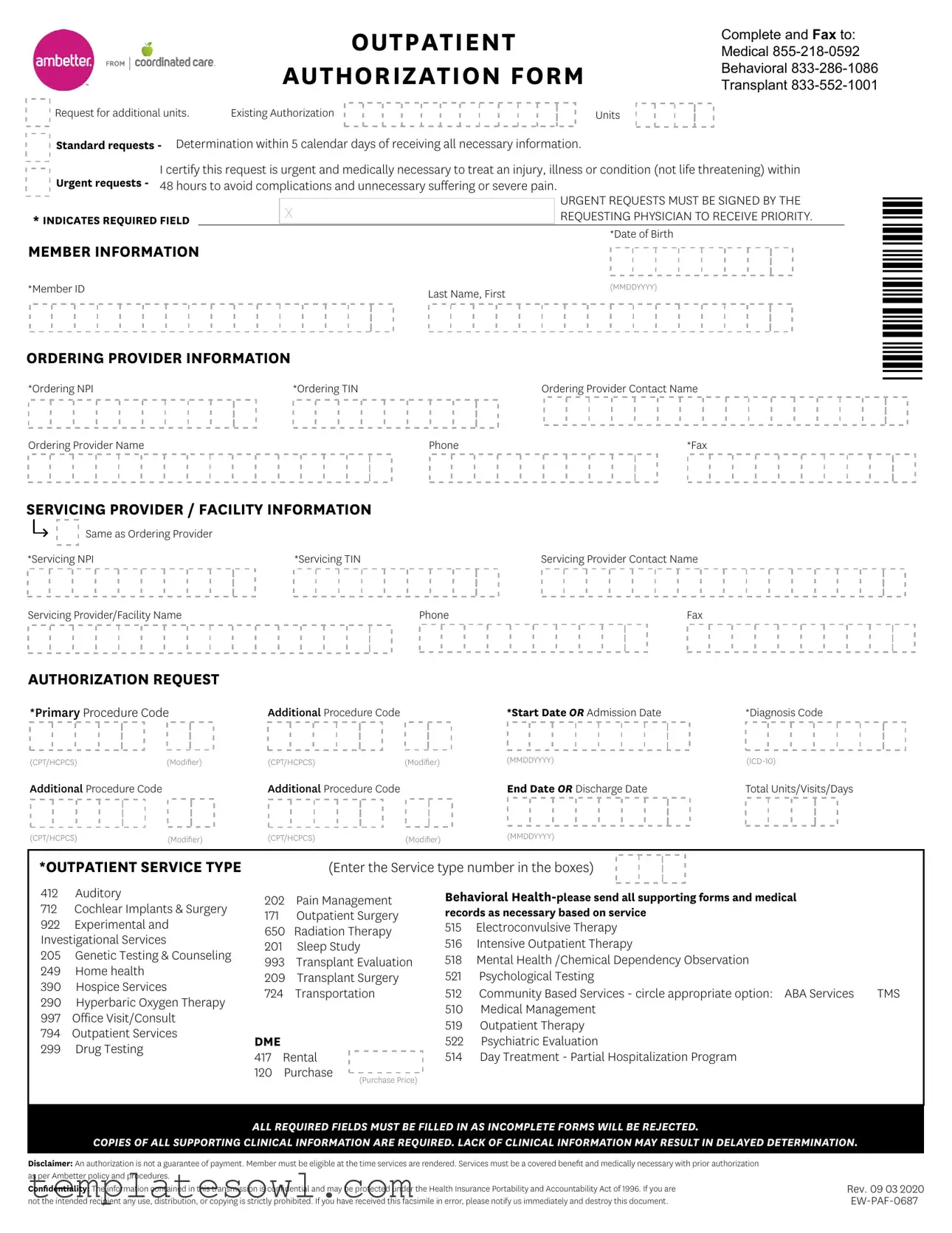
Fill Out Your Ambetter Out Patient Form
The Ambetter Out Patient form serves as a vital tool for healthcare providers seeking authorization for various outpatient services. Designed for efficiency, it includes sections requiring detailed member information such as the Member ID and date of birth. Healthcare providers, both ordering and servicing, must fill out their respective data points, including NPI and TIN numbers, ensuring proper identification and contact information. The form also delineates specific outpatient service types, ranging from behavioral health services to surgical procedures, with corresponding codes that must be accurately entered. Both standard and urgent requests are accommodated, where urgency necessitates a quicker response to avoid complications or severe pain. Additionally, the form emphasizes the importance of complete submissions, as incomplete applications will be rejected, potentially delaying necessary treatments. Clinical information must accompany the request, as the lack of such documentation may further hinder the authorization process. Notably, while the form initiates the approval process, it does not guarantee payment, highlighting the need for eligibility verification at the time of service. Patients and providers alike should be aware of the confidentiality provisions associated with the information contained within the form, as it is protected under federal law.
