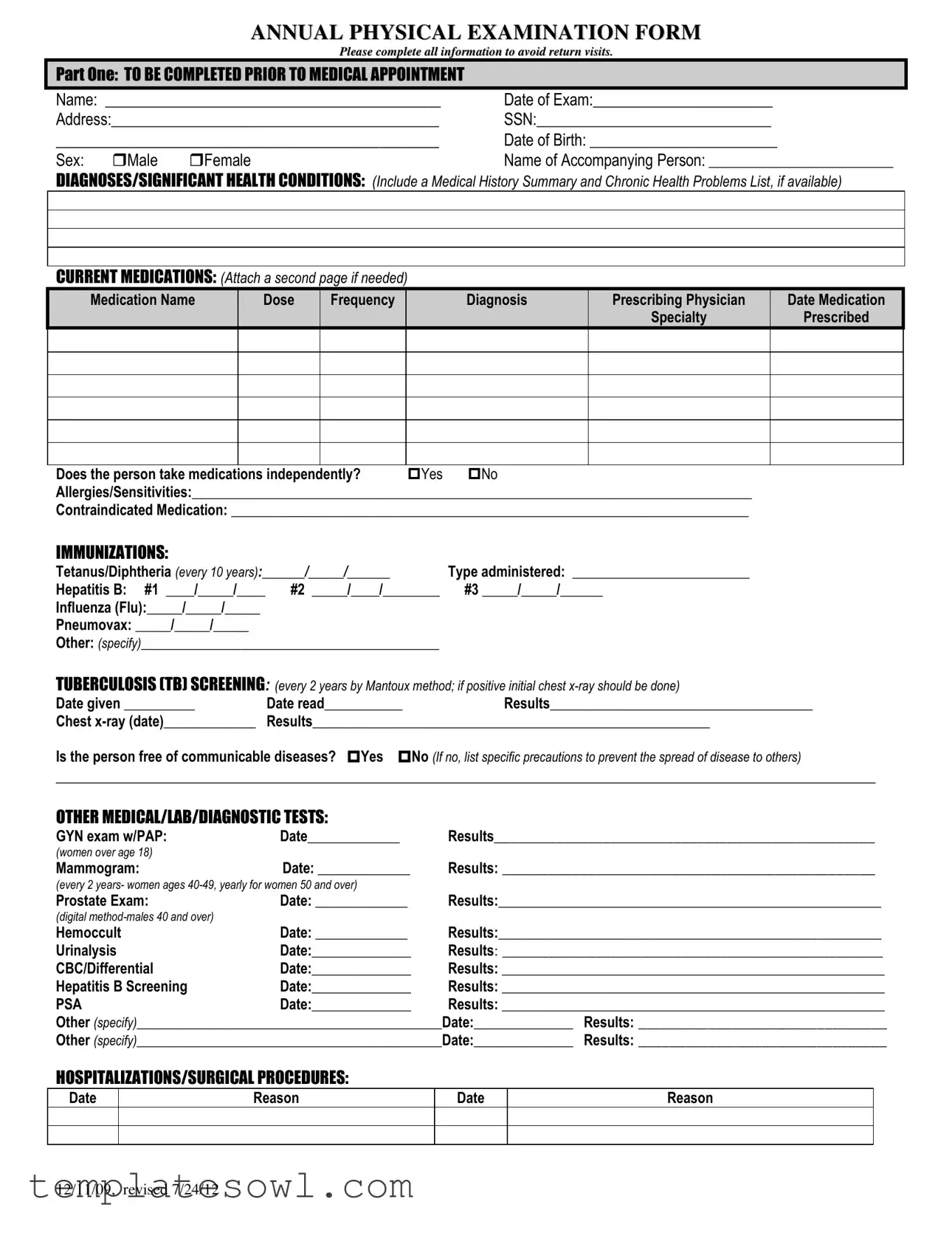
Fill Out Your Annual Physical Examination Form
The Annual Physical Examination form plays a pivotal role in ensuring that patients receive comprehensive healthcare assessments. Designed to gather essential information, the form requires individuals to provide personal details such as their name, date of birth, and current medications, along with a summary of any significant health conditions and allergies. Prior to the appointment, patients must also disclose their immunization history, including updates on tetanus, hepatitis, and flu vaccinations. A thorough evaluation of system functions, ranging from respiratory to neurological assessments, helps physicians identify any health concerns that may need further attention. Additionally, sections on hospitalizations, surgical procedures, and recommendations for future care offer both patients and healthcare providers valuable insights for ongoing health management. Completing this form accurately and thoroughly can contribute to a more effective examination process and help prevent unnecessary follow-up visits, thereby streamlining patient care.
