Fill Out Your Biopsychosocial Assessment Social Work Form
The Biopsychosocial Assessment Social Work form plays a vital role in understanding an individual's overall well-being by examining various aspects of their life. At its core, this assessment gathers essential information about a person's mental, physical, and social health, paving the way for tailored interventions. Initially, it prompts individuals to share the presenting problem that brought them to seek help, along with information on how long they've been experiencing these challenges. The form encourages a self-reflective process as individuals rate the intensity of their problems and articulate how these issues disrupt their daily functioning. Additionally, it provides space for personal goals for therapy, helping to create a roadmap for their treatment journey. The assessment also delves into mental health symptoms, relationships, education, legal issues, and work history, offering a comprehensive view of the factors affecting the individual. By documenting a person’s medical history, including past treatments and current health concerns, the form ensures that social workers can approach each case holistically. Moreover, sections addressing substance use, family dynamics, and trauma provide critical context that influences a person’s journey towards healing.
Biopsychosocial Assessment Social Work Example
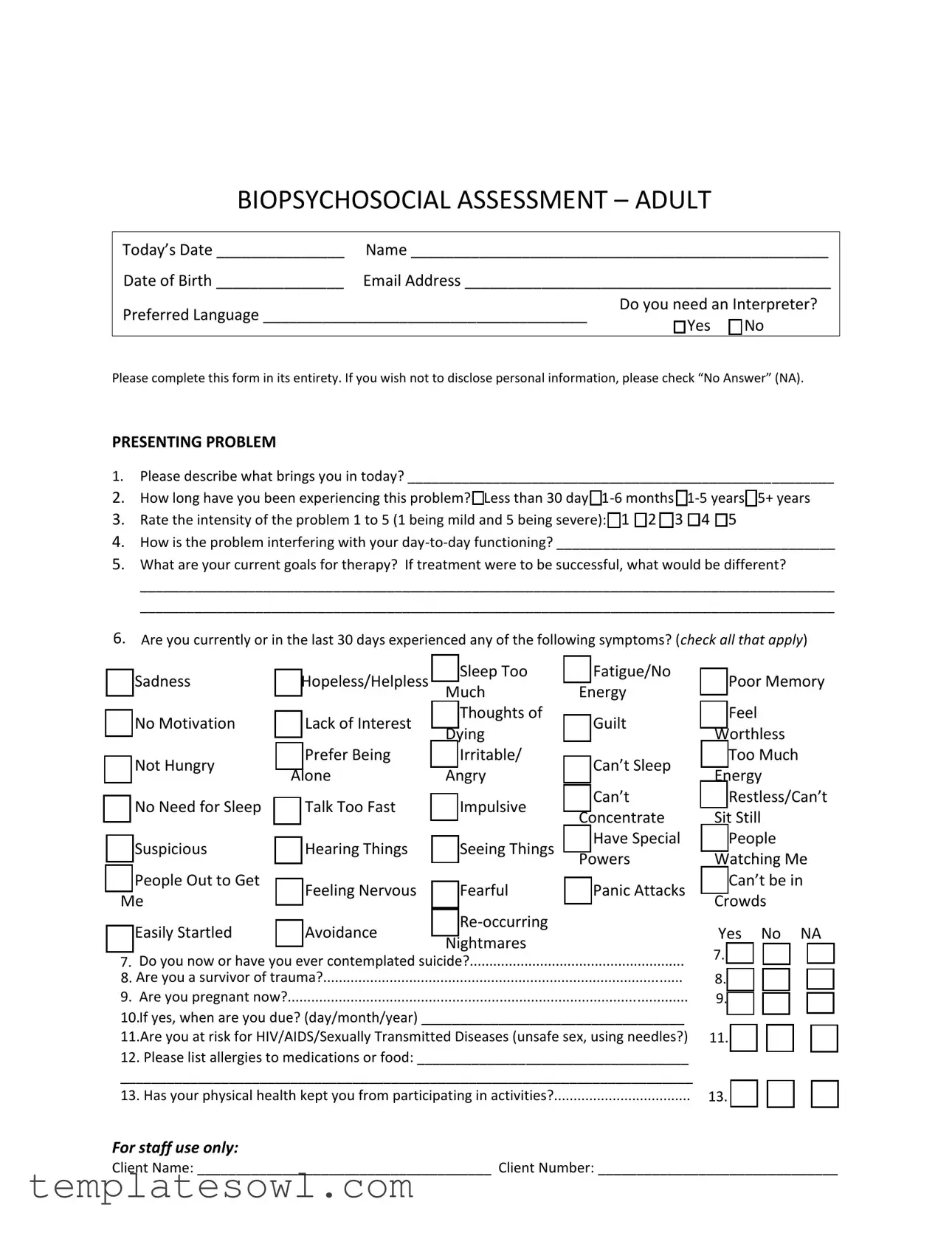
BIOPSYCHOSOCIAL ASSESSMENT – ADULT
Today’s Date _______________ |
Name _________________________________________________ |
Date of Birth _______________ |
Email Address ___________________________________________ |
Preferred Language ______________________________________ |
Do you need an Interpreter? |
|
□ Yes □ No |
||
|
Please complete this form in its entirety. If you wish not to disclose personal information, please check “No Answer” (NA).
PRESENTING PROBLEM
