Fill Out Your Braden Scale Form
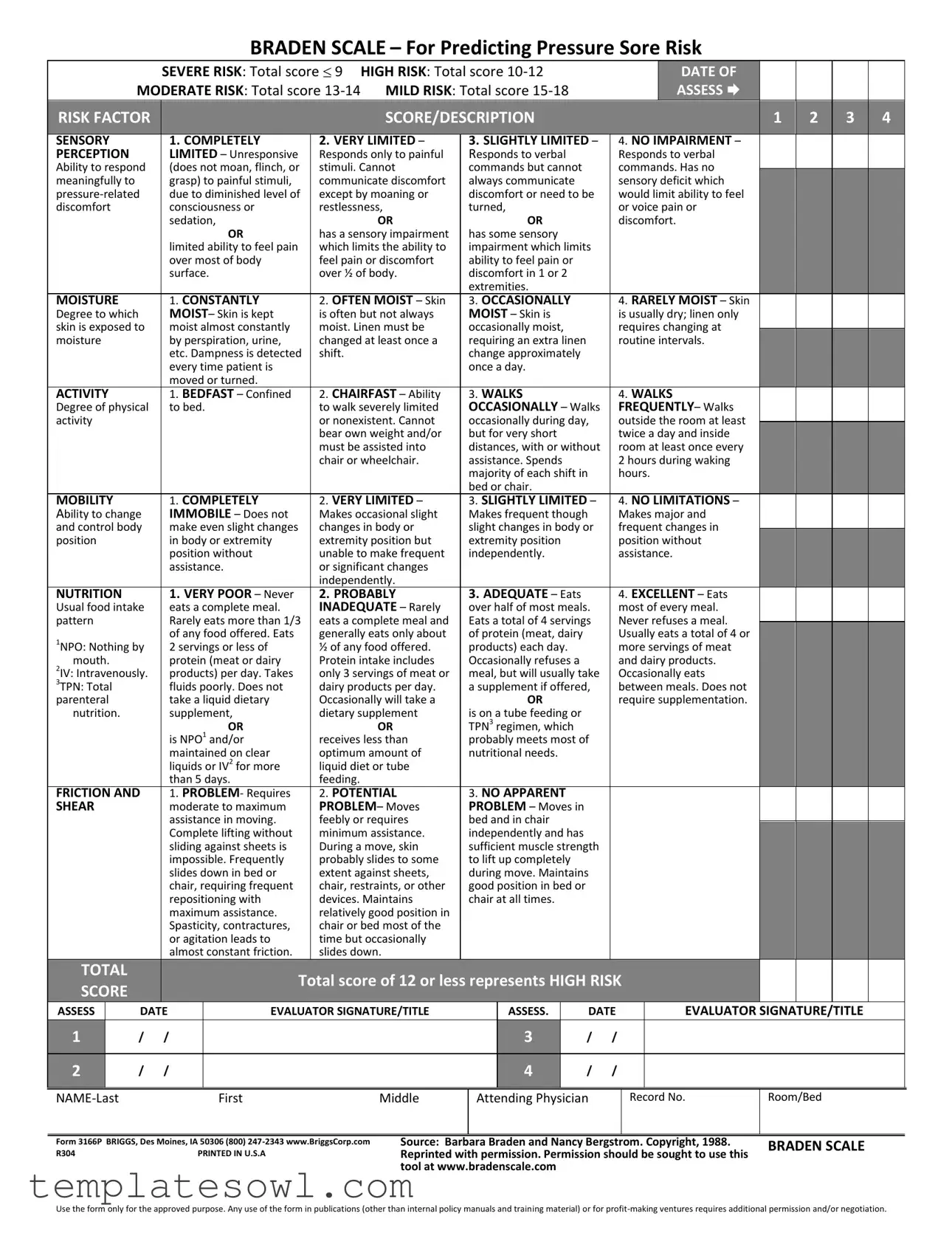
The Braden Scale is a crucial tool used in medical settings to predict the risk of pressure sores in patients. This form assigns scores to various risk factors, including sensory perception, moisture levels, activity, mobility, nutrition, and friction and shear. Each factor is assessed on a scale from one to four, with lower scores indicating greater risk. For instance, patients who are completely unresponsive or confined to bed receive high-risk scores. The total score determines the level of risk: severe risk is indicated by a score of nine or lower, while a score of ten to twelve indicates high risk, thirteen to fourteen suggests moderate risk, and scores of fifteen to eighteen represent mild risk. Proper evaluation requires careful consideration of each section, and the total score guides healthcare providers in formulating appropriate interventions to prevent pressure sore development. The form emphasizes a holistic view of the patient’s condition, integrating the interplay of physical health, nutritional status, and environmental factors.