Ambetter Out Patient Example
OUTPATIENT
AUTHORIZATION FORM
Complete and Fax to: Medical
Request for additional units. |
Existing Authorization |
Units
Standard requests - Determination within 5 calendar days of receiving all necessary information.
Urgent requests - |
I certify this request is urgent and medically necessary to treat an injury, illness or condition (not life threatening) within |
|||||
48 hours to avoid complications and unnecessary suffering or severe pain. |
||||||
|
|
|
|
|
|
URGENT REQUESTS MUST BE SIGNED BY THE |
|
|
|
X |
|
|
|
* INDICATES REQUIRED FIELD |
|
|
|
REQUESTING PHYSICIAN TO RECEIVE PRIORITY. |
||
|
|
|
|
*Date of Birth |
||
MEMBER INFORMATION |
|
|
|
|||
|
|
|
|
|||
*Member ID |
|
|
|
Last Name, First |
|
(MMDDYYYY) |
|
|
|
|
|
|
|
ORDERING PROVIDER INFORMATION |
|
|
|
|||
*Ordering NPI |
|
|
*Ordering TIN |
|
Ordering Provider Contact Name |
|
Ordering Provider Name |
|
|
|
Phone |
|
*Fax |
*0687*
SERVICING PROVIDER / FACILITY INFORMATION
Same as Ordering Provider |
|
|
*Servicing NPI |
*Servicing TIN |
Servicing Provider Contact Name |
Servicing Provider/Facility Name |
Phone |
Fax |
AUTHORIZATION REQUEST
*Primary Procedure Code |
Additional Procedure Code |
|
*Start Date OR Admission Date |
*Diagnosis Code |
|
(CPT/HCPCS) |
(Modifier) |
(CPT/HCPCS) |
(Modifier) |
(MMDDYYYY) |
|
Additional Procedure Code |
|
Additional Procedure Code |
|
End Date OR Discharge Date |
Total Units/Visits/Days |
(CPT/HCPCS) |
(Modifier) |
(CPT/HCPCS) |
(Modifier) |
(MMDDYYYY) |
|
*OUTPATIENT SERVICE TYPE
(Enter the Service type number in the boxes)
412 Auditory
712Cochlear Implants & Surgery
922Experimental and Investigational Services
205Genetic Testing & Counseling
249Home health
390Hospice Services
290Hyperbaric Oxygen Therapy
997Office Visit/Consult
794Outpatient Services
299Drug Testing
202Pain Management
171Outpatient Surgery
650Radiation Therapy
201Sleep Study
993Transplant Evaluation
209Transplant Surgery
724Transportation
DME |
|
|
417 |
Rental |
|
120 |
Purchase |
(Purchase Price) |
|
|
Behavioral
515Electroconvulsive Therapy
516Intensive Outpatient Therapy
518Mental Health /Chemical Dependency Observation
521Psychological Testing
512 |
Community Based Services - circle appropriate option: ABA Services |
TMS |
510 |
Medical Management |
|
519 |
Outpatient Therapy |
|
522 Psychiatric Evaluation |
|
|
514 |
Day Treatment - Partial Hospitalization Program |
|
ALL REQUIRED FIELDS MUST BE FILLED IN AS INCOMPLETE FORMS WILL BE REJECTED.
COPIES OF ALL SUPPORTING CLINICAL INFORMATION ARE REQUIRED. LACK OF CLINICAL INFORMATION MAY RESULT IN DELAYED DETERMINATION.
Disclaimer: An authorization is not a guarantee of payment. Member must be eligible at the time services are rendered. Services must be a covered benefit and medically necessary with prior authorization as per Ambetter policy and procedures.
Confidentiality: The information contained in this transmission is confidential and may be protected under the Health Insurance Portability and Accountability Act of 1996. If you are not the intended recipient any use, distribution, or copying is strictly prohibited. If you have received this facsimile in error, please notify us immediately and destroy this document.
