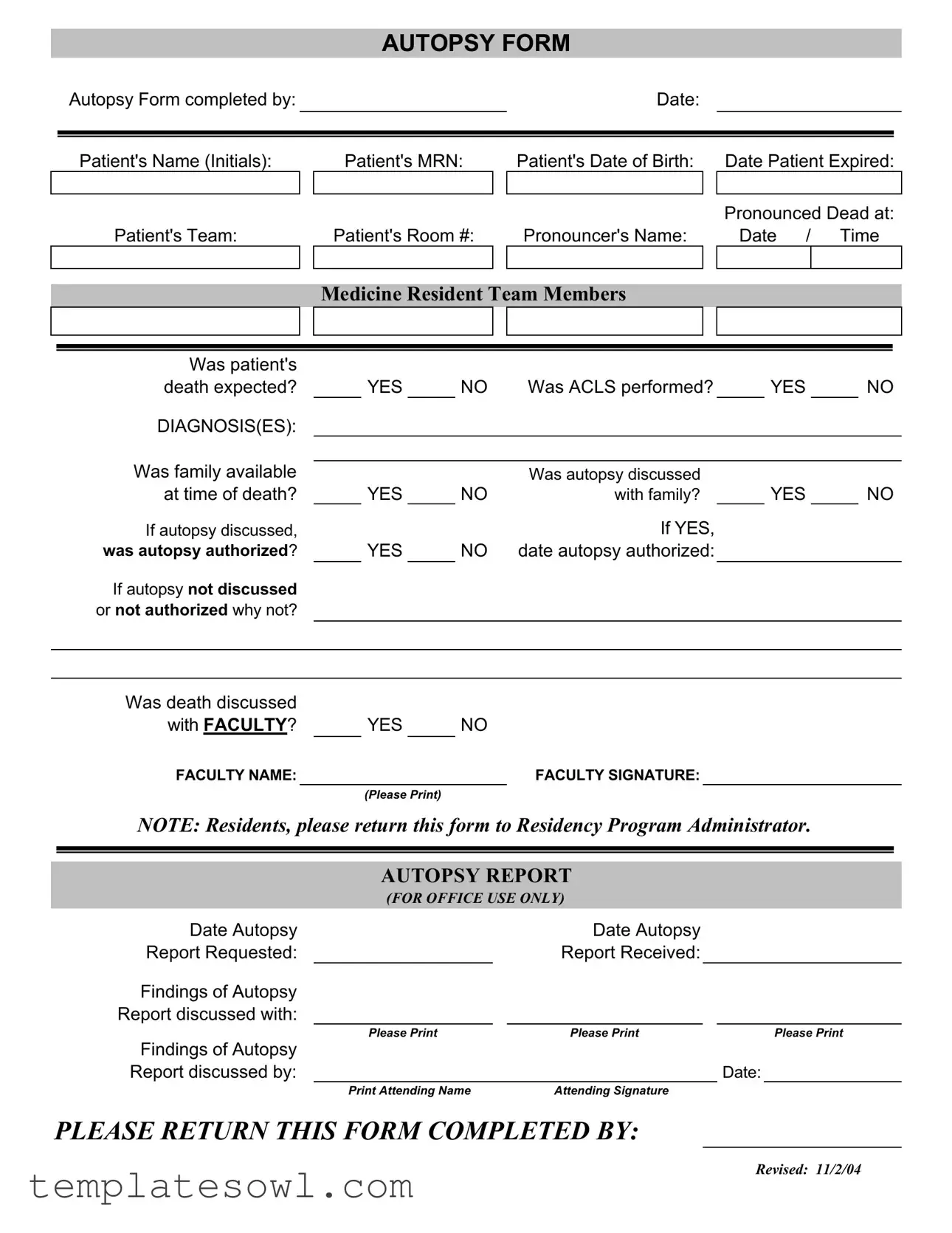
Fill Out Your Autopsy Report Form
The Autopsy Report form plays a crucial role in the post-mortem process, ensuring that the necessary details surrounding a patient's death are thoroughly documented. Every section of the form is designed to capture essential information, beginning with the patient's basic details like name, medical record number, and date of birth. This foundational data culminates with important timing notes, including when the patient expired and when they were pronounced dead. Understanding whether the death was expected or if advanced cardiac life support (ACLS) was performed is vital in assessing the scenario. The form also facilitates communication about whether the autopsy was discussed with the family and if they provided authorization for it. Additional sections ask about the involvement of faculty members and require their signatures, underscoring the collaborative nature of this process. For accurate record-keeping, the form includes distinct sections for both resident and faculty inputs, emphasizing the importance of documentation at every step. Each entry is necessary not just for legal compliance, but also for medical education and advancing our understanding of causes of death.
