Fill Out Your Aetna Validation Form
The Aetna Validation form is an essential tool for anyone looking to establish new business cases with Aetna U.S. Healthcare. This form must be submitted with all new cases, and it’s crucial to get it in 30 days prior to the proposed effective date to ensure that beneficiaries receive their ID cards on time. Proper completion of the form not only accelerates processing but also prevents unnecessary delays. The form requires detailed information about the case, including the case name, submission date, effective date, and contact details for the producer and any assistants. It also collects vital documentation, such as the employer master application, employee applications, and verification forms signed by the employer. To accurately assess eligibility and coverage options, it asks about existing group coverage, prior insurance carriers, and employee enrollment statistics. Additional requirements include a binder check and signatures, underscoring the importance of thoroughness. Each piece of data submitted helps Aetna ensure that clients receive tailored plans and that all necessary steps are taken to build a solid foundation for new health coverage. Following the guidelines laid out in this form ensures smoother processing and a better experience for everyone involved.
Aetna Validation Example
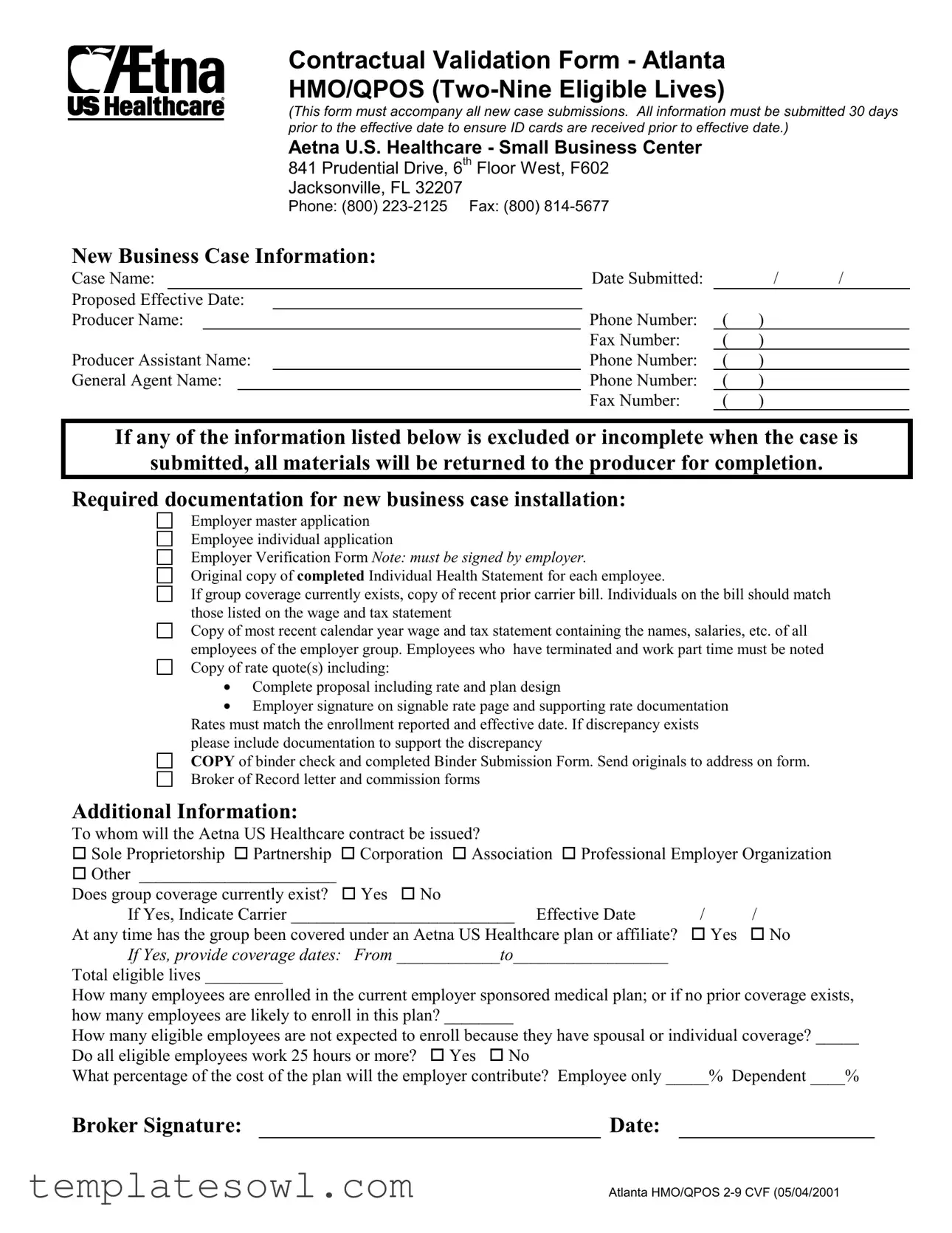
Contractual Validation Form - Atlanta
HMO/QPOS
(This form must accompany all new case submissions. All information must be submitted 30 days prior to the effective date to ensure ID cards are received prior to effective date.)