1.Please describe what brings you in today? _______________________________________________________
2.How long have you been experiencing this problem? □Less than 30 day
3.Rate the intensity of the problem 1 to 5 (1 being mild and 5 being severe): □1 □2 □3 □4 □5
4.How is the problem interfering with your
5.What are your current goals for therapy? If treatment were to be successful, what would be different?
__________________________________________________________________________________________
__________________________________________________________________________________________
6.Are you currently or in the last 30 days experienced any of the following symptoms? (check all that apply)
□Sadness
□No Motivation
□Not Hungry
□No Need for Sleep
□Suspicious
□People Out to Get
Me
□Easily Startled
□Hopeless/Helpless |
□ Sleep Too |
□ Fatigue/No |
|
|
Much |
Energy |
|
□ Lack of Interest |
□ Thoughts of |
□ Guilt |
|
Dying |
|||
|
|
||
□ Prefer Being |
□ Irritable/ |
□ Can’t Sleep |
|
Alone |
Angry |
||
|
|||
□ Talk Too Fast |
□ Impulsive |
□ Can’t |
|
Concentrate |
|||
|
|
||
□ Hearing Things |
□ Seeing Things |
□ Have Special |
|
Powers |
|||
|
|
||
□ Feeling Nervous |
□ Fearful |
□ Panic Attacks |
|
□ Avoidance |
□ |
|
|
Nightmares |
|
||
|
|
□Poor Memory
□Feel
Worthless
□Too Much
Energy
□Restless/Can’t
Sit Still
□People
Watching Me
□Can’t be in Crowds
Yes No NA |
7. Do you now or have you ever contemplated suicide?.......................................................
8. Are you a survivor of trauma?............................................................................................
9. Are you pregnant now?......................................................................................................
10.If yes, when are you due? (day/month/year) __________________________________
11.Are you at risk for HIV/AIDS/Sexually Transmitted Diseases (unsafe sex, using needles?)
