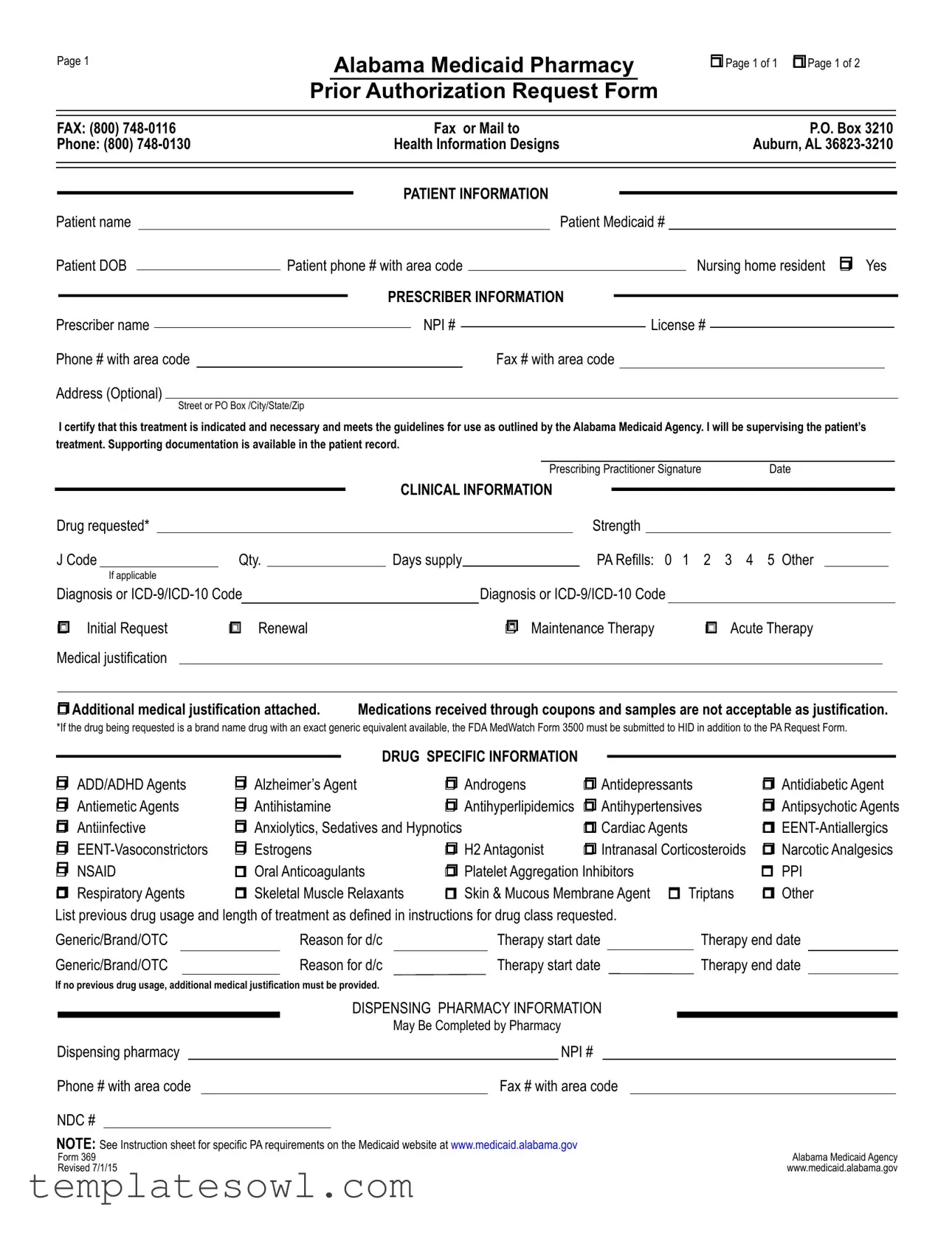
Fill Out Your Alabama 369 Form
The Alabama 369 form serves as a crucial tool for healthcare providers seeking prior authorization for medications through Alabama Medicaid. This form captures essential patient information, including details like the patient's name, date of birth, and Medicaid number. It also includes the prescriber’s information, ensuring that a qualified healthcare professional oversees the treatment process. Within the form, prescribers must clarify the specific drug requested, its strength, and appropriate diagnosis codes. It outlines whether the request is an initial or renewal application, and it requires accompanying medical justification to support the necessity of the requested therapy. The form is specifically designed to address various drug categories, from antipsychotics to antihistamines, each with distinct requirements. The background of treatment, potential alternative therapies, and any previous medication history also play a significant role in the authorization process, illustrating the thoughtful consideration needed for responsible medication management. Importantly, additional sections address unique patient circumstances, such as substance abuse history and special considerations for pediatric patients, underscoring the importance of crafting a comprehensive medication management plan.