Aetna U.S. Healthcare - Small Business Center
841 PRUDENTIAL DRIVE, 6TH FLOOR WEST, F602 JACKSONVILLE, FL 32207
PHONE: (800)
New Business Case Information:
Case Name: |
|
Date Submitted: |
|
/ |
/ |
||||
Proposed Effective Date: |
|
|
|
|
|
||||
Producer Name: |
Phone Number: |
( |
) |
|
|||||
|
|
|
|
|
|
Fax Number: |
( |
) |
|
Producer Assistant Name: |
|
|
Phone Number: |
( |
) |
|
|||
General Agent Name: |
Phone Number: |
( |
) |
|
|||||
|
|
|
|
|
|
Fax Number: |
( |
) |
|
If any of the information listed below is excluded or incomplete when the case is
submitted, all materials will be returned to the producer for completion.
Required documentation for new business case installation:
Employer master application
Employee individual application
Employer Verification Form Note: must be signed by employer.
Original copy of completed Individual Health Statement for each employee.
If group coverage currently exists, copy of recent prior carrier bill. Individuals on the bill should match those listed on the wage and tax statement
Copy of most recent calendar year wage and tax statement containing the names, salaries, etc. of all employees of the employer group. Employees who have terminated and work part time must be noted Copy of rate quote(s) including:
•Complete proposal including rate and plan design
•Employer signature on signable rate page and supporting rate documentation Rates must match the enrollment reported and effective date. If discrepancy exists please include documentation to support the discrepancy
COPY of binder check and completed Binder Submission Form. Send originals to address on form.
Broker of Record letter and commission forms
Additional Information:
To whom will the Aetna US Healthcare contract be issued? |
|
|
|
oSole Proprietorship oPartnership |
oCorporation oAssociation oProfessional Employer Organization |
||
oOther _______________________ |
|
|
|
Does group coverage currently exist? |
oYes oNo |
|
|
If Yes, Indicate Carrier __________________________ Effective Date |
/ |
/ |
|
At any time has the group been covered under an Aetna US Healthcare plan or affiliate? |
oYes |
oNo |
|
If Yes, provide coverage dates: From ____________to__________________ |
|
|
|
Total eligible lives _________ |
|
|
|
How many employees are enrolled in the current employer sponsored medical plan; or if no prior coverage exists, how many employees are likely to enroll in this plan? ________
How many eligible employees are not expected to enroll because they have spousal or individual coverage? _____
Do all eligible employees work 25 hours or more? oYes oNo
What percentage of the cost of the plan will the employer contribute? Employee only _____% Dependent ____%
Broker Signature: |
|
Date: |
ATLANTA HMO/QPOS
Form Characteristics
| Fact Name | Description |
|---|---|
| Submission Requirement | The Aetna Validation form must be submitted alongside all new case submissions at least 30 days before the proposed effective date to ensure ID cards are received on time. |
| Contact Information | All submissions should be directed to the Aetna U.S. Healthcare Small Business Center located at 841 Prudential Drive, 6th Floor West, F602, Jacksonville, FL 32207. The contact number is (800) 223-2125. |
| Documentation Requirements | Incomplete submissions will result in returning materials to the producer. Required documents include the employer master application, individual health statements, and prior carrier bills, among others. |
| Eligibility Criteria | The form is designed for groups with 2 to 9 eligible lives. Specific eligibility requirements must be met, including employee hours and employer contribution percentages. |
Guidelines on Utilizing Aetna Validation
Once you have gathered all necessary documents, you can fill out the Aetna Validation form. It is crucial to ensure all information is accurate. Missing or incorrect information may lead to delays. Therefore, proceed carefully and methodically.