12. Please list allergies to medications or food: ___________________________________
__________________________________________________________________________
13. Has your physical health kept you from participating in activities?...................................
7. |
□ |
□ |
□ |
8. |
□ |
□ |
□ |
9. |
□ |
□ |
□ |
11. |
□ |
□ |
□ |
13. |
□ |
□ |
□ |
For staff use only:
Client Name: ______________________________________ Client Number: _______________________________
TOBACCO |
|
Yes |
No |
NA |
1. Have you ever used any forms of tobacco (cigarettes, snuff, etc.)? IF NO SKIP TO NEXT |
1. |
□ |
□ |
□ |
SECTION……………………………………………………………………………………………………………………………… |
|
|
|
|
2. Are you a former tobacco user? |
2. |
□ |
□ |
□ |
3.If yes, what form(s) of tobacco have you used in the past (please check all that apply)
□ Cigarettes □ Cigars □ Snuff □ Chewing Tobacco □ Snuff □ Other
4.How many times on an average day do you use tobacco
Cigarettes____ Cigars____ Snuff____ Chewing Tobacco____ Snuff____ |
|
|
|
|
5. Have you been involved in a program to help you quit using tobacco in the past 30 |
5. |
□ |
□ |
□ |
days? |
|
|
|
|
6. If so, which |
|
|
|
|
SUBSTANCE USE/ADDICTION PRESENT |
|
Yes |
No |
NA |
1. Would you or someone you know say you are having a problem with alcohol?......………… |
1. |
□ |
□ |
□ |
2. Would you or someone you know say you are having problems with pills or illegal |
2. |
□ |
□ |
□ |
drugs? |
|
|
|
|
3. Would you or someone you know say you are having problems with other addictions, ie. |
3. |
□ |
□ |
□ |
gambling, pornography or shopping? |
|
|
|
|
4. Have you ever been to a |
4. |
□ |
□ |
□ |
SUBSTANCE USE/ADDICTION PAST |
|
Yes |
No |
NA |
1. Would you or someone you know say you had a problem with alcohol?......…………………… |
1. |
□ |
□ |
□ |
2. Would you or someone you know say you had problems with pills or illegal drugs? |
2. |
□ |
□ |
□ |
3. Would you or someone you know say you had problems with other addictions, ie. |
3. |
□ |
□ |
□ |
gambling, pornography or shopping? |
|
|
|
|
4. Is there a family history of addiction in your family? |
4. |
□ |
□ |
□ |
5. If yes, please describe: _____________________________________________________ |
|
|
|
|
PERSONAL, FAMILY AND RELATIONSHIPS |
|
Yes |
No |
NA |
1.Who is in your family? (parents, brothers, sisters, children, etc.)____________________
__________________________________________________________________________
2. |
Has there been any significant person or family member enter or leave your life in the |
2. □ |
□ |
□ |
|||||
last 90 days? |
|
|
|
|
|
|
|||
|
|
Good Fair Poor Close Stressful Distant Other |
|||||||
3. |
How are the relationships in your family? |
□ |
□ |
□ |
□ |
□ |
□ |
□ |
|
4. |
How are the relationships in your support system (friends, |
□ |
□ |
□ |
□ |
□ |
□ |
□ |
|
extended family, et.?)………………………………………………………………. |
|||||||||
|
|
|
|
|
|
|
|||
|
|
|
|
Conflict Abuse Stress Loss Other |
|||||
5. |
Are there any problems in your family now? (check all that apply)………….. |
□ |
□ |
□ |
□ |
□ |
|||
6. |
Were there any problems with your family in the past? (check all that |
|
□ |
□ |
□ |
□ |
□ |
||
apply)…………………………………………………………………………………………………………... |
|
|
|
|
|
||||
7. Are there any problems in your support system now? (check all that |
|
□ |
□ |
□ |
□ |
□ |
|||
apply)…………………………………………………………………………………………………………… |
|
|
|
|
|
||||
8. Were there any problems with your support system in the past? (check |
□ |
□ |
□ |
□ |
□ |
||||
all that apply)………………………………………………………………………………………………. |
|
|
|
|
|
||||
9.What is your marital status now? □Single □Married □Living as Married □Divorced □Widowed □Never Married
For staff use only:
Client Name: ______________________________________ Client Number: _______________________________
10.Have you ever had problems with marriage/relationships?..............................................
11.If yes, please check why: □Stress □Conflict □Loss □Divorced/Separation
□Trust Issues □Other_______________________________
12.Do you have any close friends?..........................................................................................
