Fill Out Your C 4 Auth Form
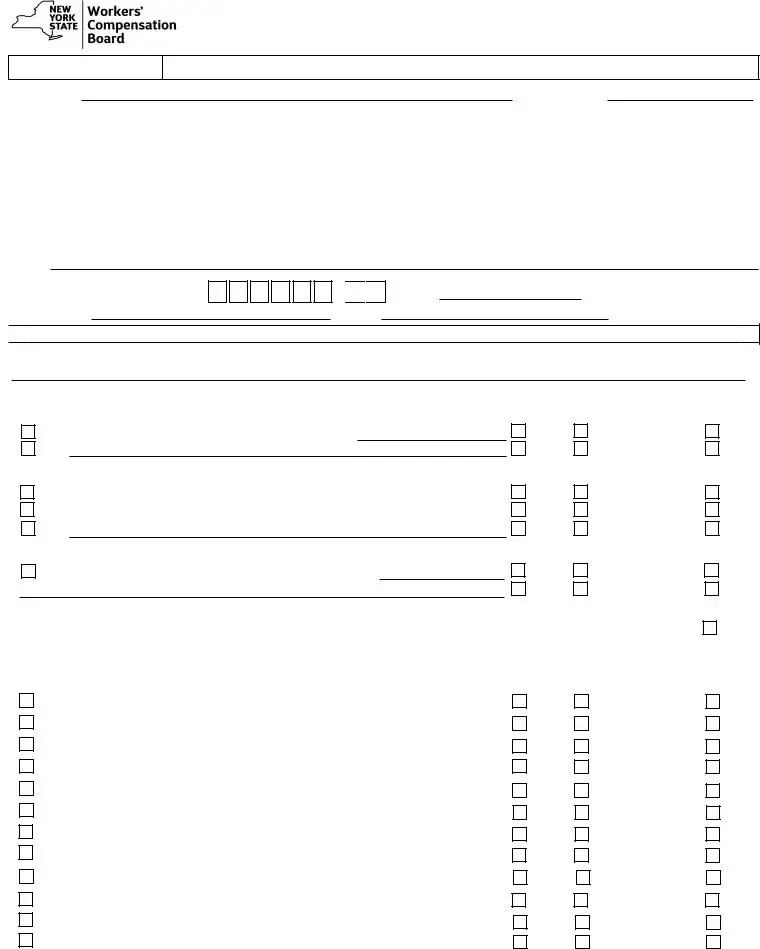
The C-4 Auth form plays a critical role in the process of obtaining necessary medical services for individuals with work-related injuries. Designed specifically for non-emergency situations, this form allows attending doctors to request written authorization for special services that exceed $1,000 or require pre-authorization according to the Medical Treatment Guidelines. Key elements of the form include sections for detailed patient information, the attending physician's details, and a comprehensive authorization request section where specific services or procedures can be identified. Additionally, the attending doctor must articulate the medical necessity of the requested services, ensuring that all parts of the form are completed accurately to avoid delays in the authorization process. Insurers are mandated to respond to these requests within a specified timeframe, with potential consequences for failing to do so. It is important to note that the C-4 Auth form cannot be used for certain injuries, such as those involving the neck or mid and low back unless specified conditions apply. Its proper usage is essential for the efficient handling of workers' compensation claims and to safeguard patients' rights to necessary medical care.