Annual Physical Examination Example
ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12
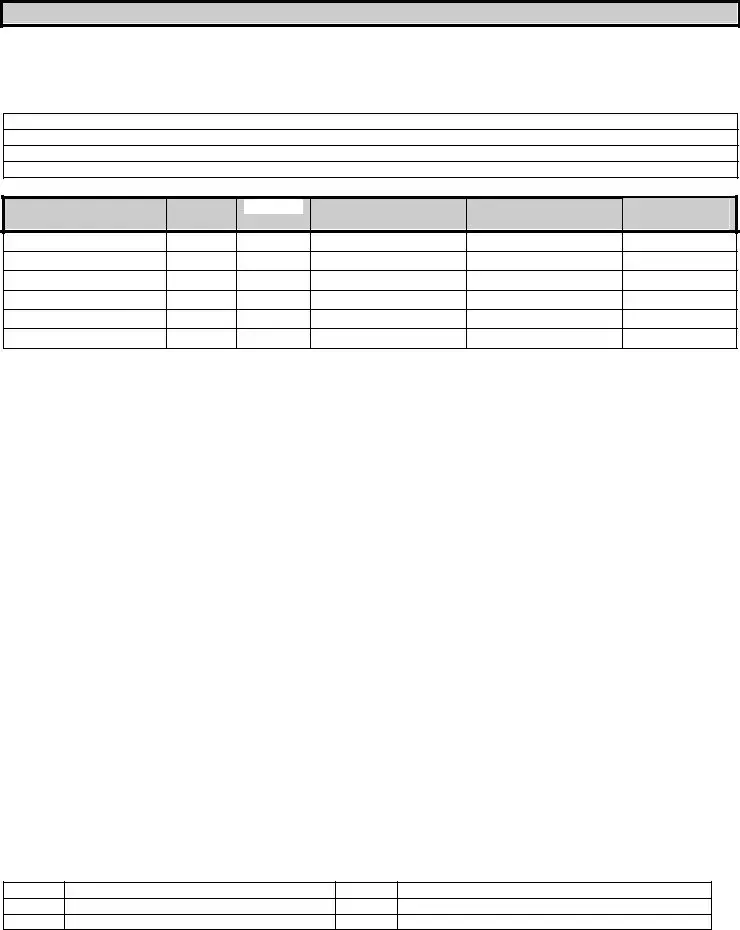
PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12

Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The Annual Physical Examination form is designed to collect comprehensive health information from patients before their medical appointment. |
| Medical History | Patients are required to provide a summary of their medical history, including significant conditions and ongoing medications, to ensure appropriate care. |
| Immunizations | Details about immunizations, such as Tetanus/Diphtheria and Influenza, must be documented to maintain up-to-date records and ensure patient safety. |
| TB Screening Requirement | According to CDC guidelines, a tuberculosis screening is necessary every two years using the Mantoux method for eligible individuals. |
| Evaluations of Systems | A thorough assessment is conducted across various body systems to identify any potential health issues, indicated by normal findings or comments. |
| Adaptive Equipment | The form includes a section to identify whether the patient uses any adaptive equipment, which is crucial for tailoring medical advice. |
| Restrictions for Activities | Patients must indicate if there are any limitations regarding their daily activities or work, ensuring health providers are informed. |
| Physician’s Verification | A physician’s signature is necessary at the bottom of the form, confirming that the information provided has been reviewed and medical advice has been given. |
Guidelines on Utilizing Annual Physical Examination
After gathering all necessary information, individuals can proceed to fill out the Annual Physical Examination form. It is important to provide accurate and comprehensive details to ensure a smooth and effective medical appointment. The following steps outline the process for completing the form.