13.Do you have problems with friendships?...........................................................................
14.Do you get along well with others (neighbors,
15.What do you like to do for fun? _____________________________________________
Yes |
No |
NA |
10. □ |
□ |
□ |
12. □ |
□ |
□ |
13. □ |
□ |
□ |
14. □ |
□ |
□ |
EDUCATION
1.What is the highest grad you completed in school? (please check)
□No Education
2.Would you describe your school experience as positive or negative?________________
3.Are you currently in school or a training program?..............................................................
Yes No NA
3. □ □ |
□ |
LEGAL
1.Have you ever been arrested? IF NO SKIP TO NEXT SECTION………………………………………….
2.In the past month?...............................................................................................................
3.If yes, how many times? ____________________________________________________
4.In the past year?...................................................................................................................
5.If yes, how many times? ____________________________________________________
6.If yes, what were you arrested for? ___________________________________________
7.What was the name of your attorney? ________________________________________
8.Were you ever sentenced for a crime?…………………………………………………………………………….
9.If yes, number of prison sentences served? ____________________________________
10.What year(s) did this occur? _______________________________________________
11.Are you currently or have you ever been on probation or parole?....................................
12.If yes, what is the name of your attorney or probation officer? ____________________
WORK
1.What is your work history like? □Good □Poor □Sporadic □Other
2.How long do you normally keep a job? □Weeks □Months □Years
3.Are you retired?....................................................................................................................
4.If yes, what kind of work do you do/did you do in the past? _______________________
5.Have you ever served in the military?..................................................................................
6.If yes, are you: □Active □Retired □Other
|
Yes |
No |
NA |
1. |
□ |
□ |
□ |
2. |
□ |
□ |
□ |
4. |
□ |
□ |
□ |
8. |
□ |
□ |
□ |
11. □ |
□ |
□ |
|
|
Yes |
No |
NA |
3. |
□ |
□ |
□ |
5. |
□ |
□ |
□ |
MEDICAL
1.Current Primary Care Physician: __________________________________Phone_________________
2.Past and Current Medical/Surgical Problems: _____________________________________________
3.Past and Current Medications and Dosages: ______________________________________________
__________________________________________________________________________________
4. Have you seen a Mental Health Professional Before? □ Yes □ No
5.If yes, Name, When, and Reason for Changing: ____________________________________________
6.Current Psychiatrist/APRN, if applicable:_________________________________________________
7.Is there anything else you would like me to know about you?_______________________________
__________________________________________________________________________________
For staff use only:
Client Name: ______________________________________ Client Number: _______________________________
Form Characteristics
| Fact Name | Detail |
|---|---|
| Purpose | The Biopsychosocial Assessment form helps social workers understand a client's mental, emotional, and social well-being. |
| Components | The form includes sections on presenting problems, substance use, family relationships, education, legal issues, work history, and medical background. |
| Client Input | Clients are encouraged to answer questions openly, with options for “No Answer” if they prefer not to disclose personal information. |
| Interpretation Needs | There's a specific question addressing the need for an interpreter, highlighting inclusivity for non-English speakers. |
| Therapeutic Goals | The form asks clients to define their goals for therapy, which aids in a focused treatment approach. |
| State Compliance | Different states may require specific legal statutes to be followed; for example, California's Welfare and Institutions Code governs mental health assessments. |
| Confidentiality | Information collected is confidential, aligning with ethical standards for client privacy and data security. |
Guidelines on Utilizing Biopsychosocial Assessment Social Work
Completing the Biopsychosocial Assessment form is an important step in understanding various aspects of your life and situation. Follow these steps to ensure you fill out the form accurately and completely.
- Enter today’s date in the provided space.
- Write your full name on the appropriate line.
- Fill in your date of birth.
- Provide your email address.
- Indicate your preferred language.
- State whether you need an interpreter by selecting "Yes" or "No."
- Answer the question about what brings you in today as clearly as possible.