C 4 Auth Example

IMPORTANT:
PLEASE READ CAREFULLY THE FOLLOWING INFORMATION FOR DETERMINING HOW TO FIND
ATTENDING DOCTOR'S REQUEST FOR |
||
AUTHORIZATION AND INSURER'S RESPONSE |
||
AUTH |
||
Answer all questions fully on this report |
WCB Case #:
Claim Administrator Claim (Carrier Case) #: |
Date of Injury/Illness: |
|
|
A. Patient's Name:
Address:
Social Security No.:
First |
MI |
Last |
|
|
|
Number and Street |
City |
State |
Zip Code |
|
Employer Name: |
|
|
|
||||
|
|
|
|
|
|
|
|
Address: |
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
Number and Street |
City |
State |
Zip Code |
|
Insurer Name: |
|
|
|
||||
|
|
|
|
|
|
||
Address: |
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
Number and Street |
City |
State |
Zip Code |
|
B. Attending Doctor's Name: |
|
|
|
||||
|
|
|
|
|
|||
Address: |
|
|
|
||||
Number and Street
Individual Provider's WCB Authorization No.:
Telephone No.:
City
-


Fax No.:
State |
Zip Code |
NPI No.:
C.  AUTHORIZATION REQUEST
AUTHORIZATION REQUEST
The undersigned requests written authorization for the following special service(s) costing over $1,000 or requiring
Authorization Requested:
Diagnostic Tests:
Radiology Services
Other
Therapy (including Post Operative): |
|
|
|
|
|
||
Physical Therapy: |
|
|
times per week for |
weeks |
|||
|
|
|
|
|
|
|
|
Occupational Therapy: |
|
|
times per week for |
weeks |
|||
|
|
|
|
|
|
|
|
Other
Surgery:
Type of Surgery (Describe, include use of hardware/surgical implants)
Treatment:
Insurer Response: if any service
is denied, explain on reverse.
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
|
|
Other |
|
|
|
|
Granted |
|
Granted w/o Prejudice |
Denied |
Medical Treatment Guidelines Procedures Requiring |
(Complete Guideline Reference for each item checked, if necessary. In first box, indicate |
|||||||||
injury and/or condition: K = Knee, S = Shoulder, B = Mid and Low Back, N = Neck, C = Carpal Tunnel, P =
1. |
Lumbar Fusions |
|
B |
|
- |
|
E |
|
4 |
|
a |
|
|
|
|
|
|
............................................................................. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1. |
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
2. Artificial Disk Replacement |
|
|
|
|
|
|
- |
|
|
|
|
E |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
........................................................... |
|
|
|
|
|
|
|
|
|
|
|
2. |
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3. |
Vertebroplasty |
|
|
B |
|
- |
E |
|
7 |
|
|
a |
|
|
|
|
i |
|
|
................................................................................ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3. |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
4. Kyphoplasty |
B |
|
- |
|
E |
|
7 |
|
a |
|
|
i |
|
.................................................................................... |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4. |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
5. |
Electrical Bone Growth Stimulators |
|
|
|
|
|
- |
|
|
E |
|
|
|
|
|
a |
|
|
|
............................................... |
|
|
|
|
|
|
5. |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
6. |
Osteochondral Autograft |
|
K |
- |
|
D |
1 |
|
|
|
|
f |
|
|
|
|
|
................................................................ |
|
|
|
|
|
|
|
|
|
|
|
|
|
6. |
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
7. Autologous Chondrocyte Implantation |
|
|
K |
|
|
D |
|
1 |
|
f |
|
|
|
|
............................................. |
