Fill Out Your Amerigroup Medicaid Form
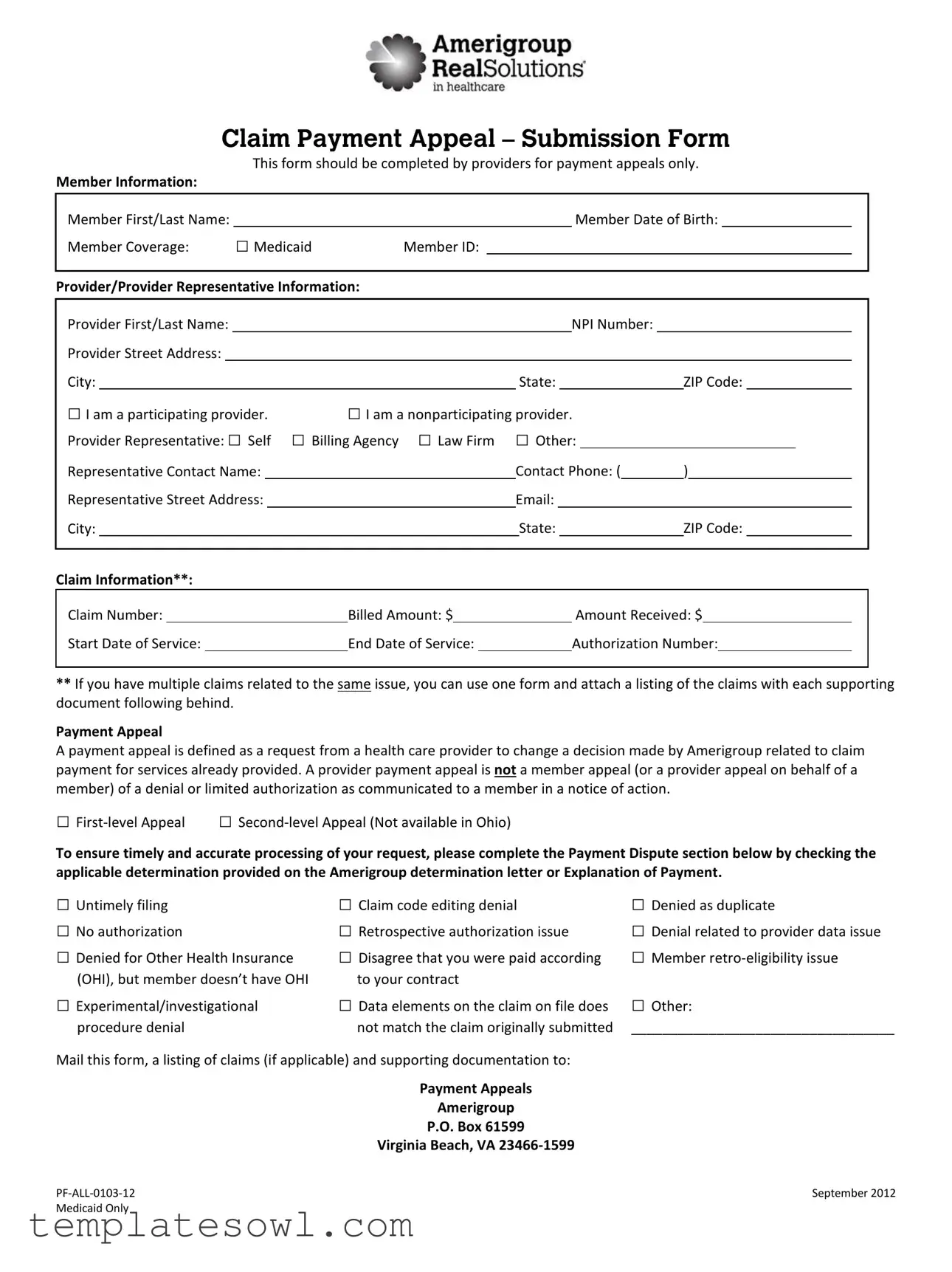
The Amerigroup Medicaid Claim Payment Appeal Submission Form is a crucial tool for healthcare providers seeking to challenge decisions about payment for services rendered. Filling out this form properly is essential for ensuring that claims are reviewed and potentially reconsidered. It collects detailed member information, including the member's name, date of birth, coverage type, and Medicaid ID. Additionally, providers must provide their details, including name, NPI number, and the nature of their participation (whether they are a participating or nonparticipating provider). There’s a section for the representative's information, allowing for various options such as self, billing agency, or law firm. Claim specifics, including claim number, billed amount, and the received amount, must also be included. There’s even room for related claims, ensuring that multiple issues can be addressed in one submission. The form differentiates between first-level and second-level appeals, urging providers to specify the nature of the dispute by checking relevant issues like untimely filing or denial due to authorization problems. Finally, completed forms and any supporting documents should be sent to the designated address, streamlining the appeal process. This form embodies the essential communication between providers and Amerigroup, fostering clarity and efficiency in the resolution of payment disputes.