- Specify how long you have been experiencing the problem by checking the relevant box.
- Rate the intensity of your problem on a scale of 1 to 5.
- Describe how the problem interferes with your daily functioning.
- List your current goals for therapy and what success would look like for you.
- Check all the symptoms you have experienced in the last 30 days.
- Answer the question about contemplating suicide honestly.
- Indicate if you are a survivor of trauma.
- Note if you are currently pregnant and provide your due date if applicable.
- List any allergies to medications or food.
- Answer all questions in the Tobacco section as they apply to you.
- Complete the Substance Use/Addiction sections, marking "Yes," "No," or "NA" as appropriate.
- Describe your personal and family relationships, answering the questions about current problems and family history.
- Provide your marital status and detail any past relationship issues if applicable.
- Answer questions regarding your education and legal history truthfully.
- Fill in your work history and answer the military service question if relevant.
- List your primary care physician and any medical or surgical problems you have had.
- Provide your past and current medications and professional mental health treatment history.
- Finally, mention anything else you think is important for your evaluator to know.
What You Should Know About This Form
What is the purpose of the Biopsychosocial Assessment Social Work form?
The Biopsychosocial Assessment form is designed to gather comprehensive information about an individual's mental, physical, and social health. This information helps social workers develop a better understanding of the client's overall situation. By assessing various aspects of life, including medical history, substance use, relationships, and personal goals, social workers can tailor interventions that address the client's unique needs.
Who should complete the form?
This form is intended for clients seeking social work services. Individuals may complete it themselves or with assistance from a social worker. It is essential that clients provide honest and accurate information to ensure effective support and intervention.
What are the key sections of the Biopsychosocial Assessment?
The assessment includes several sections:
- Presenting Problem
- Tobacco Use
- Substance Use/Addiction
- Personal, Family, and Relationships
- Education
- Legal Issues
- Work History
- Medical Information
What information do I need to provide in the 'Presenting Problem' section?
In this section, clients describe the issues prompting them to seek help. They should specify how long they have been experiencing these problems, rate their intensity, and explain how the problem interferes with daily life. Clients are also encouraged to identify their therapy goals and any symptoms experienced in the previous month.
How is the data from the form used?
The information collected assists social workers in developing a treatment plan that is personalized and effective. It may also be used to evaluate progress over time and adapt interventions as needed.
Can I leave questions unanswered?
Yes, clients may choose to skip any questions they prefer not to answer. They can select "No Answer" (NA) for those questions. However, providing as much relevant information as possible can enhance the effectiveness of the assessment process.
What if I have concerns about privacy?
Confidentiality is a critical aspect of the social work process. All information shared in the assessment is treated with the utmost confidentiality and is only used for the purpose of providing support and services. Clients should feel secure in discussing sensitive topics related to their health and experiences.
Do I need to prepare anything before filling out the form?
While no formal preparation is necessary, it may be helpful to think about recent experiences, health history, and any support systems in place. Clients might want to gather any relevant medical records or information about medications they are currently taking, as this can help make the process smoother.
How can I request assistance in completing the form?
If clients require help with the form, they can ask a social worker for assistance. Additionally, if language barriers exist, clients may request an interpreter before completing the assessment to ensure accurate communication.
What should I do if I encounter sensitive topics or trauma?
Addressing sensitive topics or trauma can be challenging. Clients are encouraged to share only what they feel comfortable discussing. Social workers are trained to handle such topics with sensitivity, and they aim to create a safe space for clients to open up at their own pace.
Common mistakes
Filling out the Biopsychosocial Assessment Social Work form is a crucial step for individuals seeking support. However, there are common mistakes that can hinder the process. One prevalent error is incomplete information. Many people skip sections or provide minimal responses, which can lead to misinterpretation of their needs. It's essential to answer all questions thoroughly. Doing so ensures that social workers have a well-rounded understanding of the individual's situation.