- Begin by filling out your Name in the designated space.
- Enter the Date of Exam.
- Provide your Address in the specified section.
- Include your Social Security Number (SSN).
- Fill in your Date of Birth.
- Select your Sex by marking the appropriate box.
- Write down the Name of Accompanying Person, if applicable.
- Detail your Diagnoses/Significant Health Conditions, including any medical history or chronic health problems.
- List any Current Medications you are taking, along with dosage and frequency. Attach a second page if necessary.
- Indicate whether you take medications independently by marking Yes or No.
- Note any Allergies/Sensitivities you have.
- List any Contraindicated Medications.
- Complete the Immunizations section, entering the dates and types of vaccines received.
- Provide information for the Tuberculosis (TB) Screening, including dates and results.
- Fill out any Other Medical/Lab/Diagnostic Tests applicable to you.
- Record any Hospitalizations/Surgical Procedures, including dates and reasons.
- Complete the General Physical Examination section, filling in your blood pressure, pulse, respirations, temperature, height, and weight.
- Evaluate each system in the Evaluation of Systems section, marking whether the findings are normal or not.
- Fill out the Vision Screening and Hearing Screening sections, indicating further evaluations if necessary.
- Provide any Additional Comments and recommendations noted during your appointment.
- Finally, ensure the form is signed by a Physician, including their name, signature, date, address, and phone number.
What You Should Know About This Form
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to gather essential health information about an individual before their medical appointment. By completing the form, patients ensure that healthcare providers have all necessary details regarding their medical history, current medications, and any significant health conditions. This information helps in providing a comprehensive and effective evaluation during the visit.
Who should complete the Annual Physical Examination form?
It is recommended that the individual who is undergoing the examination complete the form. If the person is unable to do so, an accompanying person may fill it out on their behalf. However, it is vital to ensure that the information provided is accurate and thorough, as this will directly impact the quality of care received during the physical exam.
What details are required under 'Diagnoses/Significant Health Conditions'?
This section requests a summary of the individual’s medical history, including any chronic or significant health problems they may have. If the patient has previous health records or lists of chronic conditions, they should include them with the form. This allows the healthcare provider to understand the patient’s health status better and identify any necessary follow-up actions.
Are current medications and allergies necessary to include, and why?
Yes, it is crucial to include all current medications along with doses and prescribing physicians. This information helps the provider understand potential interactions during treatment. Additionally, listing any known allergies or sensitivities is essential to prevent adverse reactions during medical assessments or procedures.
How often should immunizations be updated, and what should be included?
Immunizations should be updated as per the recommended schedule for each vaccine. This section of the form allows individuals to record dates and types of vaccines received, including tetanus, hepatitis B, and flu shots. Keeping this information current is essential for overall health and community safety.
What is the significance of tuberculosis (TB) screening?
The TB screening is essential to identify whether an individual has been exposed to the tuberculosis bacteria. This screening should be done every two years using the Mantoux method. If results are positive, a follow-up chest x-ray is usually necessary. Addressing TB is vital for both personal and public health.
What is meant by ‘Evaluation of Systems’ in the physical examination section?
The 'Evaluation of Systems' section allows the healthcare provider to assess different body systems and determine if they are functioning normally. The patient should indicate whether they have experienced any issues with each system. This comprehensive evaluation helps detect any underlying health concerns that may need further examination.
What are recommended health maintenance practices?
Health maintenance practices include a variety of recommendations based on the individual’s needs. These may involve scheduling regular lab work or tests, engaging in appropriate treatment or therapies, and maintaining physical activity and proper hygiene. Adequate weight management and a balanced diet are also crucial for overall health. This information contributes to a well-rounded approach to health care.
What should be done if there is a change in health status from the previous year?
If there has been a change in health status, this should be clearly indicated on the form. Patients should specify what changes have occurred. This transparency allows healthcare providers to address new health issues promptly and adjust the care plan accordingly.
How is the recommendation for ICF/ID level of care determined?
