (180 days) of the Treatment date. Failure to complete your form in full will result in the form being returned to you and will delay the processing of your claim. Please note Aetna International is not responsible for any costs associated with the completion of this form or for any further information/ document requested by Us to assess Your claim. The issuing of this Claim Form is in no way an admission of liability.
Please refer to your Member Handbook under General Claims Information for
7. Additional Information
How to submit a Claim
Aetna International provides alternative methods of submitting a claim form to make it easier for our members, below are the listed options:
• Postal Submission |
• Online Claim Submission for our members via our |
Aetna Global Benefits (Asia Pacific) Limited |
secure portal |
Suite |
www.AetnaInternational.com |
DCH Commercial Centre |
• Submit your claim via Fax attaching receipts and |
25 Westlands Road |
referrals from your Medical Practitioner |
Quarry Bay |
|
Hong Kong |
• Email Submission with copies of your receipts and |
|
referrals from your Medical Practitioner |
|
AsiaPacServices@aetna.com |
|
• For claim related queries please contact our 24 hour |
|
Member Services helpline |
|
Please Retain a Copy for Your Records
Policies issued in Hong Kong are issued by GAN Assurances IARD and administered by Aetna Global Benefits (Asia Pacific) Limited, an Aetna Company. Aetna Global Benefits (Asia Pacific) Limited registered address: Suite
Page 2 of 2 |
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Requirement | The Aetna International Claim Form must be completed and submitted with itemized bills and receipts. |
| Family Member Submission | A separate Claim Form is required for each family member seeking reimbursement. |
| Submission Deadline | Claims must be submitted within 180 days of the treatment date to avoid processing delays. |
| Insurance Information | Complete details on any other health insurance coverage are necessary if applicable. |
| Payment Preferences | Members can choose between receiving payments via bank transfer or cheque; bank transfer is often more efficient. |
| Declaration Requirement | The form requires a declaration confirming that all information provided is truthful and accurate. |
| Submission Methods | Claims can be submitted via postal mail, online through the secure portal, fax, or email. |
Guidelines on Utilizing Aetna International Claim
Completing the Aetna International Claim form accurately is essential to ensure timely processing of your claim. Each section of the form must be filled out carefully, as incomplete information can lead to delays. Here’s a step-by-step guide to help you navigate the form effectively.
- Member Information: Fill in all required details including your policy name, policy number, your name, date of birth, Aetna identification number, address, and contact information.
- Patient Information: Enter the patient’s full name, date of birth, gender, relationship to the member, and the patient’s Aetna identification number.
- Other Health Insurance Coverage: Indicate whether you hold any other insurance. If yes, provide the other carrier's name and policy number, along with the name of the policy holder. Include necessary documentation if you’re claiming reimbursement from another insurer.
- Claim Information: Detail the diagnosis or reason for treatment for each service received. Add specifics for accidental injuries, long-term treatments, prescribed medications, and any necessary referrals. If space is insufficient, use an additional sheet.
- Summary of Payment Details: Choose how you would like to receive future payments, whether for this claim only or for recurring payments. Fill out your reimbursement method and any required bank details if you choose bank transfer.
- Declaration: Sign and date the form, confirming that all information is accurate. Remember, if the patient is under 18, a parent or guardian must sign.
- Additional Information: Review the submission methods provided. You can submit your claim via postal mail, online, fax, or email, ensuring all necessary receipts and referrals are attached.
Double-check your entries for accuracy before submitting the form. Keep a copy of the completed claim for your records. Timely submission within 180 days post-treatment is critical in avoiding delays in processing your claim.
What You Should Know About This Form
What is the Aetna International Claim Form used for?
The Aetna International Claim Form is used to submit claims for medical, dental, maternity, vision, and wellness expenses incurred by policyholders. Completing this form allows members to request reimbursement from Aetna for healthcare services received. Each family member requires a separate claim form to ensure accurate processing.
What information do I need to provide on the claim form?
To complete the claim form, you must provide essential information about yourself and the patient, which includes your policy details, identification numbers, and contact information. The form also requires details about other health insurance coverage, specific treatment information, and payment preferences. Ensure that you include a description of the services received, diagnosis information, and any relevant receipts or bills, including itemized lists for dental claims.
How should I submit the claim form?
You can submit the Aetna International Claim Form through several methods. Options include mailing the form, using the online secure portal, sending it via fax, or emailing a scanned copy of the completed form along with receipts and referrals. The form should be submitted within 180 days of the treatment date to avoid delays in processing.
What happens if I do not provide all required information?