Alabama 369 Example
Page 1
Alabama Medicaid Pharmacy
Prior Authorization Request Form
rPage 1 of 1 r Page 1 of 2
FAX: (800) |
|
|
|
Fax or Mail to |
|
|
|
|
P.O. Box 3210 |
|
|||||||||||||
Phone: (800) |
|
|
Health Information Designs |
|
|
|
|
Auburn, AL |
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PATIENT INFORMATION |
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
Patient name |
|
|
|
|
|
|
|
|
Patient Medicaid # |
|
|
||||||||||||
Patient DOB |
|
|
Patient phone # with area code |
|
|
|
|
Nursing home resident r Yes |
|
||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
PRESCRIBER INFORMATION |
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
Prescriber name |
|
|
|
|
|
|
NPI # |
|
|
|
|
License # |
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
Phone # with area code |
|
|
|
|
|
|
Fax # with area code |
|
|
|
|
|
|
|
|
||||||||
Address (Optional) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
I certify that this treatment is indicated and necessary and meets the guidelines for use as outlined by the Alabama Medicaid Agency. I will be supervising the patient’s treatment. Supporting documentation is available in the patient record.
|
|
|
|
|
|
|
|
|
|
|
|
|
Prescribing Practitioner Signature |
Date |
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CLINICAL INFORMATION |
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
Drug requested* |
|
|
|
|
|
|
|
|
|
|
|
Strength |
|
|
|
|
|
|
|
||||
|
J Code |
Qty. |
|
Days supply |
|
|
|
PA Refills: 0 1 |
2 3 4 5 Other |
|
||||||||||||||
|
|
If applicable |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Diagnosis or |
|
|
|
Diagnosis or |
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
r Initial Request |
r Renewal |
|
|
|
r |
Maintenance Therapy |
r Acute Therapy |
|
|||||||||||||||
|
Medical justification |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
r Additional medical justification attached. |
Medications received through coupons and samples are not acceptable as justification. |
|
|||||||||||||||||||||
*If the drug being requested is a brand name drug with an exact generic equivalent available, the FDA MedWatch Form 3500 must be submitted to HID in addition to the PA Request Form.
|
|
|
|
|
|
|
|
|
|
DRUG SPECIFIC INFORMATION |
|
|
|
|
|
|
|
|
|
|
|
||
r ADD/ADHD Agents |
r Alzheimer’s Agent |
r Androgens |
r Antidepressants |
r Antidiabetic Agent |
|||
r Antiemetic Agents |
r Antihistamine |
r Antihyperlipidemics |
r Antihypertensives |
r Antipsychotic Agents |
|||
r Antiinfective |
r Anxiolytics, Sedatives and Hypnotics |
r Cardiac Agents |
r |
||||
r |
r Estrogens |
r H2 Antagonist |
r Intranasal Corticosteroids |
r Narcotic Analgesics |
|||
r NSAID |
r Oral Anticoagulants |
r Platelet Aggregation Inhibitors |
r PPI |
||||
r Respiratory Agents |
r Skeletal Muscle Relaxants |
r Skin & Mucous Membrane Agent r Triptans |
r Other |
||||
List previous drug usage and length of treatment as defined in instructions for drug class requested. |
|
|
|
|
||||||||||||||
Generic/Brand/OTC |
|
Reason for d/c |
|
Therapy start date |
|
|
Therapy end date |
|
||||||||||
Generic/Brand/OTC |
|
Reason for d/c |
|
Therapy start date |
|
Therapy end date |
|
|||||||||||
If no previous drug usage, additional medical justification must be provided. |
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DISPENSING PHARMACY INFORMATION |
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
May Be Completed by Pharmacy |
|
|
|
|
|||||
Dispensing pharmacy |
|
|
|
|
|
NPI # |
|
|
|
|
|
|||||||
Phone # with area code |
|
|
|
|
Fax # with area code |
|
|
|
|
|
||||||||
NDC # |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
NOTE: See Instruction sheet for specific PA requirements on the Medicaid website at www.medicaid.alabama.gov |
|
Alabama Medicaid Agency |
||||||||||||||||
Form 369 |
|
|
|
|
|
|
|
|
|
|||||||||
Revised 7/1/15 |
|
|
|
|
|
|
|
|
|
www.medicaid.alabama.gov |
||||||||

Page 2 |
Patient Medicaid # |
rSustained Release Oral Opioid Agonist
Proposed duration of therapy |
|
|
|
|
Is medicine for PRN use? |
r Yes |
r No |
|
|||
Type of pain r Acute r Chronic |
|
|
|
Severity of pain: r Mild |
r Moderate r Severe |
|
|||||
Is there a history of substance abuse or addiction? r Yes |
r No |
|
|
|
