Fill Out Your Amerigroup Authorization Request Form
Navigating the healthcare system can often feel overwhelming, especially when it comes to obtaining necessary medications for patients. The Amerigroup Authorization Request form serves as a vital tool in this process, streamlining the communication between healthcare providers and managed care organizations. This form is specifically designed to gather all essential information so that prior authorization for medications can be efficiently processed. It prompts for detailed patient information, such as name, date of birth, and medications, while also requiring an understanding of past treatments and current medical conditions. Each section plays a crucial role; from documenting the requested medication and its details, to providing relevant medical rationale, the depth of information sought on this form helps ensure that the requests are handled with the seriousness they deserve. By carefully completing the Amerigroup Authorization Request form, healthcare providers can not only enhance patient care but also alleviate the bureaucratic burdens that often accompany medication approvals. Additionally, the form provides opportunities for attaching relevant clinical documentation, which can strengthen the case for the requested medication. Understanding how to effectively fill out this form can significantly impact the approval timeline and patient outcomes.
Amerigroup Authorization Request Example
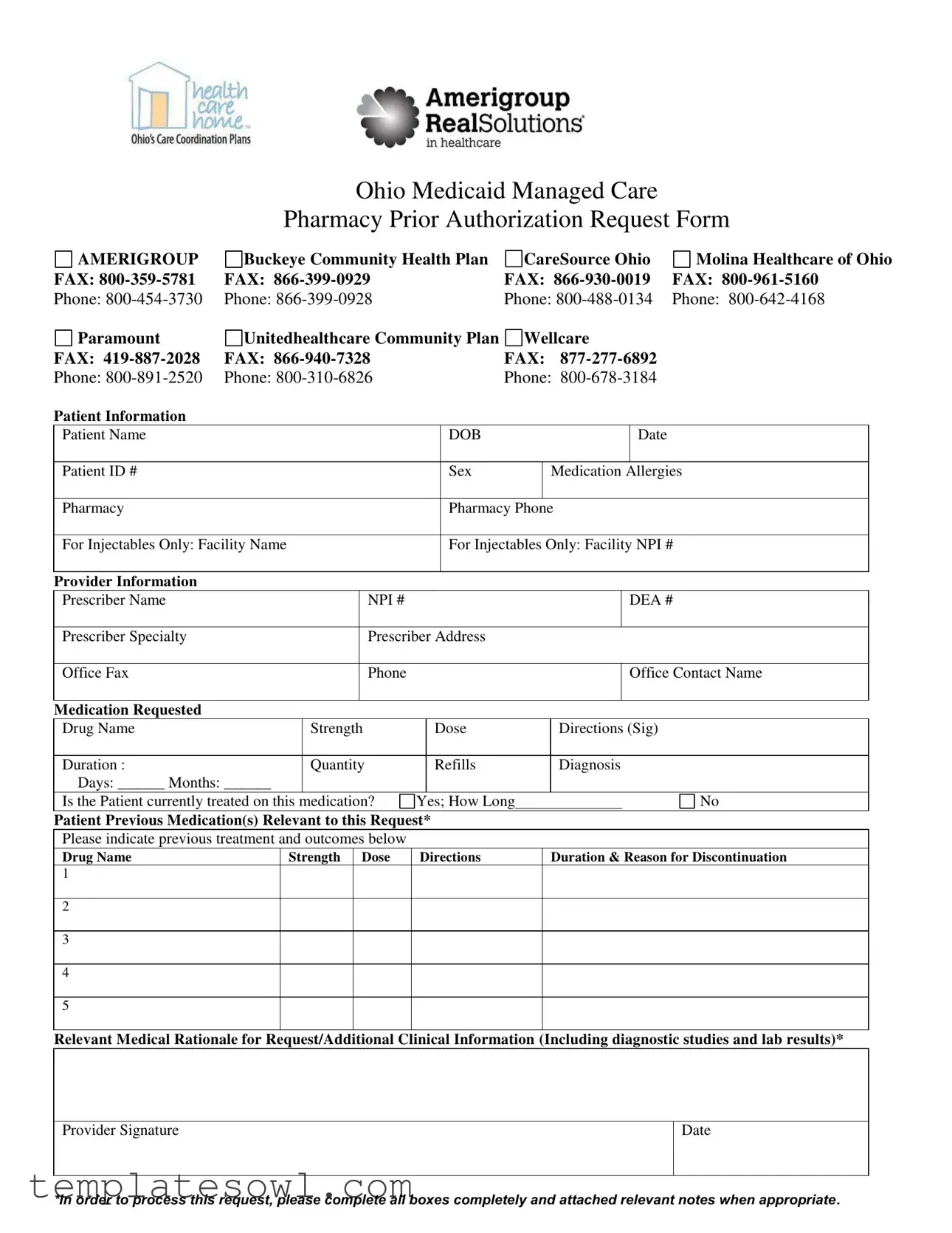
Ohio Medicaid Managed Care
Pharmacy Prior Authorization Request Form
AMERIGROUP |
Buckeye Community Health Plan |
CareSource Ohio |
Molina Healthcare of Ohio |
FAX: |
FAX: |
FAX: |
FAX: |
Phone: |
Phone: |
Phone: |
Phone: |
Paramount |
Unitedhealthcare Community Plan |
Wellcare |
|
FAX: |
FAX: |
FAX: |
|
Phone: |
Phone: |
Phone: |
|
Patient Information |
|
|
|
Patient Name |
DOB |
|
Date |
|
|
|
|
Patient ID # |
Sex |
Medication Allergies |
|
|
|
|
|
Pharmacy |
Pharmacy Phone |
||
|
|
||
For Injectables Only: Facility Name |
For Injectables Only: Facility NPI # |
||
|
|
|
|
Provider Information
Prescriber Name |
NPI # |
DEA # |
|
|
|
Prescriber Specialty |
Prescriber Address |
|
|
|
|
Office Fax |
Phone |
Office Contact Name |
|
|
|
Medication Requested |
|
|
|
|
|
|
|
|
|
Drug Name |
|
Strength |
|
Dose |
Directions (Sig) |
||||
|
|
|
|
|
|
|
|
|
|
Duration : |
|
Quantity |
|
Refills |
Diagnosis |
||||
Days: ______ Months: ______ |
|
|
|
|
|
|
|
|
|
Is the Patient currently treated on this medication? |
Yes; How Long |
|
|
No |
|||||
|
|
|
|
|
|
|
|||
Patient Previous Medication(s) Relevant to this Request* |