Rev. 09 03 2020
Form Characteristics
| Fact Name | Fact Detail |
|---|---|
| Purpose | The Ambetter Outpatient Authorization Form is used to request authorization for outpatient services, ensuring that the services are covered and medically necessary. |
| Urgent Requests | Urgent requests must be signed by the requesting physician and can be processed within 48 hours if certified as medically necessary to prevent complications. |
| Required Information | All required fields must be completed. Incomplete forms will be rejected and may delay the determination process. |
| Confidentiality | This form contains confidential information protected under HIPAA. Unauthorized use or distribution is strictly prohibited. |
Guidelines on Utilizing Ambetter Out Patient
Completing the Ambetter Out Patient form accurately is essential for a smooth authorization process. Following these steps will help ensure that all necessary information is provided and that the form is submitted correctly.
- Gather all relevant patient information, including the member's ID, last name, first name, and date of birth.
- Fill in the ordering provider details. Include the ordering provider's NPI, TIN, contact name, and phone number. Make sure to provide a fax number as well.
- Specify if the servicing provider is the same as the ordering provider. If not, fill in the servicing provider NPI, TIN, contact name, facility name, phone, and fax.
- List the authorization request details. Include the primary procedure code, additional procedure codes, diagnosis code, start date, end date, and total units or visits required.
- Indicate the outpatient service type by entering the corresponding service type number in the designated boxes.
- Check all fields for completeness. Remember that all required fields must be filled in, as incomplete forms may be rejected.
- Collect any supporting clinical information and ensure that it is ready for fax submission.
- Submit the completed form by faxing it to the appropriate number: Medical 855-218-0592, Behavioral 833-286-1086, or Transplant 833-552-1001.
What You Should Know About This Form
What is the purpose of the Ambetter Outpatient Authorization Form?
The Ambetter Outpatient Authorization Form is used to request prior authorization for outpatient healthcare services. This form ensures that the requested services are covered benefits and medically necessary according to Ambetter policies. It helps providers obtain approval before delivering certain treatments, ensuring that patients receive the appropriate care without unexpected costs.
How do I submit the Ambetter Outpatient Authorization Form?
You can complete the form and fax it to the appropriate number based on the type of service being requested. For medical services, use fax number 855-218-0592. For behavioral health services, the fax number is 833-286-1086. If the authorization is for transplant services, fax to 833-552-1001. Make sure all necessary fields are completed to avoid delays.
What information is required on the form?
The form requires several pieces of information, including the member's full name, date of birth, and member ID. Additionally, you will need details about the ordering provider, such as their NPI and contact information, as well as servicing provider details. Several clinical specifics are also necessary, including procedure codes, diagnosis codes, start or admission dates, and the total number of units or days needed for the service.
What happens if I submit an incomplete form?
Submitting an incomplete form may result in rejection of the authorization request. It is essential to fill out all required fields accurately and provide copies of supporting clinical information. Insufficient information can cause significant delays in processing the request, potentially affecting the patient's care.
How long does it take to get a determination?
The determination time depends on the urgency of the request. Standard requests are typically processed within five calendar days after all necessary information is received. Urgent requests, which must be marked as such and signed by a healthcare provider, are processed within 48 hours to avoid complications or significant pain for the patient.
What does it mean if a request is marked as urgent?
An urgent request is one that is medically necessary but not life-threatening. This means that prompt treatment is needed to prevent complications, unnecessary suffering, or severe pain. It is critical that the healthcare provider certifies the request's urgency to ensure expedited review by Ambetter.
Does authorization guarantee payment for services?
No, obtaining authorization does not guarantee payment. It is essential for the member to be eligible for coverage at the time the services are rendered. The services requested must also align with covered benefits and be determined as medically necessary according to Ambetter's policies.
How should confidential patient information be handled when submitting the form?
Confidentiality is paramount. The information included in the Ambetter Outpatient Authorization Form may be protected under the Health Insurance Portability and Accountability Act (HIPAA). Therefore, it's crucial to ensure that the form is transmitted securely. If the form is received in error, the unauthorized recipient should immediately notify the sender and destroy the document to protect the confidentiality of sensitive patient information.
What if I need help filling out the form?