Braden Scale Example
BRADEN SCALE – For Predicting Pressure Sore Risk
|
SEVERE RISK: Total score 9 |
HIGH RISK: Total score |
DATE OF |
|
MODERATE RISK: Total score |
MILD RISK: Total score |
ASSESS |
|
|
|
|
|
|
|
|
|
RISK FACTOR |
|
|
|
|
|
SCORE/DESCRIPTION |
|
|
|
|
|
|
|
1 |
2 |
3 |
4 |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SENSORY |
|
|
|
1. COMPLETELY |
2. VERY LIMITED – |
3. SLIGHTLY LIMITED – |
|
4. NO IMPAIRMENT – |
|
|
|
|||||||||||
|
|
PERCEPTION |
|
|
|
LIMITED – Unresponsive |
Responds only to painful |
Responds to verbal |
|
|
Responds to verbal |
|
|
|
||||||||||
|
|
Ability to respond |
|
|
(does not moan, flinch, or |
stimuli. Cannot |
commands but cannot |
|
|
commands. Has no |
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
meaningfully to |
|
|
|
grasp) to painful stimuli, |
communicate discomfort |
always communicate |
|
|
sensory deficit which |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
due to diminished level of |
except by moaning or |
discomfort or need to be |
|
would limit ability to feel |
|
|
|
|
||||||||||||
|
|
discomfort |
|
|
|
consciousness or |
restlessness, |
turned, |
|
|
or voice pain or |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
sedation, |
OR |
|
OR |
|
|
discomfort. |
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
OR |
has a sensory impairment |
has some sensory |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
limited ability to feel pain |
which limits the ability to |
impairment which limits |
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
over most of body |
feel pain or discomfort |
ability to feel pain or |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
surface. |
over ½ of body. |
discomfort in 1 or 2 |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
extremities. |
|
|
|
|
|
|
|
|
|
|
|
||
|
|
MOISTURE |
|
|
|
1. CONSTANTLY |
2. OFTEN MOIST – Skin |
3. OCCASIONALLY |
|
|
4. RARELY MOIST – Skin |
|
|
|
||||||||||
|
|
Degree to which |
|
|
|
MOIST– Skin is kept |
is often but not always |
MOIST – Skin is |
|
|
is usually dry; linen only |
|
|
|
||||||||||
|
|
skin is exposed to |
|
|
moist almost constantly |
moist. Linen must be |
occasionally moist, |
|
|
requires changing at |
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
moisture |
|
|
|
by perspiration, urine, |
changed at least once a |
requiring an extra linen |
|
|
routine intervals. |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
etc. Dampness is detected |
shift. |
change approximately |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
every time patient is |
|
once a day. |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
moved or turned. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
ACTIVITY |
|
|
|
1. BEDFAST – Confined |
2. CHAIRFAST – Ability |
3. WALKS |
|
|
4. WALKS |
|
|
|
||||||||||
|
|
Degree of physical |
|
|
to bed. |
to walk severely limited |
OCCASIONALLY – Walks |
|
FREQUENTLY– Walks |
|
|
|
||||||||||||
|
|
activity |
|
|
|
|
|
|
or nonexistent. Cannot |
occasionally during day, |
|
outside the room at least |
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
bear own weight and/or |
but for very short |
|
|
twice a day and inside |
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
must be assisted into |
distances, with or without |
|
room at least once every |
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
chair or wheelchair. |
assistance. Spends |
|
|
2 hours during waking |
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
majority of each shift in |
|
hours. |
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
bed or chair. |
|
|
|
|
|
|
|
|
|
|
|
||
|
|
MOBILITY |
|
|
|
1. COMPLETELY |
2. VERY LIMITED – |
3. SLIGHTLY LIMITED – |
|
4. NO LIMITATIONS – |
|
|
|
|||||||||||
|
|
Ability to change |
|
|
IMMOBILE – Does not |
Makes occasional slight |
Makes frequent though |
|
Makes major and |
|
|
|
||||||||||||
|
|
and control body |
|
|
make even slight changes |
changes in body or |
slight changes in body or |
|
frequent changes in |
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
position |
|
|
|
in body or extremity |
extremity position but |
extremity position |
|
|
position without |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
position without |