Autopsy Report Example
AUTOPSY FORM
Autopsy Form completed by: |
|
|
|
Date: |
|
|
|
|
|
|
|
|
|
|
|
Patient's Name (Initials): |
|
Patient's MRN: |
Patient's Date of Birth: |
|
Date Patient Expired: |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Pronounced Dead at: |
|
Patient's Team: |
|
Patient's Room #: |
Pronouncer's Name: |
|
Date / Time |
||
|
|
|
|
|
|
|
|
MEDICINE RESIDENT TEAM MEMBERS
Was patient's |
|
|
|
|
|
|
|
|
|
death expected? |
|
YES |
|
NO |
Was ACLS performed? |
|
YES |
|
NO |
DIAGNOSIS(ES): |
|
|
|
|
|
|
|
|
|
Was family available |
|
|
|
|
|
|
|
|
|
|
|
|
|
Was autopsy discussed |
|
|
|
|
|
at time of death? |
|
YES |
|
NO |
with family? |
|
YES |
|
NO |
If autopsy discussed, |
|
|
|
|
If YES, |
|
|
|
|
was autopsy authorized? |
|
YES |
|
NO |
date autopsy authorized: |
|
|
|
|
If autopsy not discussed |
|
|
|
|
|
|
|
|
|
or not authorized why not? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Was death discussed |
|
|
|
|
|
|
with FACULTY? |
|
YES |
NO |
|||
FACULTY NAME: |
|
|
|
|
FACULTY SIGNATURE: |
|
|
|
|
(Please Print) |
|
|
|
NOTE: Residents, please return this form to Residency Program Administrator.
AUTOPSY REPORT
(FOR OFFICE USE ONLY)
Date Autopsy |
|
Date Autopsy |
|
|
|
|
||
Report Requested: |
|
|
Report Received: |
|
|
|
|
|
Findings of Autopsy |
|
|
|
|
|
|
|
|
Report discussed with: |
|
|
|
|
|
|
|
|
|
Please Print |
|
Please Print |
|
|
|
Please Print |
|
Findings of Autopsy |
|
|
|
|
|
|
|
|
Report discussed by: |
|
|
|
|
|
Date: |
||
|
Print Attending Name |
|
Attending Signature |
|
|
|
|
|
PLEASE RETURN THIS FORM COMPLETED BY:
Revised: 11/2/04
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Purpose | The Autopsy Report form serves to document the circumstances surrounding a patient's death and the subsequent autopsy findings. |
| Completion Date | The form must be completed by a designated medical professional on the same day as the autopsy or shortly thereafter to ensure accurate documentation. |
| Patient Information | Critical details including the patient's name, medical record number, date of birth, and date of death must be recorded to maintain accurate identification. |
| Consent for Autopsy | Discussion of the autopsy with the family is essential. If consent is obtained, it is recorded on the form. In cases where consent is not given, there should be a note explaining the reason. |
| Involvement of Faculty | The form incorporates a section to confirm whether the death was discussed with faculty members, emphasizing the collaborative nature of patient care and decision-making. |
| State-Specific Regulations | In many states, specific laws regulate the performance of autopsies and the use of these forms. For example, California Health and Safety Code Section 102800 governs autopsy practices in California. |
Guidelines on Utilizing Autopsy Report
Completing the Autopsy Report form requires careful attention to detail. Each section must be filled out accurately to ensure proper documentation. After completing this form, it will need to be submitted according to the instructions provided by your specific institution.