- Begin by entering the Case Name in the appropriate field.
- Next, fill in the Date Submitted using the format / / .
- Then indicate the Proposed Effective Date in the same date format.
- Complete the Producer Name field with the relevant contact's name.
- Provide the Phone Number and Fax Number of the producer.
- Continue with the Producer Assistant Name and include their Phone Number.
- Fill out the General Agent Name along with their Phone Number and Fax Number.
- Ensure you have all Required Documentation listed in the instructions, gathering each necessary document:
- Employer master application
- Employee individual application
- Employer Verification Form
- Original copy of completed Individual Health Statement for each employee
- Copy of recent prior carrier bill (if group coverage exists)
- Copy of most recent calendar year wage and tax statement
- Copy of rate quote(s)
- COPY of binder check and completed Binder Submission Form
- Broker of Record letter and commission forms
- Indicate to whom the Aetna US Healthcare contract will be issued by selecting the appropriate option (Sole Proprietorship, Partnership, Corporation, etc.).
- Answer whether group coverage currently exists and specify the carrier, if applicable.
- Provide the effective date of existing group coverage, if relevant.
- Indicate if the group has ever been covered under an Aetna US Healthcare plan or affiliate with coverage dates.
- State the total eligible lives in the group.
- Indicate how many employees are enrolled or are likely to enroll in the plan.
- Specify how many eligible employees will not enroll due to other coverage.
- Confirm if all eligible employees work 25 hours or more by selecting Yes or No.
- Lastly, indicate the percentage of the cost of the plan that the employer will contribute for both employee only and dependent coverage.
- Sign the form where indicated and enter the date.
Double-check all entries for accuracy and completeness before submitting the form to the address specified at the top. This attention to detail helps ensure a smooth processing of your case.
What You Should Know About This Form
What is the purpose of the Aetna Validation Form?
The Aetna Validation Form is essential for the smooth processing of new business case submissions. It ensures that all necessary details and documentation are collected, submitted correctly, and received in a timely manner. Completing this form accurately helps facilitate the issuance of ID cards before the effective date of coverage.
When should the Aetna Validation Form be submitted?
This form must be submitted at least 30 days prior to the proposed effective date of coverage. Timely submission allows adequate time for processing and ensures that all ID cards are distributed before the coverage begins, minimizing any disruptions for employees.
What information is required to complete the Aetna Validation Form?
The form requires a variety of details, including the case name, date submitted, proposed effective date, and contact information for the producer and any assistants. Additionally, required documentation such as the employer master application, employee individual applications, and relevant financial statements must accompany the submission.
What happens if the form is incomplete or inaccurate?
If any part of the form or the required documentation is missing or incorrect, the materials will be returned to the producer for completion. This can delay the entire submission process, potentially pushing back the effective date of coverage.
What documentation must accompany the Aetna Validation Form?
A complete submission should include the employer master application, completed individual health statements for each employee, a signed Employer Verification Form, and copies of relevant financial documents such as wage and tax statements. Additionally, if there is existing group coverage, recent prior carrier bills need to be provided for validation.
Can the Aetna Validation Form be submitted for groups with existing coverage?
Yes, the form can be submitted for groups with existing coverage. In fact, it is important to indicate any current coverage and provide details about the existing carrier and effective dates. This information helps Aetna assess the new coverage accordingly.
