Fill Out Your C 4 3 Form
When navigating the complexities of workers' compensation, understanding the C 4 3 form is essential for both medical professionals and injured workers. This form, known as the Doctor's Report C-4.3 of Maximum Medical Improvement (MMI) and Permanent Partial Impairment, serves as a crucial tool in the assessment process. It is typically used when a doctor needs to provide their opinion on whether a patient has reached MMI or to evaluate any permanent partial impairments resulting from a work-related injury. Being thorough in completing the form is key, as it not only facilitates timely payments for necessary treatments but also ensures proper compensation for lost wages. The C 4 3 form requires detailed patient information, including their injury history and treatment details. In addition, it compels the doctor to assess the patient’s current medical status, particularly whether they have reached maximum recovery and if there is any lasting impairment. Proper submission of this form to the Workers' Compensation Board, the insurance carrier, and potentially the patient's legal representative is vital. Inaccuracies or delays can lead to unnecessary complications, such as delays in treatment, wage loss benefits, and even the need for testimony. For physicians looking to expedite the process, an online version of the form is available at the Workers' Compensation Board's website, enhancing accessibility and convenience.
C 4 3 Example

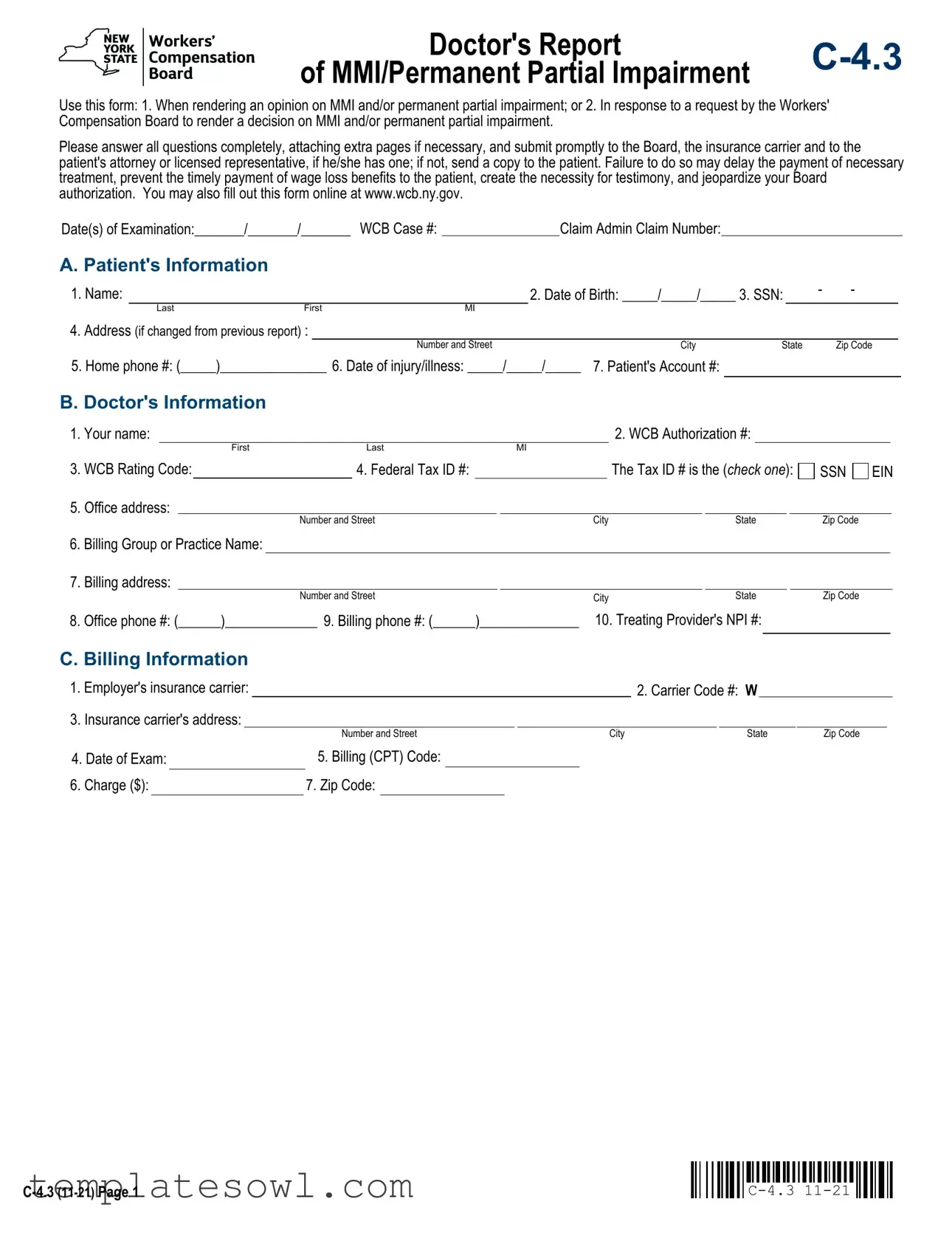
Doctor's Report |
|
of MMI/Permanent Partial Impairment |
Use this form: 1. When rendering an opinion on MMI and/or permanent partial impairment; or 2. In response to a request by the Workers' Compensation Board to render a decision on MMI and/or permanent partial impairment.
