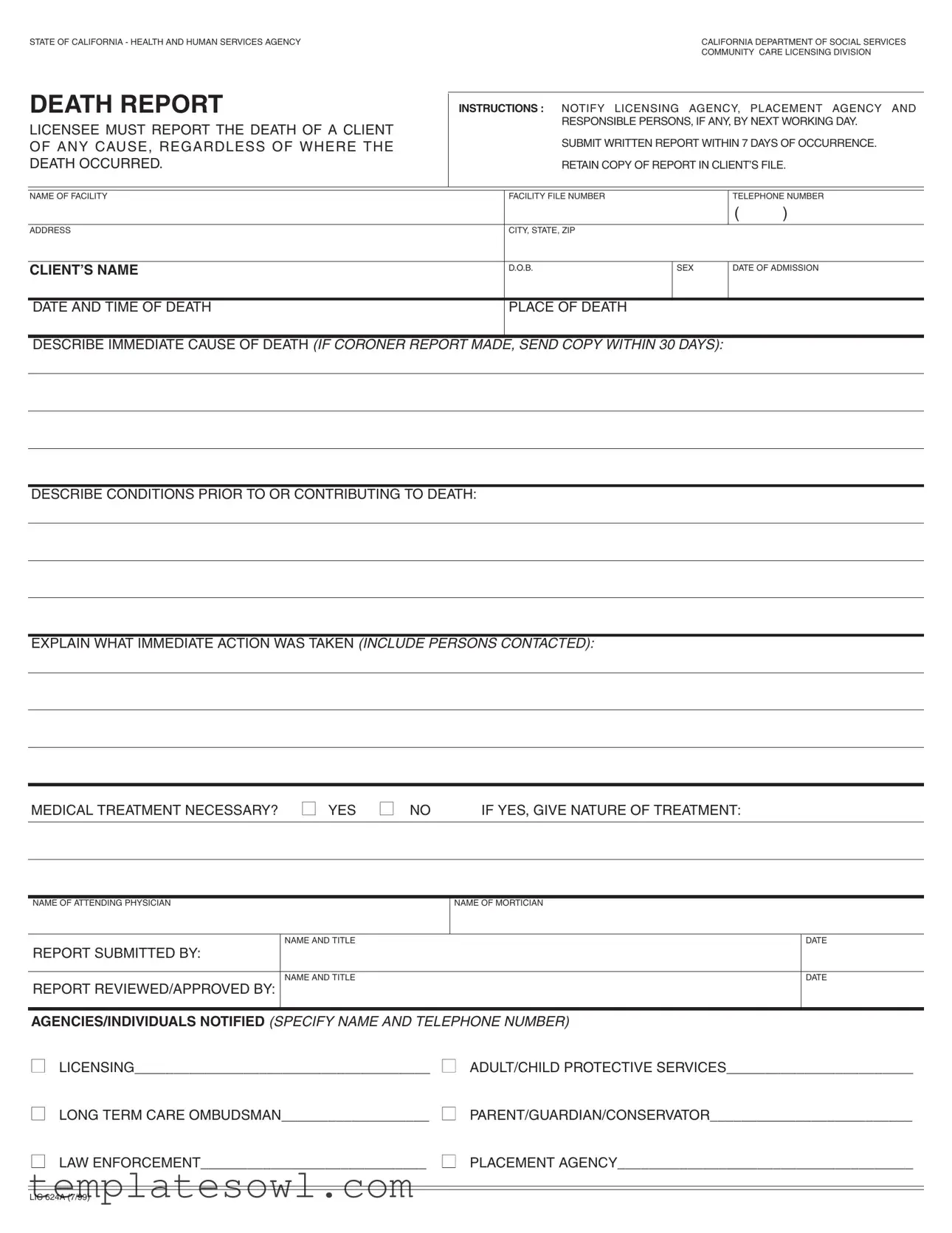
Fill Out Your Ca Death Report Form
The California Death Report form serves a crucial role in documenting the death of clients within various facilities regulated by the California Department of Social Services. This form must be completed by the responsible individuals and submitted within strict timeframes: reporting the death by the next working day and submitting a written report within seven days of the occurrence. Essential details are gathered, including the facility name, file number, and contact information, alongside specific information about the deceased, such as their name, date of birth, sex, and dates of admission and death. The form requires a description of the immediate cause of death and any contributing conditions, ensuring a comprehensive understanding of the circumstances. It also prompts the reporter to outline any immediate action taken following the death and whether medical treatment was necessary. Names and contact details of key individuals—such as the attending physician and mortician—must be included, alongside a record of agencies or individuals notified about the death, like licensing, protective services, and law enforcement. Keeping a copy of this report in the client’s file is mandatory, reflecting the thorough and responsible approach expected in these sensitive situations.