unable to make frequent |
independently. |
|
|
assistance. |
|
|
|
|
||||||||
|
|
|
|
|
|
|
assistance. |
or significant changes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
independently. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NUTRITION |
|
|
|
1. VERY POOR – Never |
2. PROBABLY |
3. ADEQUATE – Eats |
|
|
4. EXCELLENT – Eats |
|
|
|
||||||||||
|
|
Usual food intake |
|
|
eats a complete meal. |
INADEQUATE – Rarely |
over half of most meals. |
|
most of every meal. |
|
|
|
||||||||||||
|
|
pattern |
|
|
|
Rarely eats more than 1/3 |
eats a complete meal and |
Eats a total of 4 servings |
|
Never refuses a meal. |
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
1NPO: Nothing by |
|
|
of any food offered. Eats |
generally eats only about |
of protein (meat, dairy |
|
|
Usually eats a total of 4 or |
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
2 servings or less of |
½ of any food offered. |
products) each day. |
|
|
more servings of meat |
|
|
|
|
|||||||||||
|
|
mouth. |
|
|
|
protein (meat or dairy |
Protein intake includes |
Occasionally refuses a |
|
|
and dairy products. |
|
|
|
|
|||||||||
|
|
2IV: Intravenously. |
|
|
products) per day. Takes |
only 3 servings of meat or |
meal, but will usually take |
|
Occasionally eats |
|
|
|
|
|||||||||||
|
|
3TPN: Total |
|
|
|
fluids poorly. Does not |
dairy products per day. |
a supplement if offered, |
|
between meals. Does not |
|
|
|
|
||||||||||
|
|
parenteral |
|
|
|
take a liquid dietary |
Occasionally will take a |
|
OR |
|
|
require supplementation. |
|
|
|
|
||||||||
|
|
nutrition. |
|
|
|
supplement, |
dietary supplement |
is on a tube feeding or |
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
OR |
OR |
TPN3 regimen, which |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
is NPO1 and/or |
receives less than |
probably meets most of |
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
maintained on clear |
optimum amount of |
nutritional needs. |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
liquids or IV2 for more |
liquid diet or tube |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
than 5 days. |
feeding. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
FRICTION AND |
|
|
1. PROBLEM- Requires |
2. POTENTIAL |
3. NO APPARENT |
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
SHEAR |
|
|
|
moderate to maximum |
PROBLEM– Moves |
PROBLEM – Moves in |
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
assistance in moving. |
|
feebly or requires |
bed and in chair |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
Complete lifting without |
|
minimum assistance. |
independently and has |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
sliding against sheets is |
|
During a move, skin |
sufficient muscle strength |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
impossible. Frequently |
|
probably slides to some |
to lift up completely |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
slides down in bed or |
|
extent against sheets, |
during move. Maintains |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
chair, requiring frequent |
|
chair, restraints, or other |
good position in bed or |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
repositioning with |
|
devices. Maintains |
chair at all times. |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
maximum assistance. |
|
relatively good position in |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Spasticity, contractures, |
|
chair or bed most of the |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
or agitation leads to |
|
time but occasionally |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
almost constant friction. |
|
slides down. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TOTAL |
|
|
|
|
Total score of 12 or less represents HIGH RISK |
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
SCORE |
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
ASSESS |
|
DATE |
|
EVALUATOR SIGNATURE/TITLE |
|
ASSESS. |
|
DATE |
|
EVALUATOR SIGNATURE/TITLE |
|
|||||||||||
|
1 |
|
/ |
/ |
|
|
|
|
|
3 |
|
/ |
/ |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
2 |
|
/ |
/ |
|
|
|
|
|
4 |
|
/ |
/ |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
First |
Middle |
Attending Physician
Record No.