Another frequent issue arises from misunderstanding terminology. Some questions may contain terms that are unfamiliar or overly clinical. If you encounter a term that doesn’t make sense, it’s perfectly acceptable to ask for clarification before you proceed. Providing accurate and clear responses is vital for effective support.
In addition, individuals often fail to consider the importance of honesty when completing the form. It can be tempting to downplay certain issues or omit struggles out of fear or shame. However, being open and honest allows social workers to tailor their approach to better fit one's needs, fostering a supportive environment.
Another common mistake is neglecting to think about past experiences that may influence one's current situation. Many sections of the form ask about family history, relationships, and previous mental health treatment. Reflecting on these aspects before filling out the form can provide valuable insights and help identify patterns that affect one’s well-being.
Lastly, forgetting to review the form before submission is a major pitfall. Take a moment to read through all your responses to ensure they accurately reflect your situation. This final check can catch any inconsistencies or errors, which will ultimately lead to better service and support.
Documents used along the form
The Biopsychosocial Assessment Social Work form is a comprehensive tool used to understand the multifaceted needs of individuals seeking assistance. Alongside this assessment, there are several other documents that provide critical support during the evaluation and treatment planning process. Below is a list of commonly used forms and documents to enhance the understanding of a client’s situation.
- Intake Form: This document collects basic personal information including contact details, demographics, and health history. It helps initial assessment and engagement with the client.
- Release of Information Form: Clients may need to authorize the sharing of their information with other professionals or agencies. This form ensures confidentiality while enabling necessary communication.
- Treatment Plan: Developed after the assessment, this plan outlines specific goals and interventions tailored to the client's needs. It serves as a roadmap for therapy.
- Progress Notes: Clinicians use these notes to document ongoing sessions with clients. They track changes, progress, and any adjustments needed in treatment.
- Risk Assessment Form: This document evaluates a client's risk of harm to themselves or others. It ensures that appropriate safety measures are implemented.
- Demographic Information Form: Collecting information on ethnicity, gender, and socio-economic status helps tailor services and track disparities in treatment access and outcomes.
- Consent for Treatment Form: This form informs clients about the nature of treatment, their rights, and the agreement to receive care. It promotes informed decision-making by clients.
- Crisis Intervention Plan: In case of an emergency, this plan outlines specific steps to be taken to ensure client safety and connection to urgent resources.
Using these forms in conjunction with the Biopsychosocial Assessment provides a well-rounded view of the client, ensuring that their needs are addressed comprehensively. Each document serves a unique purpose, contributing to effective support and intervention.
Similar forms
- Clinical Interview: This document gathers detailed information regarding a client's history, functioning, and current issues. It includes questions about the presenting problems, family dynamics, and support systems, similar to the Biopsychosocial Assessment.
- Intake Form: An Intake Form collects vital personal information, including contact details and basic health history. Like the Biopsychosocial Assessment, it establishes a foundation for understanding the client's needs at the outset of treatment.
- Patient Health Questionnaire (PHQ-9): This tool assesses mental health symptoms, particularly depressive symptoms. It uses a similar format of self-reported surveys to gauge the severity of the client’s psychological state.
- Substance Use Disorder Assessment: This document focuses specifically on substance use history and patterns. It aligns closely with the substance use section of the Biopsychosocial Assessment, aiming to identify problems and potential treatment needs.
- Family Assessment: This form evaluates family dynamics, relationships, and conflicts within the family unit. Much like the Biopsychosocial Assessment, it provides insight into family influences on the client's current situation.
- Strengths and Needs Assessment: This document identifies both the strengths and challenges a client faces, complementing the Biopsychosocial Assessment’s goal of developing a holistic understanding of the client’s life situation.
Dos and Don'ts
When you fill out the Biopsychosocial Assessment Social Work form, it's important to approach the process thoughtfully. Here are some guidelines to help ensure that you complete the form accurately and effectively:
- Do take your time. Filling out this form can be overwhelming. Giving yourself enough time to reflect on each question will help you provide detailed and accurate information.