|
|
|||||||
Please indicate previous treatment and outcomes below |
|
|
|
|
|
|
|||
Drug Name |
Strength |
Dose |
Directions |
|
Duration & Reason for Discontinuation |
||||
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Relevant Medical Rationale for Request/Additional Clinical Information (Including diagnostic studies and lab results)*
|
|
Provider Signature |
Date |
|
|
*In order to process this request, please complete all boxes completely and attached relevant notes when appropriate.
Form Characteristics
| Fact Name | Description |
|---|---|
| State Specificity | This form is specifically designed for use in Ohio within the Medicaid Managed Care framework. |
| Participating Plans | Several health plans utilize this authorization form, including Amerigroup, Buckeye Community Health Plan, CareSource, and Molina Healthcare of Ohio. |
| Fax Numbers | The form includes distinct fax numbers for each participating plan, ensuring that requests can be directed appropriately. |
| Phone Contacts | A comprehensive list of phone numbers is provided for all participating health plans, offering direct assistance if needed. |
| Patient Identification | Key patient information is required, including the patient's name, date of birth, patient ID number, and medication allergies. |
| Injectable Medications | For injectable medications, the form specifically requests the facility name and NPI (National Provider Identifier) number where the medication will be administered. |
| Provider Information | Prescriber details are essential, including the prescriber's name, NPI number, DEA number, specialty, and contact information. |
| Previous Treatments | The form requires a history of previous medications relevant to the request, including treatment outcomes, to support the current request. |
| Clinical Rationale | Providers must supply relevant medical rationale and additional clinical information, including diagnostic studies and lab results, to justify the authorization request. |
| Completion Requirement | All sections must be filled out completely for the authorization request to be processed, with signatures required for validation. |
Guidelines on Utilizing Amerigroup Authorization Request
Completing the Amerigroup Authorization Request form requires careful attention to detail. Each section must be filled out accurately to ensure that the patient's needs are effectively communicated. After submitting the form, you will await a response that determines the requested medication's approval. This process may take some time, so it's wise to be prepared for any follow-up that may be necessary.