Please answer all questions completely, attaching extra pages if necessary, and submit promptly to the Board, the insurance carrier and to the patient's attorney or licensed representative, if he/she has one; if not, send a copy to the patient. Failure to do so may delay the payment of necessary treatment, prevent the timely payment of wage loss benefits to the patient, create the necessity for testimony, and jeopardize your Board authorization. You may also fill out this form online at www.wcb.ny.gov.
Date(s) of Examination:_______/_______/_______ WCB Case #:Claim Admin Claim Number:
A. Patient's Information
1. Name: |
|
|
|
2. Date of Birth: _____/_____/_____ 3. SSN: |
- |
- |
|
||||
|
Last |
First |
MI |
|
|
|
|
|
|
|
|
4. Address (if changed from previous report) : |
|
|
|
|
|
|
|
|
|||
|
|
|
|
Number and Street |
City |
State |
|
Zip Code |
|
||
5. Home phone #: (_____)_______________ 6. Date of injury/illness: _____/_____/_____ |
7. Patient's Account #: |
|
|
|
|
|
|||||
B. Doctor's Information
1. Your name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
2. WCB Authorization #: |
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
First |
|
|
Last |
|
|
|
MI |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
3. |
WCB Rating Code: |
|
|
|
4. Federal Tax ID #: |
|
|
|
|
|
|
|
|
The Tax ID # is the (check one): |
SSN |
EIN |
||||||||||||||||||||||||
5. |
Office address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
Number and Street |
|
|
|
|
|
City |
|
|
|
|
|
State |
|
|
|
|
|
Zip Code |
|
|
|
||||||||||
6. |
Billing Group or Practice Name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
7. |
Billing address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
Number and Street |
|
|
|
|
|
City |
|
|
|
|
|
State |
|
|
|
Zip Code |
|
|
|
||||||||||||
8. |
Office phone #: (______)_____________ 9. Billing phone #: (______)______________ |
10. Treating Provider's NPI #: |
|
|
|
|
||||||||||||||||||||||||||||||||||
C. Billing Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
1. |
Employer's insurance carrier: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. Carrier Code #: W |
|
|
|
|
|
||||||||||||||||||
3. |
Insurance carrier's address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
Number and Street |
|
|
|
|
|
|
|
City |
|
|
|
|
|
State |
|
Zip Code |
|
|
|
|||||||||||
4. Date of Exam: |
|
5. Billing (CPT) Code: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
6. |
Charge ($): |
|
|
7. Zip Code: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
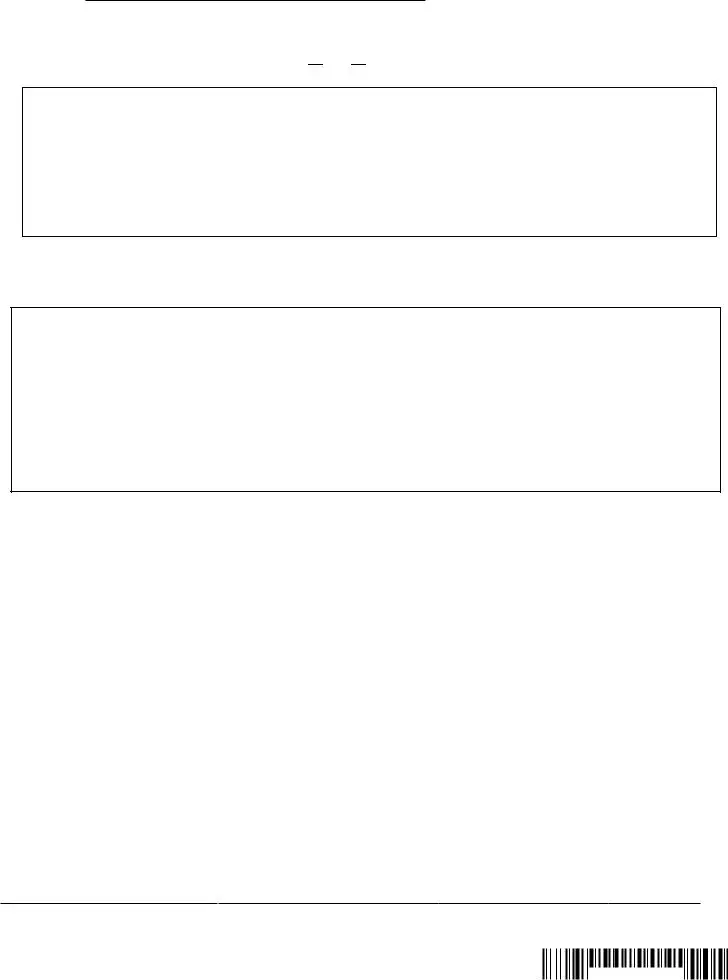
Patient's Name:
Last |
First |
MI |
Date of injury/onset of illness:______/______/______
D. Maximum Medical Improvement
1. Has the patient reached Maximum Medical Improvement?  Yes
Yes  No If yes, provide the date patient reached MMI: _____/_____/_____
No If yes, provide the date patient reached MMI: _____/_____/_____
If No, describe why the patient has not reached MMI and the proposed treatment plan (attach additional documentation, if necessary).