|||||||
If yes, is treatment plan attached? |
r Yes r No |
|
|
|
|
|
|
|
|
||
Indicate prior and/or current analgesic therapy and alternative management choices |
|
|
|
||||||||
Drug/therapy |
|
|
|
|
Reason for d/c |
|
|
|
|
|
|
Drug/therapy |
|
|
|
Reason for d/c |
|
|
|
|
|||
|
|
|
|
|
|||||||
r Antipsychotic Agents |
The request is for: |
r Monotherapy or r Polytherapy |
|
|
|||||||
For children < 6 years of age, have monitoring protocols (see Attachment C on the Alabama Medicaid website) been followed? r Yes r No For polytherapy and/or
Medical justification may include peer reviewed literature, medical record documentation, chart notes with specific symptoms that the support the diagnosis, etc.
rXenicalR
r |
If initial request |
Weight |
|
kg. |
|
Height |
|
inches |
BMI |
|
|
kg/m2 |
|||
r |
If renewal request |
Previous weight |
|
|
|
kg. |
Current weight |
|
|
|
kg. |
|
|
||
Documentation MD supervised exercise/diet regimen > 6 mo.? r Yes |
r No |
Planned adjunctive therapy? r Yes |
r No |
||||||||||||
r Phosphodiesterase Inhibitors |
|
|
|
|
|
|
|
|
||
Failure or inadequate response to the following alternate therapies: |
|
|
|
|
|
|||||
1. |
|
|
|
2. |
|
|
3. |
|
|
|
4. |
|
|
|
5. |
|
|
6. |
|
|
|
Contraindication of alternate therapies: |
|
|
|
|
|
|
|
|
||
r Documentation of vasoreactivity test attached |
r Consultation with specialist attached |
|
|
|||||||
|
|
|
|
|
|
|||||
r Specialized Nutritionals |
Height |
inches |
Current weight |
kg. |
|
|||||
rIf < 21 years of age, record supports that > 50% of need is met by specialized nutrition
rIf > 21 years of age, record supports 100% of need is met by specialized nutrition
Method of administration |
|
Duration |
|
|
|
|
# of refills |
|||
|
|
|
|
|
|
|
|
|
|
|
r Xolair® |
Current Weight:__________kg (patient’s weight must be between |
|||||||||
Is the patient 12 years or older? |
|
|
|
r |
Yes |
r |
No |
|||
Is the request for chronic idiopathic urticaria? |
r |
Yes |
r |
No |
||||||
Is the request for moderate to severe asthma and is treatment recommended by a board |
|
|
|
|
|
|
|
|||
certified pulmonologist or allergist after their evaluation (if yes answers questions below)? |
r |
Yes |
r |
No |
||||||
Has the patient had a positive skin or blood test reaction to a perennial aeroallergen? |
r |
Yes |
r |
No |
||||||
Is the patient symptomatic despite receiving a combination of either inhaled corticosteroid |
|
|
|
|
|
|
|
|||
and a leukotriene inhibitor or an inhaled corticosteroid and long acting beta agonist or has |
|
|
|
|
|
|
|
|||
the patient required 3 or more bursts of oral steroids within the past 12 months? |
r |
Yes |
r |
No |
||||||
Are the patient’s baseline IgE levels between 30 IU/mL and 700 IU/mL? |
r |
Yes |
r |
No |
||||||
Level:_________________ |
Date:__________________ |
|
|
|
|
|
|
|
||
Form 369 |
Alabama Medicaid Agency |
Revised |
www.medicaid.alabama.gov |
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | The Alabama 369 form is used to request prior authorization from Alabama Medicaid for specific medications, ensuring that they are medically necessary for the patient. |
| Governing Law | The use of the Alabama 369 form is governed by Medicaid regulations under the Alabama Medicaid Agency. |
| Documentation Requirement | Along with the submission, medical justification documentation must be provided, especially for off-label uses or polytherapy requests. |
| Pharmacy Information | The form allows pharmacies to complete specific sections, such as providing their NPI number, which is necessary for processing the request. |
| Substance Abuse History | There is a requirement to disclose any history of substance abuse or addiction, which is crucial for assessing the patient's current treatment plan. |
| Initial and Renewal Requests | The form differentiates between initial requests, renewals, and maintenance therapies, each having specific criteria that must be met for approval. |
Guidelines on Utilizing Alabama 369
Completing the Alabama 369 form involves providing specific patient and prescriber information, along with details about the drug being requested and any clinical justification. The steps below outline the process for accurately filling out this form in order for it to be processed efficiently.