- Begin by gathering all the necessary information about the patient, including their full name, date of birth, and patient ID number.
- Fill in the patient's sex and note any medication allergies they may have.
- Identify the pharmacy where the patient plans to obtain the medication, including the pharmacy's phone number.
- If the request is for injectables, enter the facility name and the facility's NPI number.
- Next, complete the provider information section, starting with the prescriber's name, NPI number, DEA number, and specialty.
- Input the prescriber's address, office fax number, phone number, and the name of a contact person in the office.
- In the medication requested section, write the drug name, strength, dosage directions (Sig), duration, quantity, and refills needed.
- Specify the diagnosis and indicate whether the patient is currently being treated with this medication, including how long they have been receiving it.
- Record any previous medications related to this request, detailing each drug name, strength, dosage directions, duration, and reason for discontinuation where applicable.
- Provide a relevant medical rationale for the request, including any diagnostic studies and lab results that support the need for the medication.
- Finally, ensure the provider signs and dates the form to validate the request.
What You Should Know About This Form
What is the purpose of the Amerigroup Authorization Request form?
The Amerigroup Authorization Request form is designed to facilitate the prior authorization process for medications under the Ohio Medicaid Managed Care program. By submitting this form, healthcare providers can obtain permission from Amerigroup to prescribe specific medications for their patients, ensuring that the treatments align with the insurance’s coverage policies.
Who should complete the Amerigroup Authorization Request form?
The form should be completed by healthcare providers, typically physicians or other licensed prescribers. They are responsible for providing accurate patient and medication information to support the authorization request. It is crucial that the prescriber ensures all sections of the form are filled out completely to avoid delays in processing.
What specific information is required on the form?
Key information required includes the patient’s name, date of birth, Medicaid ID number, and relevant medical history. Additionally, providers must provide detailed information about the medication requested, including the drug name, strength, dosing directions, and diagnosis. Previous medications and treatment outcomes must also be documented, along with any supporting clinical information.
Why is it important to include previous medications on the form?
Providing a history of previous medications is vital in justifying the need for the new request. It outlines the treatment course the patient has undergone and indicates whether the current medication is necessary due to ineffectiveness or adverse reactions to prior treatments. This information helps streamline the approval process by giving context to the prescriber's decision.
What are the potential consequences of incomplete forms?
If the form is submitted without complete information, it may result in delays or denials of the authorization request. Amerigroup requires all sections to be filled out accurately to assess the necessity of the requested medication effectively. Providers will need to follow up with a resubmission or additional documentation, which can prolong the time a patient waits for access to necessary medications.
How can I submit the Amerigroup Authorization Request form?
The completed form can be submitted via fax to the respective Amerigroup fax number designated for prior authorization requests. Each insurance carrier associated with the program has its own fax number listed on the form. It is essential to ensure that the correct number is used to avoid misdirected submissions.
What should be done if the request is denied?
If a prior authorization request is denied, the provider should receive a detailed explanation, typically accompanied by an option to appeal the decision. The provider can often resubmit the request with additional supporting information or clarification to address the reasons for denial. Engaging with the Amerigroup customer service representative can provide guidance through the appeals process.
How long does it take to process the authorization request?
The processing time for authorization requests can vary, but it generally takes several business days. Providers should verify with Amerigroup on the expected turnaround time for their specific request. Timely submission of the form and comprehensive details can help expedite the review process.
What happens if the patient is currently on the medication?
If the patient is currently being treated with the medication, the authorization form should include information regarding the duration of that treatment. Amerigroup often requires this information to ascertain ongoing medical necessity and continuity of care for the patient. It is essential to elaborate on the patient’s response to the medication and the reason for continuing therapy.
What should be included in the relevant medical rationale for the request?
The relevant medical rationale should clearly outline the clinical necessity for the medication requested. This includes any supporting diagnostic studies, laboratory results, and detailed explanations of the patient’s condition that justifies the use of the medication. Comprehensive rationale strengthens the case for approval and clarifies how the treatment aligns with the patient’s healthcare needs.