The recommendation for ICF/ID level of care is based on comprehensive assessments of the individual’s health needs and daily functioning capabilities. A qualified healthcare professional will evaluate whether the individual meets the necessary criteria. If the recommendation is applicable, it helps ensure that they receive appropriate support and services tailored to their needs.
Common mistakes
Filling out the Annual Physical Examination form is crucial for accurate medical assessments. However, many individuals make mistakes that can lead to delays or incomplete medical evaluations. One common mistake is failing to provide full personal information. For instance, leaving out the date of birth or address can result in complications during scheduling or billing.
Another frequent error involves skipping critical questions about current medications. People often forget to list all medications they are taking, including over-the-counter drugs, which can affect treatment decisions. It is essential to present a complete list, including dosages and prescribing physicians, to ensure proper care.
Many individuals also misreport their allergies or sensitivities. This information is vital for avoiding adverse reactions during treatment. Incomplete or inaccurate reporting can lead to severe health risks that can be easily avoided with careful attention to this section.
The immunization section is another area prone to mistakes. Individuals may not remember the exact dates of their vaccines, leading to gaps in important medical history. It's beneficial to keep personal health records updated or consult previous medical documentation before filling out this section.
Some people might overlook answering the question about being free of communicable diseases. This can be a significant oversight, as it directly impacts the safety of others in the clinic. If someone does have a communicable disease, it’s essential to detail precautions to mitigate any risks of spreading illness.
Additionally, not including previous hospitalizations or surgical procedures can leave the medical team unprepared for any complications. Being as thorough as possible helps the healthcare provider understand the patient's background and current health status.
Another mistake is neglecting the evaluation of systems section. Respondents may tick “Yes” or “No” without providing valuable comments or additional details about their health. This lack of information could hinder a thorough understanding of the patient’s overall health.
Lastly, some forms may not be signed or dated properly. Failing to do so can result in the form being invalidated, causing unnecessary delays in medical appointments. A complete and accurately signed form is crucial for timely treatment and service.
Documents used along the form
The Annual Physical Examination form is a critical document in healthcare, serving as a comprehensive overview of an individual's health status. Several other forms and documents often accompany it, ensuring a smooth interaction between patients and healthcare providers. Below is a list of commonly used forms that enhance the evaluation process and support effective patient care.
- Medical History Form: This document gathers detailed information about a patient's past medical issues, surgeries, family health history, and allergies. It helps physicians understand risk factors and tailor treatment plans accordingly.
- Immunization Records: This form tracks a patient’s vaccination history, ensuring they are up-to-date on essential immunizations. It is essential for preventing diseases and can also be required for school or employment.
- Medication Reconciliation Form: This document lists all current medications being taken by the patient. It serves to prevent drug interactions and ensure safe prescribing practices by allowing healthcare providers to understand their patients' medication regimens fully.
- Referral Form: When a primary care physician deems it necessary, this form facilitates referrals to specialists. It includes relevant patient information and the reason for referral, ensuring specialists have adequate background data.
- Insurance Information Form: This form collects pertinent health insurance details from the patient. It is crucial for processing claims and ensuring coverage for the services provided during the appointment.
- Follow-Up Care Instructions: After an examination, this document outlines recommended next steps for the patient, including follow-up appointments, additional tests, or lifestyle modifications. Proper instructions guide patients in managing their health effectively.
Each of these forms plays a vital role in the overall healthcare process. Together, they ensure that healthcare professionals have the information they need to offer the best care possible. By understanding the purpose of each document, patients can engage more effectively in their healthcare journey.
Similar forms
New Patient Intake Form: Similar to the Annual Physical Examination form, the New Patient Intake Form gathers essential information about a patient before their first appointment. It typically includes personal details like name, contact information, insurance information, and medical history. This ensures that the healthcare provider has the necessary information to address the patient’s needs right from the start.
Emergency Medical Form: This document is used to provide critical health information in emergency situations. Like the Annual Physical Examination form, it encompasses medical history, current medications, allergies, and significant health conditions. It’s especially important for ensuring that appropriate care is given without delay.
Referral Form: A referral form is similar as it includes detailed health history pertinent to specific specialists. It usually requires the provider to note current medications, diagnoses, and any relevant tests or examinations. This continuity of information helps specialists understand the patient's health background before the appointment.