Amerigroup Medicaid Example

|
|
|
Claim Payment Appeal – Submission Form |
|||||||||||||||||||||||
|
|
|
|
|
This form should be completed by providers for payment appeals only. |
|||||||||||||||||||||
Member Information: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Member First/Last Name: |
|
|
|
|
|
|
|
|
|
|
Member Date of Birth: |
|||||||||||||||
Member Coverage: |
□ Medicaid |
Member ID: |
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Provider/Provider Representative Information: |
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Provider First/Last Name: |
|
|
|
|
|
|
|
|
|
|
NPI Number: |
|
|
|
|
|
|
|
|
|
||||||
Provider Street Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
City: |
|
|
|
|
|
|
|
|
|
State: |
|
|
|
|
|
ZIP Code: |
|
|
||||||||
□ I am a participating provider. |
□ I am a nonparticipating provider. |
|
|
|
|
|
|
|
|
|
||||||||||||||||
Provider Representative: □ Self □ Billing Agency □ Law Firm □ Other: |
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
Representative Contact Name: |
|
|
|
|
|
Contact Phone: ( |
) |
|
|
|
|
|
|
|||||||||||||
Representative Street Address: |
|
|
|
|
|
|
Email: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
City: |
|
|
|
|
|
|
|
|
State: |
|
|
|
|
ZIP Code: |
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Claim Information**: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
Claim Number: |
|
|
|
|
Billed Amount: $ |
Amount Received: $ |
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
Start Date of Service: |
|
|
|
End Date of Service: |
Authorization Number: |
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
**If you have multiple claims related to the same issue, you can use one form and attach a listing of the claims with each supporting document following behind.
Payment Appeal
A payment appeal is defined as a request from a health care provider to change a decision made by Amerigroup related to claim payment for services already provided. A provider payment appeal is not a member appeal (or a provider appeal on behalf of a member) of a denial or limited authorization as communicated to a member in a notice of action.
□
To ensure timely and accurate processing of your request, please complete the Payment Dispute section below by checking the applicable determination provided on the Amerigroup determination letter or Explanation of Payment.
□ Untimely filing |
□ Claim code editing denial |
□ Denied as duplicate |
□ No authorization |
□ Retrospective authorization issue |
□ Denial related to provider data issue |
□ Denied for Other Health Insurance |
□ Disagree that you were paid according |
□ Member |
(OHI), but member doesn’t have OHI |
to your contract |
|
□ Experimental/investigational |
□ Data elements on the claim on file does |
□ Other: |
procedure denial |
not match the claim originally submitted |
__________________________________ |
Mail this form, a listing of claims (if applicable) and supporting documentation to:
Payment Appeals
Amerigroup
P.O. Box 61599
Virginia Beach, VA
September 2012 |
|
Medicaid Only |
|
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | This form is specifically for providers to request payment appeals. It can only be used for appeals related to payments for already provided services. |
| Member Information | Providers must enter the member's full name, date of birth, and Medicaid member ID on the form. |
| Provider Details | Providers need to provide their name, NPI number, and address. It’s important to confirm if they are participating or nonparticipating providers. |
| Claim Information | The form requires details about the claim, including the claim number, billed amount, amount received, and service dates. |
| Payment Appeal Definition | A payment appeal is a request to change a payment decision made by Amerigroup. It does not cover member appeals or provider appeals on behalf of a member. |
| Appeal Levels | Providers can select either a first-level or second-level appeal. Note that second-level appeals are not available in Ohio. |
| Dispute Reasons | Providers must specify the reason for the appeal by checking applicable items, such as untimely filing or denial for lack of authorization. |
| Mailing Address | The completed form and supporting documents should be sent to: Payment Appeals, Amerigroup, P.O. Box 61599, Virginia Beach, VA 23466-1599. |
| Applicable State Laws | Medicaid rules and regulations vary by state. Providers should consult state-specific laws when completing the form. |
Guidelines on Utilizing Amerigroup Medicaid
When seeking to submit a payment appeal using the Amerigroup Medicaid form, it is important to have all relevant information at your fingertips. Completing the form accurately will ensure your request is processed in a timely manner. The following steps outline how to fill out the necessary information on the Amerigroup Medicaid form.