Common mistakes
Completing the Amerigroup Authorization Request form is an important step in receiving the necessary medical treatment. However, many individuals overlook certain aspects of the form, leading to delays or denials of authorization. Here are ten common mistakes to watch for when filling out this form.
First, providing incomplete patient information is a frequent issue. Failing to include essential details, such as the patient's name, date of birth, and ID number, can hinder the processing of the request. Each piece of information is crucial for identifying the patient in the system.
Another common mistake is neglecting to specify medication allergies. Forgetting to list allergies or stating them ambiguously may lead to inappropriate medication being prescribed. This information is vital for ensuring patient safety.
Errors in the "Medication Requested" section are prevalent. Some individuals mistakenly assume that the prescriber’s signature is sufficient and do not include the necessary drug name, strength, or dosage instructions. Each field must be meticulously filled out to avoid confusion later on.
Moreover, related to the previous point, skipping the duration and quantity fields can create complications. The reviewing party needs to know how long the medication is to be taken and how much will be supplied. Omitting this information can result in processing delays.
It's also important to include information about previous medications. Many individuals do not detail past treatments, leaving out crucial context. This information helps convey the necessity of the requested medication and can demonstrate prior treatment failures.
Providing inadequate medical rationale can be detrimental as well. Many requesters write vague explanations instead of supplying detailed and relevant clinical information, which might include diagnostic studies and lab results. A well-articulated rationale supports the necessity of the requested treatment.
Additionally, forgetting to sign the form is a common oversight. Without a signature, the request is incomplete and cannot be processed. A simple step that is often overlooked can lead to significant delays.
Not attaching necessary documentation is another mistake that can derail the request process. Supporting notes from previous treatments or lab results may be required to justify the request. Omitting these can weaken the case for authorization.
Some individuals fail to double-check the contact information provided for both the provider and the pharmacy. If incorrect, this could lead to miscommunication or delays in obtaining approval or the medication itself.
Finally, misunderstanding the distinctions between "Yes" and "No" answers regarding current treatment can lead to incorrect submissions. Clear and accurate responses in this section help clarify the patient's current status and need for the medication.
Being mindful of these common errors can streamline the authorization process, ensuring patients receive their required medications promptly and efficiently.
Documents used along the form
When working with the Amerigroup Authorization Request form, it's essential to understand the additional documents that are often required to support the request. These forms can help streamline the approval process and ensure that all necessary information is provided. Here are five forms you might encounter:
- Ohio Medicaid Managed Care Pharmacy Prior Authorization Request Form: This form is crucial for requesting coverage for medications not typically covered under Ohio Medicaid. It provides detailed patient information and physician descriptors to facilitate the authorization process.
- Clinical Summary: A brief overview of the patient’s medical history relevant to the requested treatment. This document highlights previous medications, diagnoses, and treatment outcomes, helping the reviewer understand the necessity of the request.
- Letter of Medical Necessity: Written by the healthcare provider, this letter explains why the requested medication or treatment is essential for the patient’s health. It typically includes evidence or rationale supporting the need for the specific therapy.
- Prior Medications List: A compilation of medications the patient has previously tried, including their dosages and durations. This can support the request by demonstrating the patient’s treatment history and responses to other options.
- Test Results and Diagnostic Reports: Relevant medical documents, such as lab results or imaging reports, that can substantiate the diagnosis and the need for the requested service or medication. These documents provide concrete evidence of the patient's condition.
When submitting the Amerigroup Authorization Request form, having these additional documents ready can enhance the chances of a successful approval. Providing comprehensive information about the patient's history and current needs helps ensure that the healthcare team can make informed decisions regarding treatment options.
Similar forms
The following documents are similar to the Amerigroup Authorization Request form in purpose and function. Each document serves to facilitate the approval process for medical services or medications. Here’s a detailed breakdown:
- Ohio Medicaid Managed Care Pharmacy Prior Authorization Request Form: This document is specifically used for Medicaid patients in Ohio, just like the Amerigroup form, to obtain necessary permissions for prescribed medications.
- CareSource Prior Authorization Form: CareSource requires this form to evaluate requests for coverage. It assesses the medical necessity of certain services, mirroring the Amerigroup process.