- Fill in the name of the individual completing the form under Autopsy Form completed by:.
- Enter the date the form is being completed.
- Provide the patient's full name or initials.
- Input the patient's Medical Record Number (MRN).
- Remember to include the patient's date of birth.
- Document the date the patient expired.
- Indicate the time the patient was pronounced dead.
- List the patient's healthcare team.
- Write the patient's room number.
- Provide the pronouncer's name.
- Fill in the date and time of the report.
- Answer whether the patient's death was expected by marking YES or NO.
- Note if Advanced Cardiac Life Support (ACLS) was performed (YES or NO).
- List any diagnoses related to the patient.
- Indicate whether the family was available at the time of death (YES or NO).
- State if the autopsy was discussed with the family (YES or NO).
- If it was discussed, indicate if the autopsy was authorized (YES or NO).
- If authorized, enter the date it was authorized.
- If not discussed or authorized, explain the reason.
- Document whether death was discussed with faculty (YES or NO).
- Provide the faculty's name.
- Collect the faculty's signature (please print their name as required).
- Complete any additional requests if noted in the NOTE section.
Upon completion, ensure that the form is returned to the designated Residency Program Administrator as stated on the form. This will ensure that the necessary protocols are followed and that everything is processed correctly.
What You Should Know About This Form
What information is required to complete the Autopsy Report Form?
To complete the Autopsy Report Form, several key details must be provided. You'll start with basic patient information, such as the patient's name or initials, Medical Record Number (MRN), date of birth, date of expiration, and the time they were pronounced dead. Additionally, information regarding the medical team and the patient's room number goes on the form. It's important to document whether the death was expected and if Advanced Cardiac Life Support (ACLS) was performed. The form also includes questions about family involvement, discussions regarding the autopsy, and any authorization provided.
How do I know if an autopsy was discussed and authorized?
The Autopsy Report Form contains specific sections to clarify whether an autopsy was discussed with the family at the time of death. You must indicate ‘YES’ or ‘NO’ in the relevant boxes. If the autopsy was discussed, you also need to confirm if it was authorized. This is vital to ensure transparency and to respect the family's wishes. If the autopsy wasn't discussed or authorized, space is provided to explain the reasons for this decision.
Who should return the completed Autopsy Report Form?
The completed Autopsy Report Form should be returned to the Residency Program Administrator by the residents who filled it out. This ensures that the information is processed correctly and documented within the residency program’s system.
How are autopsy findings communicated to the appropriate parties?
Once the autopsy is performed, findings are documented in the Autopsy Report. The completed report will be reviewed and discussed with designated parties. The form includes sections for recording the names of those with whom the findings were discussed, as well as the attending physician who led the discussion. This process helps to ensure that vital information is shared and understood by all involved in the patient's care.
Common mistakes
Completing the Autopsy Report form may seem straightforward, yet there are common mistakes that can complicate the process. One of the frequent errors is failing to fill in all required fields. Omitting essential information such as the Patient's Name or Pronouncer's Name can create unnecessary delays in processing the report.
Another common mistake involves unclear or illegible handwriting. Ensure that all entries are written clearly. If the information cannot be read, it may lead to confusion and miscommunication. Using printed text, when possible, can help alleviate this issue.
Many forget to indicate whether the patient's death was expected. This detail is crucial for the context of the autopsy. Indicating YES or NO in the respective checkbox provides important insights into the circumstances surrounding the patient's passing.