- Begin by entering the patient information:
- Fill in the patient’s name.
- Enter the patient’s Medicaid number.
- Provide the patient's date of birth (DOB).
- Include the patient's phone number with area code.
- Indicate if the patient is a nursing home resident by checking 'Yes' or 'No.'
- Provide prescriber information:
- Enter the prescriber’s name.
- Fill in the National Provider Identifier (NPI) number.
- Include the license number.
- Provide the prescriber’s phone number with area code.
- Optionally, include the prescriber’s fax number and address.
- Sign and date the form where indicated for the prescriber certification.
- Complete the clinical information section, specifying:
- The drug being requested.
- The strength of the drug.
- The J Code.
- The quantity and days supply.
- The number of refills requested.
- Indicate the purpose of the request: Initial, Renewal, Maintenance, or Acute therapy.
- List any applicable diagnosis codes (ICD-9/ICD-10) associated with the request and any medical justification for therapy if needed.
- If the drug falls under a specific category (like ADD/ADHD agents, antipsychotic agents, etc.), check the appropriate box.
- If there is any previous drug usage, document that history, including reasons for discontinuation, therapy start and end dates.
- Enter dispensing pharmacy information including the pharmacy NPI number and contact information, if applicable.
- Complete the drug-specific details, confirming if the medicine is for PRN use, specifying pain type and severity, and indicating any history of substance abuse.
- If applicable, provide information regarding any additional required supporting documentation indicated within the form sections.
Once the form is filled out completely, it should be faxed to the appropriate number or mailed to the designated address for processing. Ensuring accurate entries will contribute to a smoother review and approval process.
What You Should Know About This Form
What is the Alabama 369 form?
The Alabama 369 form, also known as the Pharmacy Prior Authorization Request Form, is used to request prior approval from Alabama Medicaid for specific medications. This form ensures that prescribed treatments meet the necessary criteria set by the Alabama Medicaid Agency before being dispensed to patients.
Who needs to fill out the Alabama 369 form?
The prescriber, who is often a healthcare provider such as a doctor or nurse practitioner, needs to complete the form. The information provided will help justify the medical necessity of the requested medication for the patient.
What information is required on the form?
The form collects both patient and prescriber information, including names, Medicaid numbers, and contact details. It also requires details about the requested medication, its strength, quantity, and the diagnosis codes (ICD-9 or ICD-10) related to the patient's condition.
Can the Alabama 369 form be used for medication renewals?
Yes, the form has options for initial requests as well as renewals. It allows healthcare providers to indicate whether they are requesting a refill for a patient’s ongoing therapy or if it is a new treatment.
What if the medication requested is a brand name drug that has a generic equivalent?
If the requested medication is a brand name drug with a generic equivalent, the prescriber must submit the FDA MedWatch Form 3500 along with the Alabama 369 form. This step is crucial for compliance with Medicaid guidelines.
Where should the completed Alabama 369 form be sent?
The completed form can be faxed to (800) 748-0116 or mailed to P.O. Box 3210, Auburn, AL 36823-3210. Both methods are accepted by Health Information Designs, the entity that processes these requests for Alabama Medicaid.
How long does it take to receive a decision on the request?
Decisions typically occur within 24 to 48 hours after the form is submitted. However, additional information may be required, which could extend this timeframe.
What happens if the request is denied?
If Alabama Medicaid denies the prior authorization request, the prescriber will receive notification detailing the reasons. The provider can then either appeal the decision or consider alternative treatment options for the patient.
Are there special considerations for pediatric patients?
Yes, for children under the age of 6 receiving antipsychotic agents, monitoring protocols must be followed as per the guidelines on the Alabama Medicaid website. It’s essential to ensure that prescribed treatments align with specific protocols for this age group.