|
|
|
|
7. |
|||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
8. Meniscal Allograft Transplantation |
|
|
|
K |
- |
|
D |
|
|
|
|
|
|
|
|
|
|
|
................................................. |
|
|
|
|
|
|
8. |
|||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||
9. Knee Arthroplasty (total or partial knee joint replacement) |
K |
- |
F |
2 |
|
|
............9. |
||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
10. Spinal Cord Stimulators |
|
P |
|
- |
|
|
G |
|
1 |
|
|
|
|
|
|
|
|
|
|
|
................................................................. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
10. |
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||
11. Intrathecal Drug Delivery (pain pumps) |
|
|
|
P |
|
|
- |
|
G |
|
2 |
|
|
|
|
|
|
|
......................................... |
|
|
|
11. |
||||||||||||||||||||||||||||
12. Second or Subsequent Procedure |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
................................................ |
|
|
|
|
|
|
|
12. |
|||||||||||||||||||||||
Granted
Granted
Granted
Granted
Granted
Granted
Granted
Granted
Granted
Granted
Granted
Granted
Granted w/o Prejudice Granted w/o Prejudice Granted w/o Prejudice Granted w/o Prejudice Granted w/o Prejudice Granted w/o Prejudice Granted w/o Prejudice Granted w/o Prejudice Granted w/o Prejudice Granted w/o Prejudice Granted w/o Prejudice Granted w/o Prejudice
Denied
Denied
Denied
Denied
Denied
Denied
Denied
Denied
Denied
Denied
Denied
Denied
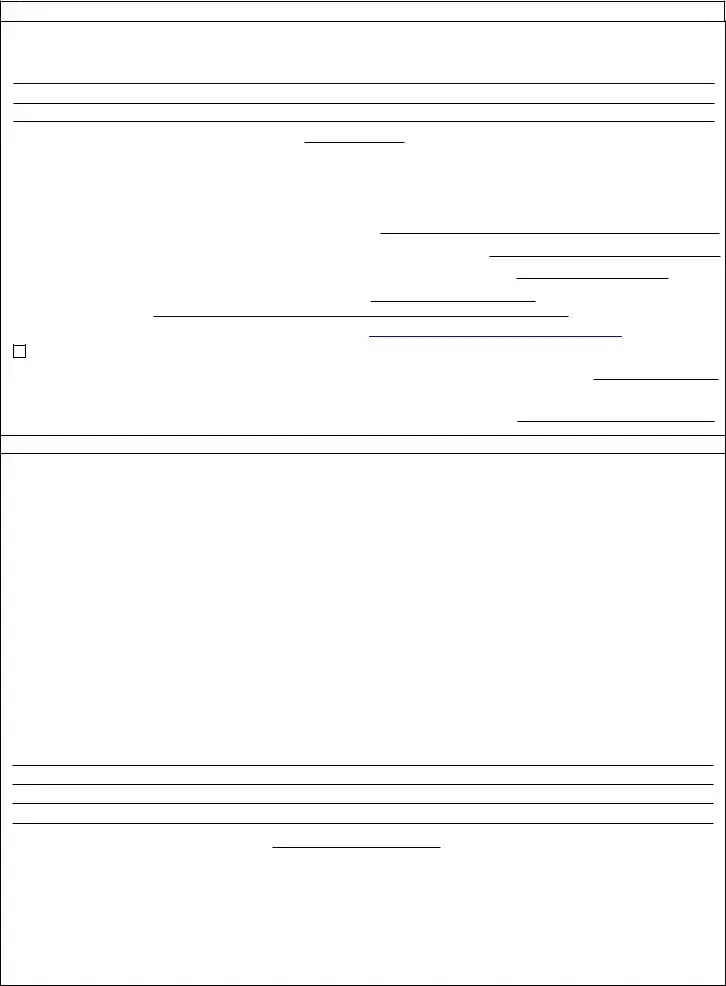
D.
STATEMENT OF MEDICAL NECESSITY
Pursuant to 12 NYCRR
Date of service of supporting medical in WCB Case File: |
(Attach if not already submitted.) |
Pursuant to 12 NYCRR 325.1(a)(3), the treating provider shall submit this form to the Workers' Compensation Board and insurer.
Providers must complete Part A below indicating that the request was sent to the
A.Insurer's designated fax # or email address as provided on the Board's website:
B. If the request was also submitted to another fax # or email address provided by the insurer, provide here:
C.I am not equipped to send or receive forms by fax or email. This form was mailed (return receipt requested) on:
If you called the insurer and spoke with an individual, provide the date of the call: and name of person contacted:
Designated contact information not available.
I certify I am making the above request for certification. This request was made to the insurance
Provider's Signature: |
|
Date: |
Response Time and Notification Required:
The
Denial of the Request for Authorization of a Special Service: A denial of authorization of a special service must be based upon and accompanied by a conflicting second opinion rendered by a physician authorized to conduct IMEs, or record review, or qualified medical professional, or a physician authorized to treat workers' compensation claimants. (If authorization is denied in a controverted case, the conflicting second opinion must address medical necessity only.) Failure to file timely the conflicting second opinion will render the denial defective. If denial of an authorization is based upon claimant's failure to attend an IME examination scheduled within the 30 day authorization period, contemporaneous supporting evidence of claimant's failure must be attached.
Failure to Timely Respond to Form
REASON FOR DENIAL(S), IF ANY. (ATTACH OR REFERENCE CONFLICTING SECOND MEDICAL OPINION AS EXPLAINED ABOVE.)