When discussing the autopsy with the family, documentation is key. Failing to note whether the autopsy was discussed with the family can create misunderstandings. It is important to record if the family was present and if they authorized the autopsy.
Another mistake involves neglecting to document the date of authorization for the autopsy when it has been discussed and approved. Without this date, the timeline of events surrounding the autopsy may become unclear.
Individuals sometimes skip the section regarding whether the death was discussed with faculty. This could be crucial in ensuring that the proper protocols were followed. It is essential to indicate whether faculty members were involved in the conversation.
Inaccuracies in the Attending Name or Signature may also lead to delays. The attending physician's details must be correct to ensure accountability and follow-up. Ensure that this section is completed accurately and clearly.
Some forget to return the form to the Residency Program Administrator. This step is critical. Not submitting the document promptly can hinder the administrative process and affect the overall autopsy timeline.
Finally, ensure that you are using the correct version of the form. Revisions, like the one dated 11/2/04, should always be referenced to avoid using outdated information. Keeping up-to-date on form versions ensures compliance with the latest protocols.
Documents used along the form
The Autopsy Report form is often accompanied by several other important documents that provide necessary information during the investigation of a patient's death. Each of these documents serves a specific purpose to ensure that all aspects of the autopsy process are properly recorded and communicated. Below are some commonly used forms and documents associated with the Autopsy Report.
- Death Certificate: This official document validates the occurrence of a death. It includes vital details such as the cause of death, date of death, and personal information about the deceased. It is essential for legal and administrative purposes.
- Consent for Autopsy: This form records the family’s approval for the autopsy. It ensures that the legal rights of the deceased and their loved ones are respected during the autopsy process.
- Medical History Form: This document contains the patient's previous medical records, treatments, and any relevant health information. It helps the medical team understand background factors that could have contributed to the death.
- Pathology Report: After the autopsy, a detailed pathology report is generated. This document outlines the findings and conclusions drawn from the examination of tissues and organs. It is crucial for diagnosis and understanding the cause of death.
- Family Discussion Notes: This document records notes from conversations held with the family regarding the autopsy process and findings. It ensures that family members are kept informed and their concerns are noted.
- Follow-Up Report: In some cases, a follow-up report may be issued after the autopsy. This document may address additional findings or clarify elements related to the cause of death, providing essential updates to both medical staff and the family.
Using these documents alongside the Autopsy Report ensures a thorough and respectful process when determining the circumstances of a patient’s death. By maintaining accurate records, healthcare providers support accountability and transparency in medical practices.
Similar forms
- Death Certificate: This document serves as the official record of a person's death. Like the autopsy report, it contains critical information such as the date of death, medical condition at the time of death, and determining cause. Both documents are essential in the legal and medical communities for confirming a death.
- Clinical Report: The clinical report details a patient's medical history and the circumstances leading to hospitalization. Similar to the autopsy report, it provides insights into the patient's condition before death, including diagnoses and treatment received, contributing to the understanding of the causative factors in demise.
- Coroner's Report: Issued by the coroner, this report investigates the manner and cause of death, often in cases of sudden or unexplained death. Both documents aim to elucidate the circumstances surrounding a death, though the coroner's report typically involves more extensive investigative procedures.
- Pathology Report: This document contains findings from the examination of tissue samples, aiding in disease diagnosis. Similar to the autopsy report, the pathology report reports on findings that can explain the cause of death and contribute to medical knowledge.
- Medical Examiner's Report: Like the autopsy report, this document results from an examination performed by a medical examiner to ascertain the cause of death, particularly in cases that are suspicious or require further investigation. It includes similar details about medical history and circumstances of death.
- Informed Consent Form: Although primarily focused on patient care and ethical considerations, this form documents the patient's or family's understanding of procedures, including autopsies. It parallels the autopsy report in that both require a clear communication process between the medical team and the family regarding treatment decisions.