- Start with the Member Information section.
- Enter the Member First and Last Name.
- Fill in the Member Date of Birth.
- Provide the Member Coverage information and Member ID.
- Next, move to the Provider/Provider Representative Information section.
- Input the Provider First and Last Name.
- Enter the NPI Number.
- Complete the Provider Street Address, City, State, and ZIP Code.
- Indicate whether the provider is a participating or nonparticipating provider by checking the appropriate box.
- Detail the Provider Representative information.
- Mark if the representative is Self, Billing Agency, Law Firm, or Other.
- Provide the Representative Contact Name and Contact Phone.
- Include the Representative Street Address, City, State, and ZIP Code.
- Don’t forget to enter the Email address.
- Now, proceed to the Claim Information section.
- Fill in the Claim Number, Billed Amount, and Amount Received.
- Enter the Start Date of Service and End Date of Service.
- Provide the Authorization Number.
- If you have multiple claims, attach a list of those claims along with this form.
- Now, move to the Payment Appeal section.
- Select either First-level Appeal or Second-level Appeal (not applicable in Ohio).
- Check the relevant payment dispute reasons based on the Amerigroup determination letter.
- Lastly, mail the completed form, any additional claim listings, and supporting documents to:
- Payment Appeals
- Amerigroup
- P.O. Box 61599
- Virginia Beach, VA 23466-1599
What You Should Know About This Form
What is the purpose of the Amerigroup Medicaid form?
The Amerigroup Medicaid form is designed specifically for providers who wish to appeal payment decisions made by Amerigroup. If a provider feels that a claim for services already rendered has been unfairly denied or adjusted, this form provides a structured way to request a reconsideration of that decision. It is crucial for providers to use this form to ensure their appeal is processed in a timely manner, thereby helping them secure the funds owed for their services.
Who should complete the appeal form?
The form should be filled out by the health care provider or their representative only for payment appeals. This includes individual providers, billing agencies, law firms, or other representatives acting on behalf of the provider. Each section must be completed accurately to avoid delays in the appeal process.
What information do I need to provide on the form?
How do I determine whether to submit a first-level or second-level appeal?
What common reasons might warrant a payment appeal?
There are various reasons a provider may wish to appeal a payment decision. Common issues include untimely filing, duplicate claims, lack of authorization, and adjustments based on other health insurance. The payment appeal form allows you to check off the applicable reasons directly, streamlining the process of communicating your specific concerns to Amerigroup.
Where should I send the completed appeal form?
After completing the Amerigroup Medicaid form along with any necessary supporting documentation, it is important to mail it to the following address: Payment Appeals, Amerigroup, P.O. Box 61599, Virginia Beach, VA 23466-1599. Ensure that all information is accurately compiled before mailing to avoid any processing delays.
Common mistakes
When filling out the Amerigroup Medicaid Claim Payment Appeal form, many individuals overlook essential details that can hinder the appeal process. One common mistake is neglecting to provide complete member information. The form requires both the first and last names of the member, along with their date of birth and Medicaid member ID. Failure to include any of these details can delay processing and affect the outcome of the appeal.