If assistance is needed when filling out the Ambetter Outpatient Authorization Form, it is advisable to contact Ambetter customer service or consult with the healthcare provider’s administrative office. They can provide guidance on completing the form accurately and ensuring that all necessary information is submitted for a smooth authorization process.
Common mistakes
When filling out the Ambetter Outpatient Authorization Form, several common mistakes can lead to complications or delays in processing. First, individuals often forget to fill in all required fields, marked with an asterisk (*). This can lead to immediate rejection of the form, prolonging the authorization process.
Another mistake is not providing accurate member information. Incorrect details such as the Member ID, date of birth, or last name can cause confusion and may require resubmission of the form. It's essential to double-check that all information aligns with what the insurance provider has on file.
Many also overlook the importance of including all necessary clinical information. Ambetter requires copies of supporting documents for each request. Missing this documentation can result in delayed determinations, which can affect patient care.
Moreover, some individuals mistakenly select the wrong service type. Each outpatient service has a designated code that must be entered correctly. An incorrect code could lead to complications in authorization, should the service be deemed medically necessary.
Errors in coding are another frequent issue. Unfortunately, misidentifying procedure codes, diagnosis codes, or modifiers can lead to improper authorization. Ensure that you review coding guidelines and confirm they are accurate before submission.
Failing to verify the provider’s information is also common. The form requires details for both the ordering and servicing providers, including their National Provider Identifier (NPI) and Tax Identification Number (TIN). Any inaccuracies here may result in delays.
Additionally, people often neglect to sign the form, especially for urgent requests. This signature is crucial for processing the request promptly. Without it, the urgency may not be recognized, leading to standard processing times.
Not adhering to the urgency requirements can lead to serious consequences. If the request is indeed urgent, it is important to clearly state this and provide a brief explanation, ensuring the medical necessity is evident.
Finally, many individuals fail to keep a copy of the submitted form for their records. Retaining documentation is essential for tracking the authorization process and addressing any potential issues that arise.
Documents used along the form
The Ambetter Outpatient Authorization Form is essential for ensuring that outpatient services are approved and covered by insurance. Alongside this form, several other documents may also be necessary for comprehensive patient management and billing. Below is a list of some common forms often used in conjunction with the Ambetter Outpatient Form.
- Ambetter Prior Authorization Request Form: This form is crucial for obtaining pre-approval for specific medical services or medications before they are administered, ensuring that the insurance provider will cover the costs.
- Patient Medical History Form: This document collects a patient's past medical information, which is important for treatment planning and insurance documentation.
- Referral Form: Sometimes required, this form documents a patient's referral from one doctor to another, often necessary for specialists or particular services.
- Insurance Verification Form: This helps confirm a patient's current insurance coverage and benefits, making sure that services will be covered and reducing the risk of unexpected costs.
- Informed Consent Form: This is used to explain the risks and benefits of proposed treatments. It ensures that patients understand what they are agreeing to and provides legal protection for healthcare providers.
- Release of Information Form: This provides permission for healthcare providers to share a patient's medical information with other parties, typically essential for coordinated care.
- Claim Submission Form: After services are rendered, this form is submitted to the insurance company to request payment for covered services, essential for the financial process.
- Behavioral Health Assessment Form: For those seeking behavioral health services, this form helps assess the patient's needs and ensures appropriate referrals and services.
- Billing Statement: This document itemizes the services provided to the patient and details the amounts due, playing a key role in financial transparency.
Each document plays a vital role in the overall process of patient care and billing. By ensuring all necessary forms are completed and submitted, patients and providers can work together more effectively and navigate the healthcare system with greater ease.
Similar forms
- Prior Authorization Request Form: Similar to the Ambetter Outpatient form, this document facilitates the process of obtaining necessary approvals from insurance providers before a medical service is rendered. It also includes patient and provider information, and a detailed description of the requested services.
- Health Insurance Portability and Accountability Act (HIPAA) Release Form: Both documents require patient information and emphasize confidentiality. The HIPAA form ensures that patient data can be shared appropriately, similar to the confidentiality clauses in the Ambetter Outpatient form.
- Insurance Claim Form: This form is used to collect reimbursement after services rendered. Both the claim form and the Ambetter Outpatient form require details about the patient, provider, and services, though the latter focuses more on obtaining prior authorization.
- Referral Form: A referral form provides necessary information from a primary care provider to a specialist. Each document requires completion of critical patient and provider details and indicates the necessity of the requested services.