Room/Bed
Form 3166P BRIGGS, Des Moines, IA 50306 (800)
R304 |
PRINTED IN U.S.A |
Source: Barbara Braden and Nancy Bergstrom. Copyright, 1988. |
BRADEN SCALE |
Reprinted with permission. Permission should be sought to use this |
|
tool at www.bradenscale.com |
|
Use the form only for the approved purpose. Any use of the form in publications (other than internal policy manuals and training material) or for
Form Characteristics
| Fact Name | Description |
|---|---|
| Risk Categories | The Braden Scale categorizes risk into four levels: Severe Risk (Score of 9), High Risk (Scores of 10-12), Moderate Risk (Scores of 13-14), and Mild Risk (Scores of 15-18). |
| Components of Assessment | The scale assesses six key factors: Sensory Perception, Moisture, Activity, Mobility, Nutrition, and Friction & Shear. |
| Scoring System | Each risk factor is scored from 1 to 4, with lower scores indicating higher risk and higher scores indicating lower risk. |
| Final Score Interpretation | A total score of 12 or below identifies a patient as at high risk for pressure sores. |
| Governing Law Usability | State-specific regulations may require particular formats or guidelines when using the Braden Scale in healthcare settings. |
| Copyright Information | The Braden Scale is a copyrighted tool and requires permission for use beyond internal policies or training. |
| Usage Limitations | Any publication or commercial use of the Braden Scale may need additional permission or negotiation. Visit www.braden.com for details. |
| Evaluation Documentation | The form includes space to document assessment dates and evaluator signatures, ensuring accountability and traceability. |
Guidelines on Utilizing Braden Scale
Filling out the Braden Scale form is a crucial procedure to assess an individual's risk of pressure sores. After gathering the necessary information, one can proceed step-by-step to ensure accurate completion of the form.
- Gather Materials: Ensure you have a pen and the Braden Scale form readily available.
- Identify the Person Being Assessed: Write the name of the individual being assessed, including their last name, first name, and middle initial, in the designated space.
- Record the Date: Fill in the date on which the assessment is taking place.
- Evaluate Sensory Perception: Choose the appropriate score based on the individual's ability to perceive stimuli. Circle the corresponding number (1 to 4) based on the description that matches their condition.
- Assess Moisture: Determine the level of skin moisture exposure and circle the number that reflects this condition, again based on the descriptions provided.
- Evaluate Activity Level: Assess the individual's physical activity and select the corresponding score that best describes their activity level.
- Assess Mobility: Circle the number that represents the person's ability to change and control body position.
- Analyze Nutrition: Evaluate the individual's usual food intake pattern and circle the appropriate score based on how well they are meeting their nutritional needs.
- Evaluate Friction and Shear: Determine the risk related to friction and shear during movement. Circle the number that fits their condition.
- Calculate Total Score: Add the scores from all categories to reach a total score and determine the risk level.
- Record Additional Information: Fill in dates, evaluator's name, and title in the appropriate sections for documentation purposes.
Make sure to review the completed form for accuracy and sign it as the evaluator. Secure the document per your facility's policies, ensuring that the assessment aids in providing appropriate care and interventions.
What You Should Know About This Form
What is the Braden Scale form?
The Braden Scale form is a tool used by healthcare professionals to assess a patient's risk of developing pressure sores, also known as bedsores. It evaluates several risk factors, including sensory perception, moisture, activity, mobility, nutrition, and friction/shear. Each of these categories is scored, and the total score helps determine the patient's level of risk ranging from mild to severe.
How is the scoring system structured on the Braden Scale?