- Family Discussion Notes: These notes summarize conversations held with a patient's family regarding the death and autopsy implications. Similar to the autopsy report, they reflect the emotional and procedural aspects involved in managing a patient's end-of-life care and have significant importance for documentation in medical records.
Dos and Don'ts
When filling out the Autopsy Report form, it is essential to ensure accuracy and clarity. Here is a list of practices to embrace and avoid:
- Do: Provide complete and accurate patient information, such as the patient's name, date of birth, and MRN.
- Do: Clearly indicate whether the death was expected and if the family was informed about the autopsy.
- Do: Ensure that all required signatures are obtained, including those from faculty members and the resident team.
- Do: Return the completed form to the designated Residency Program Administrator promptly.
- Do: Maintain confidentiality and handle the report with sensitivity towards the family’s situation.
- Don't: Do not leave any fields blank unless specifically instructed; incomplete forms can delay the process.
- Don't: Avoid using abbreviations or informal language that may cause confusion for those reviewing the report.
- Don't: Do not discuss sensitive details of the case with unauthorized individuals.
- Don't: Refrain from altering any information once it has been submitted; this could lead to miscommunication.
- Don't: Avoid procrastinating when it comes to filling out and returning the form; timely submission is critical.
Misconceptions
- Autopsy reports are only for criminal cases. Many believe that autopsies are only performed in suspicious deaths; however, they can provide valuable information in a variety of circumstances, including natural deaths, to better understand a patient's medical history.
- Autopsy reports are always lengthy and detailed. While some autopsy reports can be comprehensive, they vary in length and detail based on the case. In some instances, a brief report suffices, depending on what is discovered during the examination.
- Families must give permission for an autopsy. In most cases, the consent of the family is necessary. However, there are exceptions, particularly in cases where public health is at stake or whenever forensic autopsies are required by law.
- All autopsies are conducted for the same reasons. There are different types of autopsies, such as clinical, forensic, and medicolegal. Each type serves distinct purposes and is performed under different circumstances.
- Autopsy results are only relevant to the medical community. While the information is vital for medical practitioners, families also benefit. Results can provide closure and answers about the cause of death.
- Once an autopsy is requested, it must be performed. A request for an autopsy can indeed be made, but it is not mandatory. Factors like family consent and other considerations play critical roles in the decision to proceed.
- Autopsy findings are always conclusive. Even though an autopsy can shed light on many aspects of a death, it is essential to understand that findings may sometimes be inconclusive, requiring further investigation.
- All autopsy reports look the same. Autopsy reports can differ significantly depending on the institution, the specific circumstances of the death, and the protocols followed by the medical team involved.
- Only medical professionals can understand autopsy reports. While some medical terminology may be included, autopsy reports can be summarized and explained in simpler terms, making the findings accessible to families.
- Autopsy reports are not confidential. Protecting patient privacy is essential. Autopsy reports are considered confidential medical documents and subject to privacy regulations, ensuring that personal information remains secure.
Key takeaways
1. Ensure all fields are accurately filled out, including the patient's details and date of expiration.
2. Indicate whether the death was expected and if Advanced Cardiovascular Life Support (ACLS) was performed.
3. Clearly state any diagnoses related to the patient's condition.
4. Record if the autopsy was discussed with the family, and confirm their availability during discussions.
5. If an autopsy was discussed, document whether it was authorized and note the date of authorization.
6. If no discussion occurred or authorization was not granted, provide a reason for this decision.
7. Confirm if the patient's death was reviewed with faculty, and include the faculty's name and signature.
8. For office use, record the dates related to the autopsy and the receipt of the autopsy report.
9. After completing the form, return it promptly to the Residency Program Administrator for processing.
Browse Other Templates
How Old Do You Have to Be to Get a Ged in Michigan - Retain a copy of the form for your records after sending.
Michigan Health Appraisal Form - The completion of this form is a collaborative effort to uphold children's health and education standards.