If you do not complete all sections of the claim form, there may be delays in processing your claim. Aetna will return incomplete forms for you to revise. It's important to double-check all entries before submission to ensure accuracy and completeness.
Can I choose how I receive my reimbursement?
Yes, you have options for receiving your reimbursement. You can select to receive future payments in a preferred method, or specify payment details for the current claim only. Available options include bank transfer or cheque. If you choose a bank transfer, you will need to provide additional banking details.
What should I do if I have further questions about my claim?
If you have questions regarding your claim or the submission process, you can contact Aetna’s member services helpline available 24 hours a day. They can assist with any claim-related inquiries and provide clarification about the process.
Common mistakes
Filling out the Aetna International Claim Form can be straightforward, but many individuals make common mistakes that can lead to processing delays or complications. Understanding these potential pitfalls can significantly improve the likelihood of a timely claim approval.
One frequent mistake is not completing all sections of the form. Each part of the Claim Form is important. If even one section is left blank, it could result in the form being returned and the processing time being extended. Ensuring that every required detail is filled out accurately will not only expedite the process but also help avoid potential confusion during review.
Another error involves the inclusion of medical bills and receipts. Simply submitting the claim form without the corresponding itemized bills and receipts can result in rejection of the claim. It's essential to attach all necessary documentation, as these receipts provide proof of the services rendered and the amounts charged. Taping up small receipts on a full-size sheet of paper is advised for ease of review and processing.
People also often forget to submit a separate Claim Form for each family member. Claims for multiple family members should not be combined on a single form. Instead, individual forms are required, which helps ensure that each claim is processed correctly and independently. This separation aids in clearer communication and tracking of each member’s claims.
Another critical area often overlooked is the section regarding other health insurance coverage. If a person has additional insurance, failure to disclose it can result in complications later. It's crucial to specify if there is any other insurer involved and to provide relevant details. This information helps Aetna manage claims accurately in coordination with any other insurance benefits.
Inaccurate or incomplete information regarding the treatment details can also cause significant delays. Individuals must include a clear description of the provider, the services received, and the diagnosis. If the claim involves specific treatments or medications, it’s imperative to provide complete information, including prescriptions where necessary. Missing these details may lead to follow-up inquiries or delays in claim processing.
Finally, people sometimes neglect to review the claims submission deadlines. Failing to submit the Claim Form within the required 180 days from the treatment date can lead to outright denial of the claim. Keeping track of these deadlines is essential, ensuring claims are submitted promptly to avoid any unnecessary complications.
Avoiding these mistakes can lead to a smoother claims process. By carefully reviewing each section, providing clear and concise information, and monitoring deadlines, individuals can enhance their chances of successful claim approval with Aetna International.
Documents used along the form
The Aetna International Claim Form is a crucial document for members seeking reimbursements for medical services. However, several other forms and documents are commonly used alongside it to ensure a smooth and efficient claims process. Here is a list of those documents, along with brief descriptions of their purposes.
- Itemized Bills and Receipts: These documents detail the services provided by healthcare professionals, including costs and dates of service. They support the claim by providing proof of the expenses incurred.
- Authorization or Referral Letters: For certain treatments, especially specialist care, letters from general practitioners may be necessary. These letters indicate that a referral or authorization for treatment was granted.
- Other Insurance Policy Documentation: If a member has other health insurance coverage, documentation such as a policy summary or benefit details must be submitted. This helps clarify any reimbursements from other carriers.
- Prescription Records: Claims for prescribed medications should include a copy of the prescription from the healthcare provider, verifying that the medications were medically necessary and authorized.
- Accident Report: If the claim involves an accident, a report or statement detailing the circumstances may be needed. This provides context and supports claims for treatments related to injuries.
- Statement of Health Benefits: This statement outlines the health benefits that are covered under the member's policy. It helps in understanding what expenses are eligible for reimbursement.
- Proof of Payment: In instances where receipts are missing or inadequate, proof of payment such as bank statements or credit card receipts may be required to demonstrate that the member paid for the services.
- Claim Appeal Forms: If a claim is denied or underpaid, members may need to fill out an appeal form. This process allows members to contest decisions made regarding their claims.
- Personal Medical Information Forms: Aetna may request additional health information to process certain claims, particularly for long-term treatments or those that require extensive documentation.
- Direct Deposit Authorization Form: For members opting for direct bank transfers for their reimbursements, this form provides the necessary bank details to facilitate the deposit.
Maintaining an organized submission with all relevant documents can significantly enhance the chances of a successful claim process. Members should be diligent about reviewing their policies and ensuring all required elements are included with their Aetna International Claim Form for efficient processing.