Common mistakes
Filling out the Alabama Medicaid Pharmacy Prior Authorization Request Form 369 can be challenging. Many individuals make common mistakes that can delay processing and lead to complications. Understanding these errors can help ensure a smoother application process.
One frequent mistake is providing incomplete patient information. Essential details such as the patient's name, Medicaid number, and date of birth need to be clearly filled out. If any of these fields are missing or incorrectly entered, it can result in delays as staff may need to reach out for clarification.
Another common error involves the prescriber information. Failing to enter the prescriber’s name, NPI number, or license number can cause significant issues. Having accurate contact information is crucial not just for verification, but also for effective communication regarding the authorization request.
Many people overlook the importance of providing detailed clinical information. When submitting a request for a specific drug, it’s essential to include the correct drug strength, dosage, and any relevant diagnosis codes. Skipping this could lead to a denial of the request.
Additionally, applicants sometimes forget to indicate whether the request is for an initial, renewal, or maintenance therapy. This detail is crucial for the reviewers, as it impacts the urgency and type of information required for the evaluation.
Another significant mistake is the lack of medical justification and support documentation. If medications have been previously used, a detailed record needs to be provided; simply stating that previous medications were ineffective isn’t sufficient. Failing to include supporting documents can result in the request not being processed.
Moreover, incomplete sections regarding the dispensing pharmacy details can cause delays. Providing the pharmacy name, NPI number, and contact information is vital for fulfillment and communication. Without these, confusion may arise that hinders the authorization process.
Lastly, applicants often neglect to address the specific therapeutic information. This means not adequately clarifying details about previous drug usage, reason for discontinuation, and therapy start and end dates. These sections are necessary for clearly understanding the patient's treatment history and must be accurately completed.
Avoiding these mistakes can streamline the processing of the Alabama Medicaid Pharmacy Prior Authorization Request Form 369. Ensuring all sections are thoroughly completed and correct will help in receiving timely approval for necessary medications.
Documents used along the form
Completing the Alabama Medicaid Pharmacy Prior Authorization Request Form (often referred to as the Alabama 369 form) is just one part of navigating the healthcare system. Additional documentation may be needed to support the PA request and provide a complete picture of the patient's needs. Here are some common forms and documents that often accompany the Alabama 369 form:
- MedWatch Form 3500: This form is necessary when requesting a brand-name drug that has an exact generic equivalent available. It helps report adverse effects or product problems to the FDA.
- Prior Authorization Supporting Documentation: Supplemental information is often required to justify the decision for a specific therapy. This could include clinical notes or additional medical justifications showing the need for treatment.
- Consultation Reports: If a specialist's opinion is needed, the report from the consultation should be attached. It may contain valuable insights that support the prescribed treatment.
- Drug Utilization Review Documents: These documents help identify past drug therapies the patient has tried, their duration, and the reasons for discontinuation. In many cases, they provide essential context for the current therapy request.
- Diagnosis Codes/Clinical Notes: Detailed notes from healthcare providers that outline the patient's diagnosis often accompany the PA request. These are essential for validating the necessity of the medication being requested.
- Substance Abuse Screening Documentation: If there’s a concern regarding a patient’s history of substance abuse, documentation of screening results or treatment plans may need to be included.
- Physical Evaluation Records: These records support the need for treatments based on the patient’s clinical condition and physical health assessment.
- Weight Management Plans: For medications related to weight management, documentation detailing the patient’s diet and exercise regimen may be required.
- Allergy Testing Results: If requesting medications like Xolair, evidence of previous allergy testing is crucial. This includes the test results and interpretations by a qualified allergist.
- Patient-Specific Formulations: For patients requiring specialized nutritional therapies, documentation of clinical assessments supporting the need for those therapies should be included.
These additional documents not only help provide clarity but also enhance the approval chances for the medications requested. It's vital to understand that thorough preparation and precise documentation can significantly impact patient care and access to necessary treatments.
Similar forms
Prior Authorization Request Form: Similar to the Alabama 369 form, this document serves as a formal request for permission from a payer to proceed with a particular treatment or medication. It includes patient details, prescriber information, and a justification for the treatment sought.
Medicare Part D Coverage Determination Request: This document is used to request coverage for prescription medications under Medicare Part D. It requires details about the patient, prescribed medication, and any necessary justification, paralleling the requirements of the Alabama 369 form.