Date of service of supporting medical in WCB case file:
I certify that the
and
I certify that copies of this form were emailed, faxed, or mailed to the treating provider, the claimant (patient), the claimant's legal representative, if any, the Workers' Compensation Board and all parties of interest on the date below:
By: (print name) |
|
Title: |
||||
Signature: |
|
|
|
|
Date: |
|
www.wcb.ny.gov |
REQUEST FOR WRITTEN AUTHORIZATION
IMPORTANT TO ATTENDING DOCTOR
AUTHORIZATION FOR SPECIAL SERVICES IS NOT REQUIRED IN AN EMERGENCY
1.This form is used for a workers' compensation, volunteer firefighters' or volunteer ambulance workers' benefit case to request written authorization for special service(s) costing over $1,000 in a
2.This form must be signed by the attending doctor and must contain her/his authorization number and code letters.
3.Please ask your patient for his/her WCB case # and the claim administrator claim (carrier case) number and show these numbers on this form. In addition, ask your patient if he/she has retained a representative. If represented, ask for the name and address of the representative.
This request must be sent to the Workers' Compensation Board, and the the workers' compensation insurance carrier,
4.The attending doctor must submit this form with the Board and on the same day serve a copy on the
5.If authorization or denial is not forthcoming within 30 calendar days, (or 35 days if
6.SPECIAL SERVICES - Services for which authorization must be requested are as follows:
Physicians - To engage the services of a specialist, consultant, or a surgeon, or to provide for
Podiatrists - In treating the foot, to provide physiotherapeutic procedures,
Occupational/Physical Therapists - In treating a condition as provided in Article 136 or 156 of the Education Law, in the Workers' Compensation Law, and the Rules of the Chair relative to Occupational/Physical Therapy Practice to provide occupational/physical therapy procedures costing more than $1,000.
Psychologists - Prior authorization for procedures enumerated in section
Medical Treatment Guidelines - Lumbar Fusions, Artificial Disk Replacement, Vertebroplasty, Kyphoplasty, Electrical Bone Growth Stimulators, Spinal Cord Stimulators, Osteochondral Autograft, Autologus Chondrocyte Implantation, Meniscal Allograft Transplantation, Knee Arthroplasty (total or partial knee joint replacement), Intrathecal Drug Delivery (pain pumps).
7.If the insurer has checked "GRANTED WITHOUT PREJUDICE" in Section C, the liability for this claim has not yet been determined. This authorization is made pending final determination by the Board. Pursuant to 12 NYCRR §
8.It is the attending doctor's burden to set forth the medical necessity of the special services required. Be sure to provide this information in the Statement of Medical Necessity section of this form.
9.HIPAA NOTICE - In order to adjudicate a workers' compensation claim,
ANY PERSON WHO KNOWINGLY AND WITH INTENT TO DEFRAUD PRESENTS, CAUSES TO BE PRESENTED, OR PREPARES WITH KNOWLEDGE OR BELIEF THAT IT WILL BE PRESENTED TO OR BY AN INSURER, OR
This form must be served on the
www.wcb.ny.gov by fax, email or mailed, return receipt requested. Failure to submit the form to the designated contact identified on the Board's website may result in your request being denied. A copy of the form must also be filed with the Board.
NYS Workers' Compensation Board
PO Box 5205
Binghamton, NY
Email Filing: wcbclaimsfiling@wcb.ny.gov l |
Customer Service: (877) |
THE WORKERS' COMPENSATION BOARD EMPLOYS AND SERVES PEOPLE WITH DISABILITIES WITHOUT DISCRIMINATION |
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of the Form | The C-4 Auth form requests written authorization for special services exceeding $1,000 in non-emergency situations related to workers' compensation claims. |
| Governing Law | This form operates under the regulations set forth in 12 NYCRR § 325 and the New York Workers' Compensation Law. |
| Response Time Requirement | Insurers must respond to authorization requests within 30 days, or 35 days if mailed with a return receipt requested. Failure to respond timely results in automatic authorization of requested services. |
| Submission Method | The form must be submitted to an insurer's designated contact via fax, email, or normal mail with delivery confirmation to ensure valid processing. |
Guidelines on Utilizing C 4 Auth
Once you have gathered all necessary information, you can begin filling out the C-4 Auth form. This form helps request authorization for certain medical services related to workers’ compensation claims. Ensure you have the insurer's contact details before you proceed. Follow the steps outlined below to complete the form properly.