- Release of Information Authorization: This document allows healthcare providers to share patient information. Similar to the Ambetter Outpatient form, it requires patient identification and contains confidentiality clauses for the protection of sensitive information.
- Informed Consent Form: This form ensures that patients acknowledge understanding the proposed treatment and its risks. Both documents incorporate patient information and emphasize the importance of consent in the medical process.
- Medical Necessity Documentation: Documentation outlining the requirement of a specific service for a patient's condition. It aligns closely with the Ambetter Outpatient form in that both
Dos and Don'ts
When filling out the Ambetter Out Patient form, it’s essential to follow specific guidelines to ensure your submission is successful. Consider the following do's and don’ts:
- Do ensure all required fields are completed. Incomplete forms will be rejected.
- Do submit supporting clinical information along with the form. Lack of this information may cause delays.
- Do sign the urgent request if the situation requires immediate attention within 48 hours.
- Do clearly indicate the member’s ID and date of birth to avoid confusion.
- Do verify that all procedure and diagnosis codes are accurate and current.
- Don’t leave any mandatory fields blank, as this will lead to automatic rejection.
- Don’t forget to include the ordering provider's name and NPI, as these are crucial for processing.
- Don’t assume that prior submissions are sufficient; always attach current documentation relevant to the request.
- Don’t overlook the deadline. Standard requests are determined within 5 calendar days of receipt.
Adhering to these guidelines can streamline the authorization process and reduce the likelihood of delays.
Misconceptions
Here are some common misconceptions about the Ambetter Out Patient form:
- All fields on the form are optional. Many people believe they can skip fields, but all required fields must be filled out to avoid rejection of the form.
- The form guarantees payment. Some assume that submitting the form guarantees that the services will be paid for, but this is not true. An authorization is not a guarantee of payment.
- Urgent requests do not need a signature. It is a common misconception that urgent requests can be submitted without a signature. In fact, urgent requests must be signed by the requesting physician.
- Only medical procedures require authorization. Some people think that only medical procedures need authorization. However, behavioral health services also require authorization, including specific forms and supporting medical records.
- Submitting the form late is acceptable. Many believe that they can submit the form anytime before services are rendered. However, timely submission is important to ensure eligibility and avoid delays.
- Verbal authorization is enough. Some think that calling for a verbal authorization is sufficient. Written authorization is necessary to proceed with services.
- All services are covered by insurance. Individuals may assume that all types of services listed on the form are covered. Each service must be a covered benefit as per Ambetter policy.
- Only one procedure code is needed. A misconception exists that only one primary procedure code should be listed. Additional procedure codes can also be included when applicable.
- Confidentiality is not a concern. Some believe that confidentiality does not apply when submitting the form. In fact, the information is confidential and protected under HIPAA regulations.
Key takeaways
Filling out the Ambetter Outpatient Authorization Form can be a straightforward process if you keep some important aspects in mind. Here are key takeaways to help guide you:
- Complete Required Fields: Ensure all fields marked with an asterisk (*) are filled out. Incomplete forms will be rejected, delaying the authorization process.
- Authorization Requests: Know the difference between standard and urgent requests. Standard requests take up to five calendar days, whereas urgent requests need to be processed within 48 hours and must be signed to confirm urgency.
- Include Relevant Details: Provide precise member information, including the date of birth and member ID. Accurate information reduces processing time and minimizes errors.
- Specify Procedure Codes: Clearly list all procedure codes, including primary and additional ones, along with diagnosis codes. These codes are essential for determining the medical necessity of the requested services.
- Supporting Clinical Information: Attach all required clinical documentation. This information is vital for ensuring a smooth authorization process. Lack of necessary documentation can lead to delays.
- Confidentiality Matters: Remember that the information in your submission is confidential, and mishandling it can lead to serious privacy violations. Always ensure you're sending it to the intended recipient.
- Authorization Doesn't Guarantee Payment: Keep in mind that receiving authorization does not guarantee payment. Services still need to be covered benefits, and the member must be eligible at the time of service.
By keeping these key points in mind, you can effectively complete and use the Ambetter Outpatient Authorization Form, ultimately facilitating a smoother service experience.
Browse Other Templates
Mandatory Liability Insurance Alabama - Keep in mind your obligations as a vehicle owner under Alabama state laws.
Is Making Home Affordable Program Still Available - Using this form reduces the risk of medication errors during hospital visits.