The Braden Scale assigns scores from 1 to 4 for each risk factor. A higher score indicates a lower risk of pressure sore development. The total score can range from 6 (indicating very high risk) to 23 (indicating no risk). The risk levels are categorized as follows: Severe risk (9 or below), High risk (10-12), Moderate risk (13-14), and Mild risk (15-18).
Why is it important to use the Braden Scale?
Using the Braden Scale is essential for early identification of patients at risk for pressure sores. Early detection allows healthcare providers to implement preventative measures, such as repositioning, proper skin care, and nutritional support, thereby reducing the occurrence of pressure sores and improving patient outcomes.
How often should the Braden Scale be completed?
The Braden Scale should be completed upon patient admission and at regular intervals thereafter. It can be beneficial to reassess the patient regularly, especially if there are changes in their health status, mobility, or other relevant factors that could affect their risk level.
Who can complete the Braden Scale assessment?
Any trained healthcare professional, such as nurses or nursing assistants, can complete the Braden Scale assessment. It is crucial that the person conducting the assessment has an understanding of the scoring system and the risk factors involved in predicting pressure sore risk.
What should be done if a patient scores high on the Braden Scale?
If a patient is evaluated and scores high on the Braden Scale, healthcare providers should implement appropriate interventions. These may include more frequent repositioning, specialized skincare routines, ensuring adequate nutrition, and possibly using pressure-relieving devices to protect vulnerable areas of the skin.
Can the Braden Scale be used in various healthcare settings?
Yes, the Braden Scale is versatile and can be used across different healthcare settings, including hospitals, nursing homes, and home healthcare situations. It is beneficial in any environment where patients may be at risk for pressure sores due to limited mobility or other health complications.
Is there any specific training required to use the Braden Scale?
While formal certification is not mandatory, proper training on using the Braden Scale is recommended. This training ensures that healthcare providers understand how to assess patients accurately, interpret scores correctly, and implement preventative strategies effectively.
What resources are available for more information about the Braden Scale?
For more information about the Braden Scale, resources are available on websites such as www.bradenScale.com. Additionally, healthcare facilities may provide internal training materials and guidelines that focus on using the Braden Scale effectively.
Are there any limitations to the Braden Scale?
Although the Braden Scale is useful, it does have limitations. It may not account for all individual factors that contribute to pressure sore risk. Factors such as comorbidities, skin conditions, and patient hygiene practices are important to consider alongside the scale results for a comprehensive assessment.
Common mistakes
When it comes to evaluating patients for pressure sore risk using the Braden Scale, accuracy is vital. However, many make common mistakes that can impact the assessment's effectiveness. Here are eight errors often seen when filling out the Braden Scale form.
First, many individuals do not take the time to understand the scoring system properly. Each risk factor has specific criteria that must be assessed thoroughly. A rush to judgment can lead to misinterpretation, resulting in an inaccurate score. When scoring sensory perception, for instance, it’s crucial to observe how responsive the patient is to stimuli, not just to assume based on a previous diagnosis.
Another common mistake is neglecting to consider the patient’s full clinical picture. Patients may have fluctuating conditions, and a one-time assessment may not capture the ongoing risks. Scores should be updated regularly, especially if there’s a change in the patient's mobility or dietary intake.
Some assessors overlook the importance of moisture in determining skin health. Skin that is "occasionally moist" may not seem alarming at first glance. However, understanding the implications of continual moisture exposure is critical. It can lead to softening of the epidermis, increasing the risk for pressure sores.
In addition, miscommunication between team members can lead to errors on the form. Nurses or caregivers may fill out the form based on what they believe the last assessment indicated, rather than writing down current observations. Continuous communication ensures consistency in care and records.
Another mistake often made is underestimating the mobility and physical activity scores of patients. Patients labeled as “chairfast” may still have the ability to engage in limited activity, which could lead to them being assessed inaccurately. Evaluators must pay close attention to the actual capabilities of the patient rather than relying solely on observed behaviors during the assessment.
Nutrition is another area where missteps happen. Many may fill out this section based on the patient’s overall eating habits rather than their specific intake during the assessment period. If a patient has recently changed medications or experienced side effects, these might affect their appetite and nutritional consumption. Each meal should be evaluated individually to provide a true picture of the patient’s nutritional status.