- Start by entering the WCB Case # and Claim Administrator Claim (Carrier Case) #.
- Add the Date of Injury/Illness.
- Fill in the patient's Name, Address, and Social Security Number.
- Provide the Employer Name and Address.
- Input the Insurer Name and Address.
- Enter the Attending Doctor's Name and Address.
- Write down the Individual Provider's WCB Authorization Number, Telephone Number, Fax Number, and NPI Number.
- In the Authorization Request section, indicate the services you are requesting, including diagnostic tests, physical therapy, and any type of surgery. Be specific about the types of treatments needed.
- As you request authorization, explain the Medical Necessity for the proposed services clearly.
- Provide the insurer's designated fax number or email address as it appears on the Workers' Compensation Board's website.
- If applicable, fill out the section for any additional fax or email addresses where you submitted the request.
- If you can’t send the document electronically, check the box indicating you mailed the form and include the date.
- Sign and date the form at the bottom, confirming that it has been sent to the appropriate parties.
After completing the form, send it to the designated insurer’s contact. Store a copy for your records. Remember that the insurer must respond within 30 days; otherwise, the request may be considered granted. For any additional assistance or clarification, consult the Workers’ Compensation Board's guidelines.
What You Should Know About This Form
What is the purpose of the C 4 Auth form?
The C 4 Auth form is used at the request of attending doctors to seek written authorization for special services related to workers' compensation cases. Specifically, it applies to services that cost over $1,000 or require pre-authorization according to Medical Treatment Guidelines.
Who needs to complete the C 4 Auth form?
This form must be completed by the attending doctor overseeing the patient's care. If the patient is hospitalized, a licensed doctor assigned to the care team may also sign the form. Out-of-state providers need to include their NPI number as well.
How does one determine the insurer or self-insurer's contact information?
The designated contact information for the insurer or self-insurer is available on the Workers' Compensation Board's website at wcb.ny.gov/attending-doctors-request-authorization. Be sure to include the proper contact details on the form.
What crucial information must be included on the form?
Vital details such as the patient's name, Social Security number, date of injury or illness, treating doctor’s information, and specific services requested must be thoroughly filled out on the form. Medical necessity for the treatment should also be explained adequately.
What happens if the insurer does not respond to the authorization request?
If the self-insured employer or insurer fails to provide a written response within 30 days (or 35 days if mailed), the treatment requested will automatically be considered authorized. In such cases, treatment may proceed without further delay.
Are there specific types of services that require authorization?
Yes, services that cost more than $1,000 typically require authorization. This includes consulting with specialists, various diagnostic tests, psychological services, physical therapy, and certain surgical procedures outlined in the Medical Treatment Guidelines.
What does "Granted Without Prejudice" mean?
This term indicates that authorization has been given for the requested treatment, but it does not guarantee the employer or insurer’s liability for payment. The authorization is limited to the question of medical necessity and does not imply an acceptance of the claim as compensable.
What constitutes a denial of authorization?
An authorization request may be denied if the insurer provides a conflicting second opinion from an authorized medical professional. The basis for the denial must be clearly documented, and all supporting evidence should be attached to the denial notice.
What are the consequences of providing false information on the C 4 Auth form?
Providing false information can lead to severe legal consequences. Engaging in such actions may result in criminal charges, substantial fines, and imprisonment, emphasizing the importance of accuracy and honesty when completing the form.
What should a doctor do if they cannot submit the form electronically?
If a doctor cannot send the C 4 Auth form via fax or email, they must mail it with a return receipt requested. Documentation showing that the form was mailed should be retained for record-keeping purposes.
Common mistakes
Completing the C-4 Auth form can be a straightforward task, but there are several common mistakes that applicants often make. Understanding these pitfalls can help ensure that the process goes smoothly and that necessary authorizations are granted on time.
One of the most frequent errors is forgetting to provide the insurer’s designated contact information. This information is crucial and can be found on the Workers’ Compensation Board’s website. Leaving this section blank or incorrectly filled out may lead to delays in authorization. Always double-check that the name, fax number, or email is accurately written.
Another mistake that people make is not fully answering all questions on the form. Complete and thorough responses are vital. Omitting information about the patient’s name, injury details, or specific treatment requested can result in the form being returned for clarification, further prolonging the authorization process.