Similar forms
- Health Insurance Claim Form: Similar to the Aetna International Claim form, this document requires information such as the claimant's details, patient information, and specifics regarding the medical services received. Both forms necessitate itemized bills and receipts.
- Workers' Compensation Claim Form: This form focuses on services related to workplace injuries. Like the Aetna form, it requires detailed treatment information and a declaration confirming the truthfulness of the provided data.
- Medicare Claim Form (CMS-1500): This form is utilized for various health insurance claims. Both forms share the requirement for the patient's insurance details and medical service descriptions. Timeliness in submission is also emphasized.
- Travel Insurance Claim Form: This document requires details about medical treatment received during travel. The necessity for supporting documents and clear details on services is a commonality with the Aetna form.
- Auto Insurance Medical Claim Form: This form is used for medical expenses arising from vehicular accidents. Similarities include the need for accident details and a comprehensive breakdown of medical services received.
- Dental Insurance Claim Form: Just like the Aetna form, this document requests patient and provider information as well as detailed service descriptions. Both documents stress the importance of submitting itemized bills.
- Short-Term Disability Claim Form: This form requires information about medical treatment supporting a disability claim. The need for accurate completion and the provision of relevant medical documentation mirrors the expectations of the Aetna form.
- Supplemental Insurance Claim Form: This form assists in supplementing health claims already submitted to primary carriers. Similar to the Aetna International Claim form, it entails the inclusion of prior insurance coverage details and treatment descriptions.
Dos and Don'ts
When filling out the Aetna International Claim form, follow these important guidelines to ensure a smooth process.
- Do ensure all sections are completed. Every section of the form needs to be filled out completely.
- Do tape small receipts to a full-size sheet of paper. This prevents loss and makes everything easier to review.
- Do submit your claim within 180 days of the treatment date. Timeliness is crucial for smooth processing.
- Do provide detailed information for any treatments received. Include diagnosis, medical provider details, and relevant history.
- Don't leave out any required documents. Missing information can cause delays in processing.
- Don’t forget to keep a copy of your completed claim form. This is essential for your records.
Misconceptions
Here are some common misconceptions about the Aetna International Claim form. Understanding these can help ensure a smoother claims process.
- Only one claim form is needed for the entire family. Each family member must have a separate claim form. This means that if multiple family members seek treatment, you will need to submit distinct forms for each one.
- Receipt documentation isn't necessary. You must provide itemized bills and receipts along with the claim form. This documentation is crucial for processing your claim accurately and efficiently.
- It's fine to submit the claim anytime after treatment. In fact, you must return the completed claim form within 180 days of the treatment date. Missing this deadline could result in denial of the claim.
- All information is optional and can be left blank if not applicable. It’s important to fill out every section that pertains to your claim. Incomplete forms may cause processing delays.
- Submitting a claim means Aetna admits liability. The submission of a claim does not indicate acceptance of liability. Aetna reviews each claim based on the provided documentation.
- Payment methods are fixed and cannot be changed. You can choose between various reimbursement methods. Options include a bank transfer or receiving a cheque, depending on what suits you best.
By clearing up these misconceptions, members can take action to ensure that their claims are processed without unnecessary delays.
Key takeaways
When filling out the Aetna International Claim Form, keep these key takeaways in mind:
- One Claim Form per Family Member: You need a separate form for each family member claiming for treatment.
- Complete All Sections: Every section must be fully filled out to avoid delays in processing your claim.
- Submission Deadlines: Ensure you submit the claim form within 180 days of the treatment date.
- Itemized Bills Required: Attach itemized bills and receipts, taping small receipts to a full sheet of paper for clarity.
- Additional Documentation: Provide relevant documents if you have other insurance that will cover part of your claim.
- Payment Method Choices: Select your preference for how you want to receive reimbursements, either through bank transfer or cheque.
- Declaration of Truthfulness: Sign the declaration to confirm that all provided information is accurate and complete.
- Accident Details: If your claim involves an accident, include all pertinent details about the incident.
- Preferred Payment Currency: Indicate your preferred currency for the reimbursement; otherwise, it will default to US dollars.
- Retain a Copy: Keep a copy of the completed claim form for your records before submission.
By following these steps, you can help ensure a smoother claim process with Aetna International.
Browse Other Templates
Dd Form 2492 - The form requires basic personal information, including name and Social Security number.
Huntington Bank Direct Deposit - Avoid delays by including a voided check with your enrollment form.
Casper College Transcripts - Double-check that your full address is written clearly on the request form.