- Don’t rush through the questions. Each section is designed to help assess your needs. Skipping questions may lead to gaps in understanding your situation.
- Do be honest. Accurate information is crucial for your care. If you are experiencing difficulties, sharing them openly will enable better support.
- Don’t withhold information. If a question makes you uncomfortable, consider that it may still be important. Saying “No Answer” is acceptable, but withholding relevant details can hinder your assessment.
- Do use clear and specific language. The more precise your answers, the easier it will be for those reviewing the form to understand your experiences and needs.
- Don’t ignore the “NA” option. If a question is not applicable to you, mark it accordingly. This helps to prevent confusion later on about which questions are relevant to your situation.
Misconceptions
Understanding the Biopsychosocial Assessment form is crucial for both clients and social workers involved in the therapeutic process. However, several misconceptions can cloud its purpose and interpretation. Here are five common myths:
- It’s just a questionnaire. Many people believe the assessment is merely a list of questions. In reality, it is a comprehensive tool designed to gather vital information about various aspects of a person's life, including emotional, social, and physical factors. This holistic approach helps social workers understand clients more fully.
- Only serious issues need to be reported. Some individuals might think that they should only answer questions pertaining to severe problems, like substance abuse or trauma. Each question is important, regardless of the severity of the issue. Even everyday challenges can greatly impact overall well-being.
- My responses are not confidential. Concerns about privacy often arise when completing this form. However, social workers are bound by strict confidentiality laws. Information shared during the assessment is kept private and only disclosed with the client's consent, ensuring a safe space for open communication.
- It’s only for diagnosing mental health problems. A common misconception is that the Biopsychosocial Assessment is strictly for mental health diagnosis. While it can aid in identifying mental health issues, it also looks at physical health, life circumstances, and social relationships to create a broader understanding of a person's life.
- Filling it out doesn’t influence treatment. Some may think that their information will not impact their therapy. In truth, the insights gathered from this assessment play a crucial role in developing a tailored treatment plan, addressing the unique needs and goals of each client.
Clarifying these misconceptions can foster a better understanding and a more positive experience for clients as they engage with the Biopsychosocial Assessment process.
Key takeaways
The Biopsychosocial Assessment Social Work form serves as a crucial tool for gathering comprehensive information about an individual’s psychological, social, and biological factors. Below are key takeaways regarding its completion and use.
- Full Disclosure: It is important to complete the form in its entirety. In cases where personal information is uncomfortable to disclose, individuals should check “No Answer” (NA).
- Understanding Presenting Problems: Individuals should clearly articulate their presenting problems. This information is vital for the assessment of needs and development of treatment plans.
- Duration and Intensity: The form asks about the length of time individuals have experienced their problems and their intensity level. This information helps in understanding the severity of the issues.
- Interference with Daily Functioning: Those filling out the form must describe how their issues impact day-to-day activities. This may inform the therapist about areas that require immediate attention.
- Identifying Goals: It encourages individuals to outline their current therapy goals. Knowing what success looks like for them is essential in tracking progress during treatment.
- Symptom Checklist: A comprehensive checklist examines various symptoms related to mental health. Individuals should review and select symptoms that resonate with their experiences, which aids therapists in diagnosis.
- Awareness of Trauma and Risk Factors: The assessment includes questions regarding trauma history and current risks, such as suicidal thoughts or substance use. This information is critical in developing a safety plan.
- Highlighting Support Systems: Gathering information about family relationships and social support networks is crucial in understanding an individual’s social context, which can significantly impact their therapy.
- Medical and Legal History: It also collects data on medical conditions and any legal issues. This holistic approach provides therapists with a better understanding of all factors that may affect an individual’s mental health.
Browse Other Templates
How Many Cows Do You Need to Be Tax Exempt in Texas - Keep a copy of the completed certificate with your purchase records.
Texas Kidney Healthcare Application - Timely submission of the form ensures prompt processing of claims.