E. Permanent Partial Impairment
1.Is there permanent partial impairment?  Yes
Yes  No
No
2.List the body parts and conditions you treated the patient for related to the date of injury listed in Section A, Question 6.
Complete Permanent Partial Disability, Attachment A and/or Attachment B, as indicated based on the patient's condition. Attachment A and/or Attachment B must be completed for each body part and/or condition which you treated the patient for on the date of injury listed in Section A, Question 6.
nFor a permanent partial impairment where schedule award (schedule loss of use) is appropriate, complete Attachment A, except for serious facial disfigurement, vision, or hearing loss.
Hearing Loss:
lOccupational Loss of Hearing -
lTraumatic Hearing Loss - C4.3 with an attached narrative.
Vision Loss:
lAttending Ophthalmologist's Report (Form
l
Serious Facial Disfigurement
l
nFor a
Sign below and submit to the Board only the pages of the form that apply to this report.
This form is signed under penalty of perjury.
Board Authorized Health Care Provider signature:
|
|
/ |
/ |
Name |
Signature |
Specialty |
Date |
|
|||

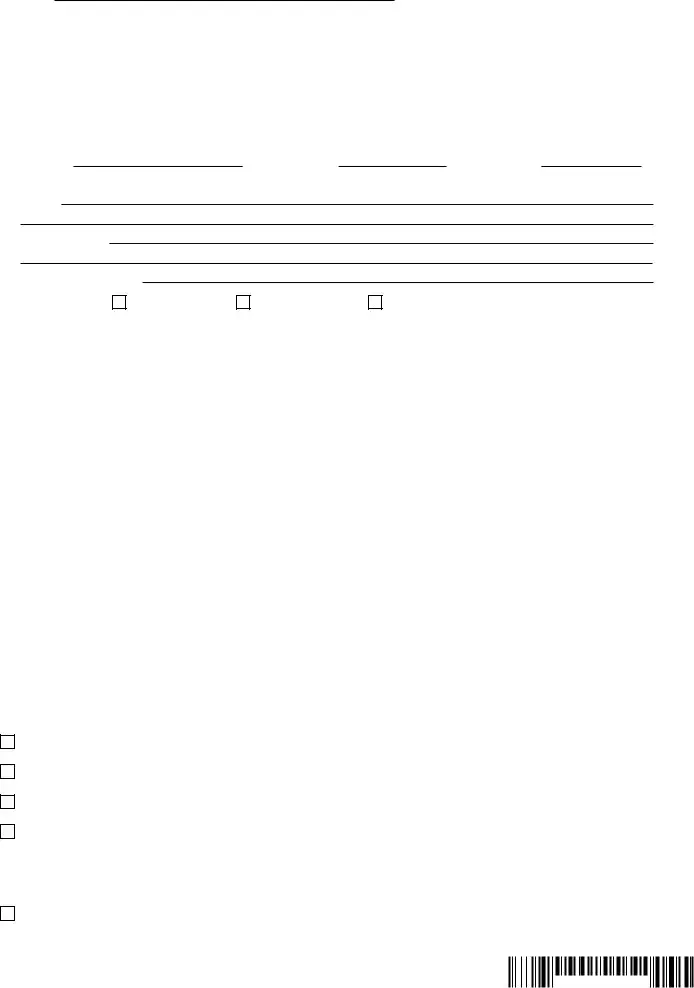
Patient's Name: |
|
|
|
Date of injury/onset of illness:______/______/______ |
|
Last |
First |
MI |
|
Permanent Partial Disability - Attachment A
Schedule Loss of Use of Member
If the patient has a permanent partial impairment, complete Attachment A for all body parts and conditions for which a schedule award is appropriate (schedule loss of use). You must complete this attachment for all body parts and conditions for which you treated the patient for the date of injury listed in Section A, Question 6. Attach additional sheets if needed.
Body Part
Please include all the information in the bullet points below in the table on this page or attach a medical narrative with your report. The medical narrative should include the following information:
lAffected body part (include left or right side) and identify Guideline chapter (when special consideration exist).
lMeasured Active Range of Motion (ROM) (3 measurements for injured body part, and use the greatest ROM). If not, please explain why.