A common error involves failing to attach supporting medical documentation. The Statement of Medical Necessity section must clearly outline why the requested services are essential for treatment. Without adequate justification, the insurer may deny the request. This documentation should directly relate to the patient's needs and the specifics of the case.
Some applicants also neglect to update the date of service for supporting medical information. This date must reflect when the paperwork was prepared and should coincide with the documentation included. An outdated or incorrect date can raise questions and create unnecessary complications.
Inadequately signing the form is another issue that arises. The attending doctor must provide a signature along with their WCB Authorization Number and NPI Number if applicable. If this signature is missing or incorrect, it can render the request invalid, causing needless delays and frustration.
Timing is also essential. Submitting the form beyond the required time frame can lead to automatic denials. To avoid this, ensure that the form is sent promptly to both the insurer and the Board, ideally on the same day it’s completed. If the 30-day deadline is missed, the request may be deemed automatically approved, which can create confusion.
Lastly, failure to keep copies of all submitted forms can be detrimental. Documentation is key in case there are future disputes or requests for clarification. It's always a good practice to maintain a well-organized record of all correspondence related to the C-4 Auth form.
Documents used along the form
When dealing with the C-4 Auth form, you'll often encounter additional documents that play a vital role in the workers' compensation process. Understanding these forms can streamline your experience and ensure that you provide the necessary information efficiently. Below is a list of commonly used documents that accompany the C-4 Auth form, detailing their purpose and importance.
- WCB Claim Form (C-3): This form initiates a worker's compensation claim. It provides essential details about the injury, including the date, nature of the incident, and any witnesses. Filing this form correctly is crucial for processing claims efficiently.
- Request for Independent Medical Examination (IME): When disputes arise regarding the need for treatment, a request for an IME may be made. This document requests an evaluation from a neutral physician to assess the injured worker’s condition and needs.
- Medical Treatment Guidelines (MTG): This document outlines the standards for medical care in New York. It helps medical providers and insurers determine the appropriate treatment for specific injuries and ensures compliance with regulatory requirements.
- Detailed Medical Reports: Healthcare providers submit these reports to give insurers a comprehensive view of the injury, treatment history, and ongoing care needs. They must detail the medical necessity of services requested and the patient’s response to treatment.
- Insurer's Response Form: This form is used by insurers to respond formally to authorization requests. It indicates whether services are approved, granted without prejudice, or denied, along with the reasons for any denial.
- Notice of Decision: After issues of compensability are resolved, this document communicates the insurer's findings regarding liability and treatment reimbursement. It is an essential record for both the injured worker and their healthcare provider.
- Claimant's Authorization to Release Information: This document allows healthcare providers to share medical information with the insurer, ensuring compliance with privacy regulations while facilitating the claim process.
Being familiar with these documents not only prepares you for the process ahead but also heightens your awareness of the requirements involved. Ensuring all necessary forms are completed and submitted on time can significantly impact the timely approval of essential medical treatments. Act now to protect your rights and access the care you need.
Similar forms
The C-4 AUTH form serves as an important document in the workers’ compensation process, specifically for requesting authorization for specialized services. Similar documents often share a purpose or function within various legal contexts. Here are five documents similar to the C-4 AUTH form:
- Medical Treatment Guidelines (MTG) Report: This document outlines which medical treatments require prior approval in workers' compensation cases, similar to how the C-4 AUTH addresses services that exceed a certain cost threshold. Both require detailed information about the patient’s condition and the requested services.
- Request for Medical Authorization (RMA): Like the C-4 AUTH, the RMA is submitted by a healthcare provider to an insurer to obtain permission for specific treatments or procedures. The process for submission and the necessity for thorough documentation are comparable.
- Claim for Compensation (C-3): This form is filed by workers to initiate a compensation claim after an injury. Both forms require detailed information about the injured worker and the nature of the claim. The C-3 includes requests for benefits, while the C-4 AUTH focuses on pre-authorization for services.
- Occupational Safety and Health Administration (OSHA) Report: Similar to the C-4 AUTH, some OSHA forms are used to report workplace injuries and illnesses. Both sets of documents emphasize the necessity of proper documentation and timely filing to support claims related to worker's compensation.