Physical Activity Readiness Questionnaire (PAR-Q): Like the Annual Physical Examination form, the PAR-Q assesses a person’s readiness for physical activity. It gathers information on health history and any potential risks associated with exercise, ensuring that individuals are aware of their health status before engaging in fitness activities.
Medication List: This document is akin to the Annual Physical Examination form in that it provides a comprehensive account of all medications a patient is currently taking. It includes details such as dosage and frequency, helping healthcare providers manage prescriptions, assess interactions, and monitor treatment effectiveness.
Dos and Don'ts
Do's when filling out the Annual Physical Examination form:
- Complete all sections of the form to avoid return visits.
- Provide detailed medical history, including any chronic health problems.
- List all current medications, including dosages and frequency.
- Note any allergies or sensitivities clearly.
- Update immunization records accurately.
- Indicate whether the individual takes medications independently.
- Be honest about any communicable diseases.
- Ensure the physician’s signature and date are included at the end.
Don'ts when filling out the Annual Physical Examination form:
- Do not leave sections blank if possible; incomplete forms may be returned.
- Avoid using vague terms; specificity is crucial for health records.
- Do not forget to attach additional pages if needed for medications or medical history.
- Do not omit important health conditions that could affect diagnosis.
- Refrain from using abbreviations or shorthand in descriptions.
- Do not disregard prior medical evaluations; reference them if necessary.
- Avoid altering the form or overwriting sections; use clear corrections instead.
- Do not submit the form without reviewing all entries for accuracy.
Misconceptions
Misconceptions about the Annual Physical Examination form can lead to confusion. Here are some common misunderstandings:
- It’s just a formality. Many people think the annual exam is merely a routine procedure with little value. In reality, it plays a crucial role in preventive healthcare, helping to identify potential health issues before they become serious.
- Only unhealthy people need an annual exam. This is incorrect. Annual exams are essential for everyone, regardless of their current health status. They help maintain health and catch any changes early.
- The form is not important. While some may view the form as unimportant paperwork, it provides vital information for healthcare providers to assess an individual’s health accurately.
- All information is optional. Most sections of the form are essential to ensure comprehensive care. Providing complete information can help prevent unnecessary return visits.
- You don’t need to prepare before the appointment. Preparation is crucial. Collecting medical history, medication lists, and any relevant tests can make the visit more productive.
- The exam results are immediate. Some results, especially lab tests, may take time to process. Follow-up appointments are common for discussing findings and next steps.
- Annual exams only focus on physical health. These exams also address mental and emotional health, nutrition, and lifestyle choices, which are vital for overall well-being.
- If you feel fine, you can skip the form. Feeling healthy doesn’t mean you shouldn’t complete the form. Many health issues can be asymptomatic, making regular exams important for everyone.
Understanding these misconceptions about the Annual Physical Examination form can help individuals take charge of their healthcare more effectively. Remember, knowledge is key to staying healthy!
Key takeaways
Completing the Annual Physical Examination form entirely ensures a smoother appointment process, reducing the likelihood of needing return visits.
Prior to the medical appointment, include personal information such as name, address, and date of birth, as well as any significant health conditions or diagnoses.
List all current medications and dosages accurately. Attach additional pages if necessary to provide complete information to the healthcare provider.
Immunization records are vital. Include dates and types of vaccines received, as this information impacts overall health assessments and recommendations.
Document any previous hospitalizations or surgical procedures to give the physician a comprehensive view of your medical history.
Ensure evaluation of systems is thorough. Indicate any normal findings or concerns which may assist the physician in their examination.
After the examination, review recommendations for health maintenance, including lab work, exercise, and dietary instructions, to optimize health moving forward.
Browse Other Templates
Coastal Bend Academic Record Request,Coastal Bend Transcript Application,Coastal Bend Student Record Retrieval,Coastal Bend Transcript Order Form,Coastal Bend Official Transcript Request,Coastal Bend Educational Record Request,Coastal Bend Transcript - Keep the college informed of any changes to your contact information.
Vit Tax - Instructions for completing the form are included to ensure clarity for the dealer.