lMeasurement of contralateral body part ROM, or explain why inapplicable
lPreviously received scheduled losses of use to same body part(s), if known
lSpecial considerations
lLoading for Digits and Toes
 C-4.3
C-4.3
|
|
|
Body Part/Measurement |
|
Body Part/Measurement |
|
Body Part/Measurement |
|
Body Part/Measurement |
|
Body Part/Measurement |
|
Body Part/Measurement |
||||||
|
1 |
|
|
2 |
|
|
3 |
|
|
4 |
|
|
5 |
|
|
6 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Left |
Right |
|
Left |
Right |
|
Left |
Right |
|
Left |
Right |
|
Left |
Right |
|
Left |
Right |
Range of Motion |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(3 measures) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Contralateral |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Applicable Y/N |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
If No, please |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
explain below |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Contralateral ROM |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Special Considerations |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(Chapter) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Impairment % |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Details: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
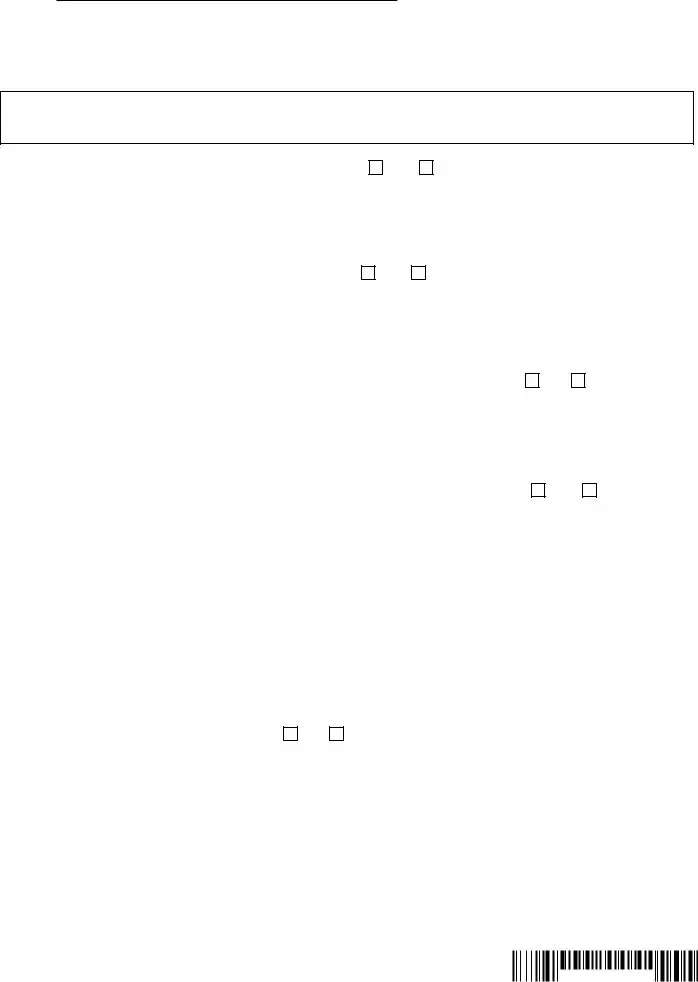
Patient's Name:
Last |
First |
MI |
Date of injury/onset of illness:______/______/______
Permanent Partial Disability - Attachment B
1.
(Identify impairment class according to the latest Workers' Compensation Guidelines for Determining Impairment. Attach separate sheet for |
||||||
additional body parts.) |
|
|
|
|
|
|
Body Part: |
|
Impairment Table: |
|
Severity Ranking: |
|
|
Body Part: |
|
Impairment Table: |
|
Severity Ranking: |
|
|
Body Part: |
Impairment Table: |
|
Severity Ranking: |
|||
State the basis for the impairment classification (attach additional narrative, if necessary):
History:
Physical Findings:
Diagnostic Test Results:
2. Patient's Work Status: |
At the |
At other employment |
Not working |
3.Functional Capabilities/Exertion Abilities:
a. Please describe patient's residual functional capacities for any work at this time (not limited to the
|
Never |
Occasionally |
Frequently |
Constantly |
|
|
|
|||||||||||
Lifting/carrying |
|
|
|
|
|
|
lbs. |
|
|
|
lbs. |
|
|
|
lbs. |
|
||
|
|
|
|
|
|
|
|
|
||||||||||
Pulling/pushing |
|
|
|
|
|
|
lbs. |
|
|
|
lbs. |
|
|
|
lbs. |
|
||
|
|
|
|
|
|
|
|
|
||||||||||
Sitting |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Patient's Residual Functional Capacities |
|
||
Standing |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
n Occasionally: can perform activity up to |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1/3 of the time. |
|
||
Walking |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
n Frequently: can perform activity from |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
Climbing |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1/3 to 2/3 of the time. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
Kneeling |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
n Constantly: can perform activity more |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
than 2/3 of the time. |
|
||
Bending/stooping/squatting |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
Simple grasping |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Fine manipulation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Reaching overhead |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Reaching at/or below shoulder level |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Driving a vehicle |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Operating machinery |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Temp extremes/high humidity |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Environmental |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
Specify: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
b. Please check the applicable category for the patient's exertional ability: |
|
|
|
|
|
|
|
|||||||||||
Very Heavy Work - Exerting in excess of 100 pounds of force occasionally, and/or in excess of 50 pounds of force frequently, and/or in excess of 20 pounds of force constantly to move objects. Physical demand requirements are in excess of those for Heavy Work.