Another frequent error involves the provider information section. Incorrectly entering the provider's NPI number can result in immediate rejection of the appeal. This critical identifier must be accurate to ensure that the appeal is linked to the appropriate provider. Also, some may forget to indicate their participation status, either as a participating or nonparticipating provider, which influences how the claim is processed.
Additionally, claim-related information must be filled out with precision. Many make the mistake of misreporting the claim number, billing amount, or amount received. Any inaccuracies in these figures can lead to confusion and complications. It's vital to cross-check these numbers with the original claim documents before submitting the form.
Some individuals fail to check the correct payment dispute reason as outlined on the Amerigroup determination letter. Selecting the wrong reason can mislead the process and may result in the appeal being denied. Each option is important, and it’s crucial to reflect accurately the reason for the appeal to support your case effectively.
Providing insufficient supporting documentation is another serious oversight. Many believe that submitting the form alone is enough. Instead, any relevant documents that substantiate the claim must accompany the appeal. Without these documents, the review team may not have enough information to support your request.
Finally, some people overlook the mailing instructions and fail to take note of the specific address. It's essential to send the completed form and attachments to the correct location: Payment Appeals at Amerigroup in Virginia Beach, VA. Misaddressing the appeal can delay processing further and prevent a timely resolution.
Documents used along the form
The Amerigroup Medicaid form is essential for healthcare providers seeking to appeal payment decisions. However, there are several other documents that may accompany or complement this form in the claims and appeals process. Understanding these forms can help facilitate smoother interactions with Medicaid and ensure that all necessary information is submitted. Here’s a brief overview of other important forms often used alongside the Amerigroup Medicaid form:
- Medicaid Application Form: This form is used by eligible individuals to apply for Medicaid benefits. It collects personal, financial, and medical information to determine eligibility.
- Authorization for Release of Information: This document authorizes healthcare providers to share a patient’s medical information with insurers or other parties, facilitating the claims process.
- Claim Submission Form: Providers use this form to detail the services rendered to a patient. It includes information like procedure codes, dates of service, and billed amounts, which are essential for reimbursement.
- Explanation of Benefits (EOB): After a claim is processed, this document provides a summary of what costs were covered by Medicaid and what the patient may owe, helping to clarify payment details.
- Secondary Insurance Claim Form: If a patient has multiple insurance policies, this form is used to submit claims to a secondary insurer after Medicaid has processed the initial claim.
- Patient Acknowledgment Form: Providers may ask patients to sign this form, confirming that they understand their insurance coverage and any potential out-of-pocket costs related to their care.
- Payment Agreement Form: This document outlines the payment arrangements made between the provider and the patient, detailing responsibilities for unpaid balances after Medicaid processing.
- Incident Report Form: In cases of service-related issues or complaints, this form is completed to document the event thoroughly and may be used in appeals if necessary.
- Provider Credentialing Application: This form collects information on a healthcare provider's qualifications and is essential for ensuring the provider is authorized to participate with Medicaid.
Gathering the right documentation is key to successful claim appeals and overall management of Medicaid services. Be sure to keep these forms handy in case they are required during the process.
Similar forms
- Insurance Claim Form: This document is used by healthcare providers to bill insurance companies for services rendered. Like the Amerigroup Medicaid form, it requires details about the patient, provider, and the services performed, ensuring that the billing process is systematic and organized.
- Medicaid Provider Claim Form: Similar to the Amerigroup form, this is specifically designed for providers who bill Medicaid for their services. It includes sections for provider information, member details, and claim specifics, making it essential for claims processing.
- Claim Denial Appeal Form: This form allows providers to contest a denied claim. Both this form and the Amerigroup Medicaid form initiate a formal review process aiming to overturn unfavorable decisions regarding payment, focusing on particular reasons for denial.
- Authorization Request Form: Used to request prior authorization for services, this form shares the same type of provider and member information as the Amerigroup Medicaid form. Both are essential in the lifecycle of a Medicaid claim to ensure approvals are obtained for specified services.
- Patient Billing Statement: This document is provided to patients to detail charges for services rendered. While primarily for patient communication, it shares similarities with the Amerigroup form by breaking down services and amounts, allowing for clarity in billing disputes.