- Molina Healthcare Prior Authorization Request: Molina's form also gathers patient and provider information to review requests, ensuring compliance with medication management similar to Amerigroup.
- Buckeye Community Health Plan Prior Authorization Form: This form enables providers to submit requests for treatment approvals, much like the Amerigroup Authorization Request.
- UnitedHealthcare Community Plan Prior Authorization Form: Similar to the Amerigroup Authorization Request, this form seeks clear documentation from a provider to justify treatment necessity.
- WellCare Prior Authorization Request: This document is used to obtain approvals for health services, focusing on medical necessity and treatment history like the Amerigroup form.
- Paramount Authorization Request Form: Providers use this form to request prior authorizations for medications. It emphasizes detailed patient information and diagnostic history as in Amerigroup.
- Highmark Prior Authorization Form: This document, like Amerigroup's, is designed to ensure that the requested services align with medical necessity assessments conducted by the health plan.
- Anthem Blue Cross Blue Shield Authorization Request: Anthem requires similar information to evaluate request validity, focusing on patient history and clinical rationale akin to the Amerigroup format.
Dos and Don'ts
When filling out the Amerigroup Authorization Request form, it is critical to ensure accuracy and completeness to avoid delays in processing. Here are eight important dos and don’ts to keep in mind:
- Do fill out all sections of the patient and provider information accurately.
- Do include the patient's medication allergies to prevent any health risks.
- Do provide a detailed medical rationale for the requested medication.
- Do attach any relevant notes that support the request.
- Don’t leave any boxes incomplete; missing information can lead to processing delays.
- Don’t forget to include the prescriber’s signature and date for validation.
- Don’t use abbreviations or unclear terms that may confuse reviewers.
- Don’t submit the form without double-checking for any errors or omissions.
Following these guidelines will help facilitate a smoother authorization process. Act promptly and ensure all details are clear and accurate.
Misconceptions
The Amerigroup Authorization Request form can often be misunderstood. Below are some common misconceptions and clarifications to help you navigate the process more effectively.
- Misconception 1: The form is only for certain medications.
- Misconception 2: Only doctors can submit the form.
- Misconception 3: Filling out the form is a quick process.
- Misconception 4: It doesn't matter if I don't include relevant previous medications.
- Misconception 5: The authorization request will always be approved.
- Misconception 6: Once submitted, I cannot follow up on the request.
- Misconception 7: There's no need to provide additional clinical information.
- Misconception 8: The process is the same for all Medicaid plans.
Fact: The form can be used for a wide range of medications that require prior authorization, including those for complex conditions.
Fact: While it’s typically submitted by healthcare providers, patients can advocate for their request, ensuring all necessary information is included.
Fact: Completing the form accurately takes time. Ensure that all sections, especially medical history and rationale, are thoroughly addressed.
Fact: Previous medication details are crucial for the review process. They help justify the need for the requested medication.
Fact: Approval isn't guaranteed. Each request is evaluated based on medical necessity and the specific criteria of the plan.
Fact: You can and should follow up if you don’t receive a timely response. Staying informed is key to ensuring your request is processed.
Fact: Additional documentation, such as lab results and diagnostic studies, can significantly strengthen your request.
Fact: Different plans may have varying requirements and processes. Familiarize yourself with the specific procedures for Amerigroup and related providers in your state.
Key takeaways
When filling out the Amerigroup Authorization Request form, consider the following key takeaways:
- Complete All Fields: Ensure that every section of the form is filled out completely. Missing information can lead to delays in processing your request.
- Include Relevant Medical Rationale: When providing clinical information, clearly outline the rationale for the medication request. This helps convey the medical necessity to the reviewer.
- Attach Supporting Documentation: Including relevant notes, diagnostic studies, and lab results can strengthen your request. Make sure to attach these documents as needed.
- Double-Check Contacts: Verifying provider information, including the office fax and phone numbers, is crucial. Accurate contact details ensure smooth communication for any follow-up questions.
Browse Other Templates
Nycha Careers - NYCHA's Human Resources Department oversees the accommodation request process thoroughly.
Letter to School for Absence of Child - Indicates whether the student can return immediately or later.
Dwp Pip Payments - Provide information about medications you are currently taking.