Moreover, assessors sometimes fail to account for external factors that may contribute to friction and shear. Patients with specific conditions, like spasticity or advanced age, may have a higher risk but are not always scored accordingly. Understanding each patient's unique situation helps to provide a clearer risk assessment.
Lastly, errors can arise when evaluators do not document their findings consistently. Clear documentation is essential not only for the current care team but also for future assessments. Each scorer must keep meticulous notes on the assessment date, evaluators, and observations to ensure every risk is adequately captured.
By being aware of these common pitfalls, you can help ensure that the Braden Scale assessment accurately reflects the patient’s risk for pressure sores. An accurate score is essential in providing the right preventative measures and care, ultimately leading to better patient outcomes.
Documents used along the form
The Braden Scale form is a valuable tool used to assess the risk of pressure sores in patients. However, it is often used alongside other important documents that help healthcare professionals ensure comprehensive patient care. Here’s a list of commonly associated forms and documents:
- Patient Assessment Form: This form gathers general information about the patient's health status, medications, and prior medical history, allowing clinicians to customize care plans.
- Nursing Care Plan: A structured outline of the nursing interventions required for a patient, this plan addresses specific needs identified during assessments, including those from the Braden Scale.
- Skin Assessment Form: This document details the condition of a patient's skin, documenting any existing wounds or areas of concern that may contribute to a pressure sore risk evaluation.
- Incident Report Form: If a patient experiences a pressure sore incident, this form is used to document the event for quality control. It helps facilities track and improve care protocols.
- Patient Monitoring Log: A log that tracks ongoing assessments of the patient’s condition, including mobility and nutrition. Regular entries facilitate timely interventions.
- Dietary Assessment Form: This form collects information about the patient's diet and nutritional needs. Proper nutrition plays a significant role in skin health and pressure sore prevention.
- Consultation Report: If specialized care is needed, this form provides recommendations from consulting specialists, ensuring that all aspects of the patient's health are addressed.
- Discharge Plan: A plan developed before the patient leaves a healthcare facility, it outlines follow-up care, necessary equipment, and education on preventing future pressure sores.
Using these forms in conjunction with the Braden Scale ensures a holistic approach to patient care. They serve to strengthen communication among healthcare team members and enhance patient outcomes.
Similar forms
The Braden Scale is widely used to assess pressure sore risk, but several other documents serve similar purposes in various healthcare settings. Each of these documents evaluates different aspects of patient care and risk factors associated with specific conditions. Here are eight documents that bear similarity to the Braden Scale:
- Norton Scale: Similar to the Braden Scale, the Norton Scale assesses a patient's risk for pressure ulcer development using factors like physical condition, mental state, activity, mobility, and incontinence. This scale also employs a scoring system, where lower scores indicate higher risk.
- Morse Fall Scale: The Morse Fall Scale focuses on identifying a patient's risk for falls. It considers the history of falls, secondary diagnoses, ambulatory aid, and more, paralleling the Braden Scale's method of assessing different risk factors through a scoring system.
- Waterlow Score: Like the Braden Scale, the Waterlow Score assesses pressure sore risk. It evaluates factors such as body mass index, skin type, gender, and medical history. The use of a calculated score aids healthcare professionals in identifying patients at risk.
- Ramsay Sedation Scale: The Ramsay Sedation Scale measures a patient's level of sedation and awareness, similar to how the Braden Scale assesses sensory perception. This tool helps track patients who may be less responsive due to sedation or other medical conditions.
- Bishop Scale: The Bishop Scale evaluates the readiness for labor in pregnant patients. It uses scoring for aspects like cervical dilation and effacement, offering a structured approach akin to the Braden Scale's risk assessment framework.
- Glasgow Coma Scale: The Glasgow Coma Scale assesses a patient's level of consciousness following a head injury. It evaluates eye opening, verbal response, and motor response, similar to how the Braden Scale addresses sensory perception.
- Skin Assessment Tool: This tool encourages regular evaluation of the skin condition in patients. It measures the appearance and integrity of skin and underlying tissues, akin to the risk factors assessed in the Braden Scale.