Prescription Drug Prior Authorization Forms: These are documents required by various insurance companies to approve specific medications before they can be dispensed. Like the Alabama 369 form, they collect information about the patient and the prescribed medication along with clinical justification.
Medicaid External Review Request: This form requests an external review of a denied service under Medicaid. It shares similarities with the Alabama 369 as it involves submitting details about the patient and the treatment, along with supporting documents to justify the request.
Medication Exception Request Form: This document is similar in that it is used to request a medication that is not listed in the formulary. It captures essential patient and medication information just like the Alabama 369 form.
Clinical Prior Authorization Forms: These forms are utilized in various healthcare settings to evaluate the medical necessity of treatments. They require clinical information and rationale, resembling the content and purpose of the Alabama 369.
Drug Treatment Authorization Form: This form is used by healthcare providers to authorize treatment with specific drugs. Similar to the Alabama 369, it includes patient information and medical justification supporting the treatment prescribed.
Choice of Provider and Treatment Form: This document is relevant for managing patient care options within Medicaid programs. Details about the patient and selected treatment are documented, much like the format of the Alabama 369.
Veteran’s Health Administration Prescription Request: This request form is used by veterans to obtain prescription medications. It resembles the Alabama 369 in structure, requiring patient, prescriber, and medication details along with justification for the request.
Behavioral Health Treatment Authorization Request: This form is used for obtaining authorization for mental health services. Patient details and clinical justification are akin to those required in the Alabama 369 form.
Dos and Don'ts
When filling out the Alabama 369 form, follow these guidelines carefully.
- Do: Ensure that all patient and prescriber information is complete and accurate.
- Do: Clearly indicate the drug requested and its strength.
- Do: Attach any relevant medical justification documentation if required.
- Do: Double-check for any required additional forms, such as the FDA MedWatch Form 3500 for brand name drugs.
- Don’t: Provide incomplete information; this can delay your request.
- Don’t: Forget to indicate if the patient is a nursing home resident; this information matters.
- Don’t: Use medications received through coupons or samples as justification.
- Don’t: Send the form without verifying all the information is correct and legible.
Misconceptions
The Alabama 369 Form is a critical document used for obtaining prior authorization from Alabama Medicaid for certain medications. However, several misconceptions surround its usage. Here are five common misconceptions, along with clarifications.
- Misconception 1: Only doctors can fill out the form.
- Misconception 2: The form is only needed for brand-name drugs.
- Misconception 3: Submitting the form guarantees approval.
- Misconception 4: Any information can be submitted as medical justification.
- Misconception 5: The form can be submitted without prior drug therapy documentation.
While healthcare providers such as doctors are typically responsible for submitting the form, pharmacists can assist in completing necessary sections. Collaborative care can improve efficiency in the submission process.
The Alabama 369 Form is required for specific medications, including generics under certain circumstances. If there's a generic equivalent available but the prescriber believes the brand name drug is necessary, additional justification must be provided.
Submitting the form does not guarantee that the request will be approved. Approval depends on meeting specific clinical guidelines outlined by Alabama Medicaid. Careful documentation and justification are crucial for a higher likelihood of approval.
Not all information qualifies as medical justification. The justification must be up-to-date, relevant, and aligned with the guidelines specified by Alabama Medicaid. Peer-reviewed literature and thorough medical records often carry more weight.
If the patient has not undergone previous drug therapy, extra medical justification is required. This helps ensure that all appropriate treatment avenues are explored before considering the requested medication.
Key takeaways
When filling out the Alabama 369 form, consider the following key takeaways:
- The form is used for requesting prior authorization for pharmacy services under Alabama Medicaid.
- All patient information, including the Medicaid number and date of birth, must be accurately recorded.
- Make sure to include the prescriber’s details such as their name, NPI number, and contact information.
- Select the correct category for the drug requested, which may include various classes like antidepressants or antipsychotic agents.
- Indicate whether the request is for an initial prescription, renewal, or maintenance therapy.
- Medical justification for the prescribed treatment is required; mere samples or coupons are not acceptable.
- Be mindful of specific requirements for requesting brand-name drugs with available generic alternatives.
- A portion of the form details current and past drug therapy; complete this accurately for a successful submission.
- Additional documentation may be needed if there is no prior drug usage; ensure to attach necessary papers.
- Submit the form via fax or mail to the specified address, maintaining compliance with deadlines.
Browse Other Templates
Can I Buy a House With Bad Credit - The application process allows for checking the status within 30 days.
Kmart Application Form - Know that accurate personal details will streamline your application.