Heavy Work - Exerting 50 to 100 pounds of force occasionally, and/or 25 to 50 pounds of force frequently, and/or 10 to 20 pounds of force constantly to move objects. Physical demand requirements are in excess of those for Medium Work.
Medium Work - Exerting 20 to 50 pounds of force occasionally, and/or 10 to 25 pounds of force frequently, and/or greater than negligible up to 10 pounds of force constantly to move objects. Physical demand requirements are in excess of those for Light Work.
Light Work - Exerting up to 20 pounds of force occasionally, and/or up to 10 pounds of force frequently and/or negligible amount of force constantly to move objects. Physical demand requirements are in excess of those for Sedentary Work. Even though the weight lifted may only be a negligible amount, a job should be rated Light Work: (1) when it requires walking or standing to a significant degree; or (2) when it requires sitting most of the time but entails pushing and/or pulling of arm or leg controls; and/or (3) when the job requires working at a production rate pace entailing the constant pushing and/or pulling of materials even though the weight of those materials is negligible. NOTE: The constant stress of maintaining a production rate pace, especially in an industrial setting, can be and is physically demanding of a worker even though the amount of force exerted is negligible.
Sedentary Work - Exerting up to 10 pounds of force occasionally and/or a negligible amount of force frequently to lift, carry, push, pull or otherwise move objects, including the human body. Sedentary work involves sitting most of the time, but may involve walking or standing for brief periods of time. Jobs are sedentary if walking and standing are required only occasionally and all other sedentary criteria are met.
Patient's Name:
Last |
First |
MI |
Date of injury/onset of illness:______/______/______
Functional Capabilities/Exertion Abilities (continued):
c. Other medical considerations which arise from this work related injury (including the use of pain medication such as narcotics):
d. Could this patient perform his/her |
Yes |
No |
|
|
|
|
If Yes, specify: |
|
|
|
|
|
|
|
|
|
|
e. Could this patient perform any work activities with or without restrictions? |
Yes |
No |
|
|
|
|
Explain: |
|
|
|
|
|
|
|
|
|
|
f. If patient is not working, could reasonable accommodations be made to enable the patient to perform work? |
Yes |
No |
|||
|
If Yes, explain: |
|
|
|
|
|
|
|
|
|
|
4. Has the patient had an injury/illness since the date of injury which impacts residual functional capacity? |
Yes |
No |
|||
|
If Yes, explain. Attach additional sheets if necessary. |
|
|
|
|
|
|
|
|
|
|
5. Would the patient benefit from vocational rehabilitation? |
Yes |
No |
|
|
If Yes, explain |
|
|
|
|
|
|
IMPORTANT - TO THE ATTENDING DOCTOR
The
MEDICAL REPORTING
This form must be signed by the attending doctor and must contain his/her authorization certificate number, code letters and NPI number.
A CHIROPRACTOR, PODIATRIST, PSYCHOLOGIST, NURSE PRACTITIONER OR LICENSED CLINICAL SOCIAL WORKER FILING THIS REPORT CERTIFIES THAT THE INJURY DESCRIBED CONSISTS SOLELY OF A CONDITION(S) WHICH MAY LAWFULLY BE TREATED BY THE FILING PROVIDER, AS DEFINED IN THE EDUCATION LAW AND, WHERE IT DOES NOT, THE FILING PROVIDER HAS ADVISED THE INJURED PERSON TO CONSULT A PHYSICIAN OF HIS/HER CHOICE.
HIPAA NOTICE - In order to adjudicate a workers' compensation claim,
Ask the patient if he/she has retained a legal representative. If they have retained legal representation, you are required to send copies of all reports to the patient's representative.
Instructions for Completing Section D, E, Attachment A and Attachment B
Section D. Maximum Medical Improvement
Section D includes questions regarding maximum medical improvement (MMI). For the definition of MMI, see Chapter 1.2 of the 2018 Guidelines and 2012 Guidelines. A provider who finds that the patient has met MMI should so indicate and provide the approximate date of such finding (Question 1). If the patient has not yet reached MMI so indicate (Question 1) and provide an explanation as to why additional improvement is expected and the proposed treatment plan.
Section E. Permanent Partial Impairment
Section E includes questions regarding permanent partial impairment. If there is no permanent partial impairment (Question 1) do not file this form, instead use Form
List all the body parts and/or conditions that the patient was treated for with regards to the workers' compensation claims identified in Section A of the form (Question 2). Complete either Attachment A and/or Attachment B for each body part and/or condition for which permanency exists.
Permanent Partial Disability
Attachment A and Attachment B includes questions about schedule loss of use of member or facial disfigurement (1) or
Attachment A. Schedule loss of use of member
Determine impairment % using the 2018 Workers' Compensation Guidelines for Determining Impairment. If a scheduled loss is appropriate under the 2018 Impairment Guidelines do not complete any questions in Attachment B. Attach additional sheets or narrative, if necessary. The provider should sign the Board Authorization at the bottom of page 2 and return to the Workers' Compensation Board.
Attachment B.