- Provider Enrollment Application: This application allows healthcare providers to enroll in insurance networks. Like the Amerigroup Medicaid form, it gathers essential provider information to facilitate smoother interactions with insurance companies regarding payments and services.
- Explanation of Benefits (EOB): This document explains how much an insurance company paid for a claim and why certain amounts were covered or denied. Both the EOB and the Amerigroup Medicaid form aim to clarify payment decisions, providing healthcare providers insight into accepted claims and necessary appeals.
Dos and Don'ts
When filling out the Amerigroup Medicaid form, it’s essential to ensure accuracy and completeness. Here’s a list of things to do and avoid:
- Double-check your member’s information. Accuracy in the member's name and date of birth is crucial.
- Provide a complete address. Make sure both your street address and ZIP code are correct.
- Use the correct provider type. Indicate whether you are a participating or nonparticipating provider.
- Attach all necessary documentation. Include a list of claims and supporting documents if there are multiple claims.
- Specify the correct claim issue. Choose the applicable determination from the provided options.
- Avoid leaving any sections blank. Each part of the form must be filled out.
- Avoid using outdated information. Ensure all data is current before submission.
- Don’t ignore deadlines. Timely filing is essential for a successful appeal.
- Refrain from submitting claims without proper authorization. Ensure you have the necessary approvals.
- Do not forget to include a return address on the envelope when mailing the form. Ensure you can be contacted if necessary.
Misconceptions
Understanding the Amerigroup Medicaid form is essential for healthcare providers seeking to navigate the appeal process. Unfortunately, some misconceptions could lead to confusion or delays. Here are ten common misconceptions explained:
- All claims can be appealed using this form. This form is specifically for payment appeals. It cannot be used for member appeals or general inquiries regarding claim denials.
- The appeal process is the same for all states. The second-level appeal option is not available in Ohio. Each state may have different regulations regarding the appeal process.
- Only participating providers can use this form. Both participating and nonparticipating providers can use the form. It's important for nonparticipating providers to indicate their status clearly.
- A single appeal form can only address one claim. You can submit multiple claims related to the same issue using one form. Just attach a list of the claims being appealed.
- All supporting documents should be attached to the claim. Supporting documents must be relevant to the appeal. Attach them carefully to make the case clearer.
- An appeal guarantees payment. Submitting an appeal does not guarantee that the claim will be paid. It only allows for the decision to be reconsidered.
- Timely filing is not a concern if you have an appeal. Appeals can be denied due to untimely filing. Always double-check specific deadlines for submissions.
- There’s no need to follow up after submitting the form. Following up can be crucial. It helps ensure that your appeal is being processed and that no additional information is needed.
- You don't have to fill out all sections of the form. Completeness is key. Every section has significance in the review process, so ensure all relevant information is provided.
- The same reasons for denial can be reused for different claims. While some denial reasons may overlap, each claim should be analyzed individually to determine the appropriate grounds for appeal.
By understanding these misconceptions, providers can increase their chances of successfully navigating the appeal process with Amerigroup.
Key takeaways
Here are some key takeaways for filling out and using the Amerigroup Medicaid form:
- Purpose of the Form: This form is specifically for payment appeals from healthcare providers regarding claim decisions made by Amerigroup.
- Member Information: It is essential to provide accurate details, including the member's full name, date of birth, and Medicaid Member ID.
- Provider Details: Include your full name, NPI number, and contact information. Be clear about whether you are a participating or nonparticipating provider.
- Claim Information: Accurately fill in the claim number, billed amount, amount received, service dates, and authorization number.
- Multiple Claims: If appealing for multiple claims, use one form for all. Attach a list of the claims and all relevant supporting documents.
- Payment Appeal Options: Specify if this is a first-level or second-level appeal. Note that the second-level appeal is not available in Ohio.
- Dispute Areas: Check the relevant reason for the payment appeal, such as untimely filing or authorization issues, as noted in the determination letter or Explanation of Payment.
Following these key points will help streamline the process and increase the chances of a successful appeal.
Browse Other Templates
What Happens in a Physical - Common symptoms like chest pain or shortness of breath are recorded as they arise.
Gun License California 2024 - This license is meant to enhance personal security while upholding community safety.