- CHA2DS2-VASc Score: The CHA2DS2-VASc Score identifies patients at risk of thromboembolism, utilizing criteria such as congestive heart failure, hypertension, age, diabetes, and stroke history. Its structured assessment shares similarities with the methodical approach of the Braden Scale.
These documents, while tailored to different aspects of patient care, reflect the shared principle of systematic evaluation to improve patient outcomes. By employing such tools, healthcare providers can enhance their ability to identify risks and apply appropriate interventions.
Dos and Don'ts
When filling out the Braden Scale form, it is important to adhere to best practices to ensure accuracy and effectiveness. The following list outlines key dos and don’ts.
- Do read the instructions carefully to understand the scoring system.
- Do assess each category thoroughly based on observation and clinical judgment.
- Do involve other healthcare team members when needed for a comprehensive evaluation.
- Do complete the form promptly after patient assessment to ensure the information is current.
- Don't rush through the assessment; take the time to evaluate each risk factor properly.
- Don't make assumptions without evidence when determining the patient's risk level.
- Don't use outdated information from previous assessments; prioritize the most recent observations.
Misconceptions
Understanding the Braden Scale is crucial for predicting the risk of pressure sores. Misconceptions can lead to inadequate care. Here are six common misconceptions about the Braden Scale:
- The Braden Scale is only for the elderly population. This scale can be utilized for patients of all ages. Pressure sore risk can occur in anyone with limited mobility, regardless of age.
- A high score on the Braden Scale indicates no risk at all. A high score suggests lower risk, but it does not eliminate the possibility of pressure sores. Continuous monitoring is essential.
- Assessing moisture is the only factor that matters. Moisture is one of several factors assessed. Sensory perception, activity, mobility, nutrition, and friction/shear are also critical in determining risk.
- Once assessed, patients do not need to be re-evaluated. Regular re-assessments are vital. A patient's condition may change over time, requiring adjustments in care strategies.
- The Braden Scale is a diagnostic tool. The scale assesses risk, not a diagnosis. The findings should inspire preventive measures rather than serve as a definitive medical conclusion.
- The Braden Scale is used only in hospital settings. While it is widely used in hospitals, the scale is also beneficial in long-term care facilities, home health settings, and rehabilitation centers.
Accurate understanding and application of the Braden Scale can enhance patient care and prevent adverse outcomes. Education and awareness among healthcare providers can mitigate these misconceptions.
Key takeaways
Using the Braden Scale form is essential for assessing a person's risk of developing pressure sores. Here are some key takeaways to keep in mind:
- Understanding Risk Levels: The Braden Scale categorizes risk into four levels: severe risk (total score 9), high risk (score 10-12), moderate risk (score 13-14), and mild risk (score 15-18). Identifying the correct level helps guide care decisions.
- Detailed Scoring System: Each of the six components—sensory perception, moisture, activity, mobility, nutrition, and friction/shear—has a scoring system. This comprehensive evaluation is key to understanding overall risk.
- Regular Assessments: It is important to complete the Braden Scale assessment regularly. Changes in a patient's condition can affect their risk level, so consistent evaluations ensure timely interventions.
- Interdisciplinary Use: This tool should be utilized by various healthcare professionals. Nurses, physicians, and dietitians can all contribute valuable insights, enhancing the accuracy of the assessment.
- Documenting Scores: Always record the scores, the date of assessment, and the evaluator's details. This information is vital for tracking changes over time and for ensuring communication among care team members.
By following these takeaways, individuals involved in patient care can assess and manage pressure sore risks more effectively.
Browse Other Templates
Duplicate Diploma Request Form,NMSU Degree Verification Form,NMSU Transcript Reissue Form,NMSU Diploma Replacement Form,NMSU Graduation Document Request,NMSU Academic Certificate Request,NMSU Credential Retrieval Form,NMSU Degree Copy Order Form,NMSU - Ensure to check the total cost when ordering multiple copies.
Dmv Accident Report Form - Timeliness in submitting the SR1 is essential to avoid receiving penalties from the DMV.