If the patient was treated for a body part and condition that is not amendable to a schedule loss of use award, record the body part, impairment table and severity letter grade for each body part or system (Question 1) using the 2012 Guidelines. Also state the history, physical findings, and diagnostic test results that support the impairment finding. If the patient has a
Complete the questions regarding the patient's work status (2).
Complete the Functional Capabilities/Exertion Abilities (Question 3. a - f). Attachment B should be completed based on the patient's current condition if the provider believes there is MMI and/or permanent partial impairment or in a response to a request by the Board to render a decision on MMI and/or permanent partial impairment.
Question 3. includes questions applicable to a patient who has reached MMI and has a permanent,
Question 3a - Rate whether the patient can perform each of the fifteen functional abilities: never, occasionally, frequently, or constantly. Note the specific weight tolerances for the categories lifting/carrying and pulling/pushing. There is also room to describe any functional limitations in connection with environmental conditions (e.g., occupational asthma). Attach documentation when describing
Question 3b - Check the applicable category for the patient's exertional ability.
Question 3c - Note any other medical considerations arising from the permanent injury that are not captured elsewhere in Attachment B. This includes any restrictions or limitations that may be imposed as a result of medications (e.g., narcotics) taken by the patient or other relevant medical considerations that impact work function.
Question 3d - With knowledge of the patient's
Question 3e. Indicate whether the patient can perform any work activities with or without restrictions. Explain by providing what activities can be performed with restrictions and what work activities can be performed without restrictions.
Question 3f - Provide an explanation whether reasonable accommodations can be made for the patient.
Question 4 - Explain or attach a detailed explanation if the patient has had an intervening injury or illness that may account for any of the functional restrictions noted in Question 3a.
Question 5 - Indicate if the patient would benefit from vocational rehabilitation and if so, provide detailed explanation.

BILLING INFORMATION
Complete all billing information contained on this form. Use additional forms or narrative, if necessary. The workers' compensation carrier has 45 days to pay the bill or to file an objection to it. Contact the workers' compensation carrier if neither payment nor an objection are received within this time period. After contacting the carrier, if necessary, file Health Provider's Request for Decision on Unpaid Medical Bill(s) (Form
ANY PERSON WHO KNOWINGLY AND WITH INTENT TO DEFRAUD PRESENTS, CAUSES TO BE PRESENTED, OR PREPARES WITH KNOWLEDGE OR BELIEF THAT IT WILL BE PRESENTED TO OR BY AN INSURER, OR
All reports are to be filed by sending directly to the Workers' Compensation Board at the address below with a copy sent to the insurance carrier:
NYS Workers' Compensation Board - Centralized Mailing, PO Box 5205, Binghamton, NY
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose of Use | This form is used to provide an opinion on Maximum Medical Improvement (MMI) and/or permanent partial impairment for workers' compensation cases. |
| Response to Board | The form may also be submitted in response to a request from the Workers' Compensation Board regarding MMI or permanent partial impairment evaluations. |
| Submission Requirements | All questions on the form must be answered completely. Extra pages may be attached if necessary. Timely submission is critical to avoid treatment payment delays. |
| Patient Information | The form collects essential patient details including name, date of birth, Social Security Number, and the date of injury or illness. |
| Doctor's Information | Doctors must provide their name, WCB authorization number, and tax ID among other details, ensuring proper identification and billing. |
| Maximum Medical Improvement Assessment | The form requires a determination of whether the patient has reached MMI and provides space for explanations if not. |
| State Governing Laws | This form is governed by the New York Workers' Compensation Law, pertaining to the evaluation of work-related injuries. |
Guidelines on Utilizing C 4 3
Completing the C 4 3 form is essential when assessing a patient's Maximum Medical Improvement (MMI) and any permanent partial impairments. This process ensures accurate communication with the Workers' Compensation Board and facilitates timely treatment and benefits for the patient.
- Gather necessary information, including patient and doctor details, insurance information, and specific injury details.
- Fill in the date(s) of examination.
- Provide the WCB Case number and Claim Admin Claim Number.
- In section A, enter the patient's name, date of birth, SSN, address, home phone number, date of injury/illness, and patient account number.
- In section B, enter your name, WCB Authorization number, WCB Rating Code, Federal Tax ID number (specifying if it's an SSN or EIN), and office address. Also, include the billing group or practice name and addresses and both office and billing phone numbers. Finally, provide the treating provider's NPI number.
- In section C, input the employer’s insurance carrier, the carrier code number, the insurance carrier's address, date of exam, CPT code for billing, charge amount, and zip code.
- In section D, indicate whether the patient has reached MMI, and if yes, provide the date. If no, explain why they have not reached MMI and detail the proposed treatment plan.
- Section E asks if there is permanent partial impairment. Indicate 'Yes' or 'No.' If 'Yes,' list the body parts and conditions related to the injury from section A, question 6.
- Complete either Attachment A or Attachment B for permanent partial disability, depending on the applicable situation. Attach supporting documentation if necessary.
- Sign the form under penalty of perjury, including your name, signature, specialty, and the date.
- Submit the completed form promptly to the Board, insurance carrier, and patient's attorney or licensed representative. If the patient does not have an attorney or representative, send a copy directly to them.