- Referral for Authorization of Treatment (RAT): This document is utilized when a healthcare provider seeks approval for a specialist or specific treatments. Much like the C-4 AUTH, it details the medical necessity behind a treatment request and ensures that insurance protocols are adhered to.
Understanding these documents facilitates better navigation through the workers' compensation process and enhances the ability to secure necessary medical treatments for injured workers.
Dos and Don'ts
When filling out the C-4 Auth form, attention to detail is essential. Here are ten guidelines to keep in mind:
- Do ensure that all required information is complete. Missing information could delay processing.
- Do precisely identify the insurer's designated contact. This information is critical for communication.
- Do submit the form promptly. This will avoid potential delays in authorization.
- Do attach any necessary supporting documentation. This strengthens the request for authorization.
- Do provide clear medical necessity explanations. This must align with guidelines to avoid denials.
- Don’t use the form for non-compensable conditions. It is strictly for authorized workers' compensation claims.
- Don’t neglect to check if the information provided is current. Outdated contact details can lead to rejection.
- Don’t forget to send a copy to the patient. Keeping them informed fosters good communication.
- Don’t submit the form without the appropriate signatures. Incomplete forms may be considered invalid.
- Don’t misinterpret "Granted Without Prejudice." This does not confirm liability; be cautious with this wording.
Following these guidelines will streamline the authorization process and minimize complications. It's crucial to maintain accuracy and clarity throughout the C-4 Auth form submission.
Misconceptions
Understanding the C 4 Auth form is crucial for effective communication between healthcare providers and insurance companies within the workers' compensation system. However, several misconceptions can lead to confusion about how to properly use this form. Here are five common misconceptions, explained for clarity:
- Misconception 1: The C 4 Auth form can be used for all types of injuries.
- Misconception 2: Information on the insurer's designated contact is not important.
- Misconception 3: Authorization is always granted for special services.
- Misconception 4: The request for authorization can be submitted any time after the treatment is given.
- Misconception 5: Only the healthcare provider can submit the C 4 Auth form.
This is untrue. The C 4 Auth form specifically excludes injuries or illnesses involving the mid and low back, neck, knee, shoulder, carpal tunnel syndrome, and non-acute pain, unless they are part of listed procedures that require pre-authorization. Ensure you're using the correct form for your specific situation.
This is not correct. The form requires the name and contact details of the insurer's designated representative as listed on the Workers' Compensation Board website. Failing to provide accurate contact information may result in your authorization request being denied.
Authorization is not guaranteed. The insurer may grant, deny, or grant with prejudice depending on various factors, including the medical necessity of the requested service. Providers must provide a solid justification in the Statement of Medical Necessity section to improve chances of approval.
This is misleading. The request for authorization must be submitted prior to providing treatment costing over $1,000, unless it’s an emergency. If the insurer does not respond within 30 days (or 35 days if mailed), the treatment may automatically be deemed authorized.
While the healthcare provider typically submits the form, there are instances where the injured worker or their representative can assist. It's vital that all parties stay informed and communicate effectively about the submission process and necessary follow-ups.
Key takeaways
1. The C-4 Auth form is utilized to request written authorization for special services costing over $1,000 within a non-emergency context, specifically for workers' compensation cases.
2. It is essential to fully answer all questions on the form, including pertinent details such as the patient's WCB case number and the claim administrator claim number.
3. The designated insurer or self-insurer's contact information must be sourced from the Workers' Compensation Board's website. Failure to do so may jeopardize the approval of the request.
4. This form must be submitted to the insurer via fax or email, but if those options are unavailable, mailing with return receipt is acceptable. The request must also be sent to the Workers' Compensation Board.
5. A response from the insurer is required within 30 days (or 35 days if mailed). If there is no response, the requested treatment is automatically deemed authorized.
6. It's critical that the attending physician clearly articulates medical necessity in the relevant section of the form, as this is required for the appropriate approval of services.
Browse Other Templates
Edd Account Locked - The signature section assures that the individual signing has the authority to act on behalf of the business.
Alaska Oil - CoachXO.com provides various play options against different opponents.
Bmcc Immunization Form - Send your deposit early to avoid any last-minute issues.