Is a Broker of Record letter necessary for submission?
Yes, a Broker of Record letter is required, along with any commission forms, to establish authorization and ensure that all parties involved receive appropriate acknowledgment and compensation for their roles in the business case submission.
What should be done if discrepancies arise in enrollment numbers?
If there is a discrepancy between the reported enrollment numbers and the submitted information, supporting documentation must be provided to justify these differences. It is crucial to clarify and resolve any inconsistencies to avoid delays or complications.
How can I contact Aetna for assistance with the validation form?
If assistance is needed, you can reach Aetna directly through their designated phone line at (800) 223-2125. Additionally, fax communications can be sent to (800) 814-5677 for queries or submission of accompanying documentation.
Common mistakes
Filling out the Aetna Validation form can be straightforward, but many people make common mistakes that can lead to delays or complications. One frequent error is leaving out required information. Each section demands specific details, such as the case name and proposed effective date. Omitting any of this information may result in the entire form being returned for completion. Ensure that all required fields are filled in completely before submission.
Another common mistake is not checking the accuracy of the documentation being submitted. Do not forget to include essential documents like the Employer Verification Form and the completed Individual Health Statement for each employee. It's important to verify that the individuals listed match those on the wage and tax statement. If there are discrepancies, such as mismatched names or missing prior carrier bills, this could also hold up the processing of the case.
Many people also fail to pay attention to the deadlines outlined in the form. The submission must occur 30 days before the proposed effective date to receive ID cards on time. Procrastinating could mean that the information is not processed quickly enough, causing unnecessary stress and complications for everyone involved.
Lastly, ensuring clarity in communication is vital. When completing the form, use clear and concise language. Avoid abbreviations or ambiguous terms that could confuse the reviewers. Each response should be easily understandable to avoid misinterpretations that could lead to delays. Paying attention to these details can streamline the process and ensure a smoother experience.
Documents used along the form
The Aetna Validation form is essential for processing new business cases with Aetna. However, several other documents accompany this form, each playing a critical role in ensuring a smooth submission and approval process. Below is a list of these documents, which are often required when submitting your application.
- Employer Master Application: This comprehensive application collects information about the employer and the desired health plan options for employees. It is a foundational document that must be completed accurately.
- Employee Individual Application: Each employee needs to fill out this application to provide personal details and benefit preferences. It ensures that all individuals covered under the plan are properly registered.
- Employer Verification Form: This document serves as proof that the employer is legally operating and should be signed by the employer to validate the application.
- Individual Health Statements: For every employee, an original Individual Health Statement is required. This document discloses health information necessary for underwriting the insurance coverage.
- Prior Carrier Bill: If group coverage was previously in place, a copy of the most recent bill is needed. This helps Aetna verify current members and their coverage status.
- Wage and Tax Statement: This statement outlines the financial details of the employer's workforce. It must reflect all employees, including part-time workers, ensuring accurate enrollment and premium calculations.
- Rate Quotes: This includes a complete proposal with rates, plan design, and employer signatures, ensuring all parties agree on terms before proceeding.
- Binder Check and Binder Submission Form: A check is needed to secure the initial coverage period. This document indicates payment and confirms intent to enroll.
- Broker of Record Letter and Commission Forms: This establishes the broker's authority to manage the case and outlines the commission structure for their services.
Completing this list of documents thoroughly and submitting them on time is crucial. Any missing or incorrect information can result in delays or rejections of your application. Make sure to gather all necessary paperwork before moving forward with your submission.
Similar forms
The Aetna Validation Form is an essential document for ensuring compliance and accuracy in submitting new business cases. Several other documents share similarities with it in their purpose and the information they require. Below are five documents that are comparable to the Aetna Validation Form:
- Employer Master Application: This form often accompanies new group insurance submissions. Like the Aetna Validation Form, it requires comprehensive details regarding the employer, employees, and proposed coverage. Both documents emphasize accuracy and completeness to avoid delays in processing.