What You Should Know About This Form
What is the purpose of the C 4 3 form?
The C 4 3 form is used to provide a doctor's opinion on whether a patient has reached Maximum Medical Improvement (MMI) and to assess any permanent partial impairment related to a work injury or illness. This form is required when requested by the Workers' Compensation Board or when a healthcare provider deems it necessary based on the patient's condition.
Who is responsible for submitting the C 4 3 form?
The healthcare provider who completes the form is responsible for submitting it. The completed form must be sent promptly to the Workers' Compensation Board, the patient's insurance carrier, and the patient's attorney or licensed representative, if applicable. If there is no attorney, a copy should be sent to the patient directly.
What happens if the C 4 3 form is not submitted on time?
If the C 4 3 form is not submitted promptly, it may lead to delays in the payment for necessary medical treatments and can hinder the timely provision of wage loss benefits to the patient. Such delays could also create the need for testimony and jeopardize the healthcare provider's authorization by the Board.
Can the C 4 3 form be filled out online?
Yes, the C 4 3 form can be filled out online. It is available on the website www.wcb.ny.gov. Utilizing the online version can streamline the process and reduce potential errors associated with handwritten submissions.
What should be included in the patient's medical narrative attached to the form?
The patient's medical narrative should encompass several key details, including the affected body part, the range of motion (with three measurements), previous scheduled losses to the same body part, and any special considerations. This comprehensive information is crucial for accurately assessing the level of impairment and ensuring proper classification for potential awards.
Common mistakes
Completing the C 4 3 form can be straightforward, but there are common mistakes that can cause delays or complications. One significant error is not providing complete information. Each section of the form is crucial. If a name, date, or account number is missing, it could slow down the process significantly. It’s essential to ensure all fields are filled out accurately before submitting the form.
Another frequent mistake occurs when individuals fail to attach necessary documentation. The C 4 3 form often requires additional medical narratives or attachments for body parts and conditions treated. If these documents are omitted, the Workers' Compensation Board may reject the submission. Always check that you have included all relevant attachments to avoid this issue.
People often neglect to keep copies of the submitted form and attachments. This mistake can be problematic. Without copies, you may find it challenging to track your request or address any questions that arise later. Keeping thorough records of everything submitted is essential for clarity and follow-up.
Many also forget to notify the patient when their information has been submitted. While the provider is responsible for the report, the patient's awareness of the submission can help them prepare for any next steps in their case. Good communication helps in ensuring that the patient remains informed and supportive of the ongoing process.
Finally, a misstep many make is failing to submit the form promptly. Timeliness is crucial in handling matters related to workers' compensation. Delays can result in complications like delayed treatments and benefits. Submitting the form as soon as possible can prevent unnecessary challenges for both the provider and the patient.
Documents used along the form
The C 4 3 form, also known as the Doctor's Report of Maximum Medical Improvement (MMI) and Permanent Partial Impairment, is crucial in the workers' compensation process. Several other forms accompany this report, streamlining communication between medical providers and the Workers' Compensation Board. Below is a list of related documents that frequently support the C 4 3 form.
- C-4.2 - This is the Doctor's Initial Report. It details the initial evaluation of the patient's condition post-injury. This form helps establish a baseline for treatment and is essential in outlining the patient’s medical history and current symptoms.
- C-4.1 - This is the Doctor's Report on Continued Treatment. It provides progress updates on a patient's recovery and the ongoing treatment plan. Regularly submitting this report helps monitor the patient’s state and ensures timely care.
- C-5 - Used for the Attending Ophthalmologist's Report, this form is necessary when vision impairment is involved. It documents the ophthalmologist's findings, which are vital in assessing visual disabilities related to work injuries.
- C-72.1 - This is the report for Occupational Loss of Hearing. It is required when a patient has experienced hearing loss due to their occupation. This form assists in determining compensation eligibility for auditory impairments.
- Attachment A - This is the form used for documenting Permanent Partial Disability related to schedule loss of use. It outlines specific body parts that may have sustained an impairment and provides a framework for determining compensation amounts based on the extent of the injury.
- Attachment B - This document covers Non-Schedule Permanent Partial Disability. It classifies the impairment into various categories, guiding decisions on compensation when the impairment does not fit the scheduled category.
Each of these forms plays a significant role in the workers' compensation process, supporting the documentation needed to assess an injured worker’s condition accurately. Properly completed, they ensure that all parties remain informed and facilitate the necessary approvals for treatment and compensation.
Similar forms
The C 4 3 form is a specialized document used primarily for reporting on a patient's Maximum Medical Improvement (MMI) and Permanent Partial Impairment (PPI). Several other forms serve similar purposes in the realm of workers' compensation. Below is a list of documents that share similarities with the C 4 3 form:
- C-5: Attending Ophthalmologist's Report - This form is used to report on vision-related injuries, similar to how the C 4 3 assesses overall impairment. Both forms require detailed medical narratives that document the patient's conditions and treatments.
- C-72.1: Occupational Loss of Hearing - This document addresses hearing impairments and is comparable to the C 4 3 in that it focuses on specific impairments. It also requires specific measured assessments and connections to the injury details.
- C-4.1: Employee's Claim for Compensation - The C-4.1 form is submitted by employees to claim compensation for work-related injuries, just like the C 4 3. Both forms must be thoroughly filled out and submitted along with relevant medical documentation.
- C-9: Notice of Payment of Compensation - This form notifies parties of compensation payments. Much like the C 4 3, it plays a role in the overall claims process and reinforces communication between the involved parties.
- B-4: Employee's Report of Work-Related Injury or Illness - This document provides details about the injury or illness from the employee's perspective. While the C 4 3 centers on the medical assessment, both are essential to the workers' compensation workflow.
- C-4.2: Medical Authorization Form - This form allows medical providers to release patient information related to a work-related injury. It works alongside the C 4 3, which uses the medical details to assess impairment and MMI.
- D-5: Physician's Report of Medical Examination - This report provides an assessment of an individual's medical condition. Similar to the C 4 3, it is a crucial part of the evaluation process in determining work-related injuries and necessary follow-ups.
Dos and Don'ts
When filling out the C-4.3 form, it is crucial to approach the task with care and clarity. Below are seven guidelines to help ensure that the form is completed correctly. These include both practices to adopt and pitfalls to avoid.
- Do answer all questions completely. Incomplete responses can lead to delays and complications.
- Don’t wait until the last minute to submit the form. Prompt submission is vital for timely processing.
- Do attach any necessary extra pages if additional space is needed. This ensures that your responses are thorough.
- Don’t forget to provide the date(s) of examination. This information is essential for accurate record-keeping.
- Do send copies of the completed form to the patient, attorney, and relevant parties involved. Transparency is important.
- Don’t use vague language or abbreviations that could lead to misunderstandings. Be clear and precise in your descriptions.
- Do review the form for any errors or omissions before submission. A final check can help prevent unnecessary complications.
Misconceptions
Understanding the details around the C 4 3 form can be challenging. Here are six common misconceptions that can lead to confusion:
- Only doctors can fill out the C 4 3 form. Many believe that only licensed medical providers can complete this form. In truth, once a medical professional assesses the patient's condition, any authorized representative can assist with the submission process.
- The C 4 3 form is optional. Some think that this form is just a suggestion. However, submitting the C 4 3 form is often a requirement for processing workers' compensation claims. Without it, important benefits, such as treatment payments, could be delayed.
- Maximum Medical Improvement (MMI) must be declared. There's a misconception that every patient must always reach MMI. However, MMI may not be applicable in all cases. If a patient is still receiving treatment, a doctor can indicate that MMI has not yet been achieved and describe ongoing treatment plans instead.
- All injuries require the same type of documentation. Some people think that every injury documented on the C 4 3 form needs the same details. It's essential to provide specific information tailored to each unique injury or condition listed, including relevant attachments as needed.
- Attachments are optional. Another misunderstanding is that attachments to the C 4 3 form are not necessary. In fact, to support the information provided, if there are complexities related to the injury, attaching additional documents is crucial for a comprehensive evaluation.
- Time delays in filing are acceptable. Many believe that delays in submitting the C 4 3 form will have no consequences. Unfortunately, failing to submit promptly may indeed result in postponed treatment approvals and delayed wage loss benefits.
It's essential to have accurate information about the C 4 3 form to ensure that all required actions are taken efficiently and effectively. Understanding these common misconceptions can help in navigating the workers' compensation process with greater ease.
Key takeaways
Filling out the C-4.3 form, which pertains to a doctor's report on Maximum Medical Improvement (MMI) and Permanent Partial Impairment, is a crucial step in the workers' compensation process. Here are some key takeaways for effectively using this form:
- Purpose of the Form: Utilize this form when offering an opinion on a patient’s MMI status or in response to a request from the Workers' Compensation Board.
- Completeness is Key: Answer all questions fully. If needed, attach extra pages to ensure comprehensive responses.
- Timely Submission: Send the completed form promptly to the Board, insurance carrier, and the patient’s attorney or representative to avoid delays in treatment payment.
- Impact of Delays: Understand that failure to submit can lead to delayed treatment payments and wage loss benefits, as well as potentially requiring testimony later.
- Online Option: You have the option to fill out this form online, which can streamline the process and potentially reduce errors.
- Details Matter: Keep accuracy in mind regarding patient and provider information. This includes names, dates, and addresses.
- Accurate Medical Information: Document any findings on MMI carefully. If the patient has not reached MMI, outline the relevant treatment plan.
- Identification of Impairment: Clearly indicate any permanent partial impairment, detailing the body parts affected per the injury date.
- Attachments: Attach any necessary additional documentation as specified, such as narratives for particular body parts, to support your evaluation.
By paying attention to these important aspects while filling out and utilizing the C-4.3 form, you can help ensure a smoother process for both the patient and the workers' compensation system.
Browse Other Templates
Safeway Sponsorship - Collect all necessary documents before submitting your application.
Mv900 Form - Every detail on the MV-900 form is important for lien verification and title issues.