- Employee Individual Application: Similar in structure, the Employee Individual Application gathers personal and health information from each employee who will be covered under the plan. It aligns with the Aetna Validation form by ensuring that all necessary individual data is collected to facilitate group coverage approval.
- Employer Verification Form: This document verifies the legitimacy of the employer and usually requires the employer's signature. Like the Aetna Validation Form, it aims to assure that only valid entities are entering into a healthcare agreement, thus maintaining compliance with insurance regulations.
- Binder Submission Form: This form is crucial in finalizing the submission of all required documentation and often includes a check for the initial premium. Similar to the Aetna Validation Form, the Binder Submission Form must be completed accurately and sent to the same designated location to ensure timely processing.
- Broker of Record Letter: This letter designates the broker responsible for the group’s insurance case. Like the Aetna Validation Form, it includes necessary endorsements and signatures, reinforcing relationships between all parties involved—employer, employees, and brokers—and ensuring everyone is on the same page regarding representation.
Dos and Don'ts
When filling out the Aetna Validation form, it’s important to get everything right. Here’s a helpful list of what to do and what to avoid.
- Do submit the form at least 30 days before the effective date.
- Do ensure all required documentation is included with your submission.
- Do check that all information provided is complete and accurate.
- Do provide the original copy of all necessary forms and statements.
- Don’t submit the form without verifying all signatures are included and valid.
- Don’t forget to match rates with the enrollment reported and effective date.
- Don’t assume any information is understood; clarity is essential to avoid delays.
By following these guidelines, you can help ensure that your submission goes smoothly, reducing the chances of returning for further information.
Misconceptions
Misconceptions about the Aetna Validation form can lead to confusion and delays in the process. Here are ten common misunderstandings:
- The form can be submitted at any time. Many believe that the Aetna Validation form can be submitted whenever it is convenient. However, it must be submitted a minimum of 30 days prior to the proposed effective date to ensure that ID cards are received on time.
- All information is optional. Some individuals think that submitting incomplete information is acceptable. This is incorrect; if any required information is missing, the materials will be returned for completion.
- Only the employer's application is necessary. The misconception exists that only the employer master application is required. In fact, multiple documents, including individual applications and tax statements, are necessary for proper processing.
- The form can be faxed with incomplete documents. It is often believed that incomplete submissions can be sent via fax. However, the original documents must be sent to the designated address to ensure proper handling.
- Providing a copy of prior carrier bills is optional. Some think that submitting a recent prior carrier bill is not mandatory. This is incorrect; it is necessary for validating the current coverage status.
- The employer's signature is not required for submission. A common misunderstanding is that the employer's signature on the rate page is not needed. This signature is crucial as it validates the submitted rate and proposal.
- The form is the same for all types of businesses. Individuals may believe that one version of the form works for every business structure. However, different types of entities, such as sole proprietorships or partnerships, require tailored information.
- Eligibility for coverage can be assessed at a later date. Some may think that eligibility details can be decided after form submission. Accurate enrollment details should be provided upfront to avoid complications.
- Emailing the form is an acceptable alternative to mailing it. There is a misconception that emailing the completed form suffices. However, originals must be mailed to the specified address for processing.
- The use of the form is limited to new cases only. Some individuals assume that the form is relevant only for new applications. In reality, it can also be used for certain updates to existing plans under specific circumstances.
Key takeaways
When using the Aetna Validation form, keep these key takeaways in mind:
- The form must accompany all new case submissions.
- Submit all information at least 30 days before the effective date.
- Ensure all required documentation is included to avoid delays.
- Check for accuracy to prevent the return of materials for completion.
- Include a signed Employer Verification Form.
- Provide original copies of necessary applications and statements.
Browse Other Templates
New Connection - All payments related to the application should be made at authorized banks only.
Alabama Child Support Modification Forms - Intentional inaccuracies in the form can lead to serious legal consequences.
Nj License Fee - Failure to comply with the terms could lead to civil liabilities or penalties under the law.