Ca Death Report Example
STATE OF CALIFORNIA - HEALTH AND HUMAN SERVICES AGENCY |
CALIFORNIA DEPARTMENT OF SOCIAL SERVICES |
|
COMMUNITY CARE LICENSING DIVISION |
DEATH REPORT |
INSTRUCTIONS : NOTIFY LICENSING AGENCY, PLACEMENT AGENCY AND |
||||||
LICENSEE MUST REPORT THE DEATH OF A CLIENT |
|
RESPONSIBLE PERSONS, IF ANY, BY NEXT WORKING DAY. |
|||||
|
|
|
|
|
|
||
OF ANY CAUSE, REGARDLESS OF WHERE THE |
|
SUBMIT WRITTEN REPORT WITHIN 7 DAYS OF OCCURRENCE. |
|||||
DEATH OCCURRED. |
|
RETAIN COPY OF REPORT IN CLIENT’S FILE. |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NAME OF FACILITY |
|
FACILITY FILE NUMBER |
|
TELEPHONE NUMBER |
|||
|
|
|
|
|
( |
) |
|
|
|
|
|
|
|
|
|
ADDRESS |
|
CITY, STATE, ZIP |
|
|
|
|
|
|
|
|
|
|
|
|
|
CLIENT’S NAME |
|
D.O.B. |
SEX |
DATE OF ADMISSION |
|||
|
|
|
|
|
|
|
|
DATE AND TIME OF DEATH |
|
PLACE OF DEATH |
|
|
|
|
|
|
|
|
|
|
|
|
|
DESCRIBE IMMEDIATE CAUSE OF DEATH (IF CORONER REPORT MADE, SEND COPY WITHIN 30 DAYS): |
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DESCRIBE CONDITIONS PRIOR TO OR CONTRIBUTING TO DEATH: |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
EXPLAIN WHAT IMMEDIATE ACTION WAS TAKEN (INCLUDE PERSONS CONTACTED): |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MEDICAL TREATMENT NECESSARY? ■ YES ■ NO |
IF YES, GIVE NATURE OF TREATMENT: |
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NAME OF ATTENDING PHYSICIAN |
NAME OF MORTICIAN |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
NAME AND TITLE |
|
|
|
|
|
DATE |
REPORT SUBMITTED BY: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NAME AND TITLE |
|
|
|
|
|
DATE |
REPORT REVIEWED/APPROVED BY: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
AGENCIES/INDIVIDUALS NOTIFIED (SPECIFY NAME AND TELEPHONE NUMBER)
■LICENSING______________________________________ ■ ADULT/CHILD PROTECTIVE SERVICES________________________
■LONG TERM CARE OMBUDSMAN___________________ ■ PARENT/GUARDIAN/CONSERVATOR__________________________
■LAW ENFORCEMENT_____________________________ ■ PLACEMENT AGENCY______________________________________
LIC 624A (7/99)
Form Characteristics
| Fact Name | Details |
|---|---|
| Governing Law | The reporting of client deaths is governed by California Code of Regulations, Title 22, Section 87212. |
| Reporting Timeline | Licensing agencies, placement agencies, and licensees must be notified of a client’s death within the next working day. |
| Written Report Requirement | A written report detailing the death must be submitted within seven days of the incident. |
| Retention of Report | Facilities are required to retain a copy of the death report in the client's file for future reference. |
| Immediate Cause of Death | The report should describe the immediate cause of death. If a coroner's report is available, a copy must be sent within thirty days. |
| Medical Treatment | The report must indicate whether medical treatment was necessary, and if so, the nature of that treatment should be detailed. |
| Responsible Persons | Identification of responsible persons involved prior to or contributing to the death is essential in the report. |
| Agencies Notification | The report requires listing of all notified agencies and individuals, including law enforcement and protective services, with their contact details. |
Guidelines on Utilizing Ca Death Report
After filling out the California Death Report form, the next step involves submitting the completed document to the appropriate agencies. Ensure you retain a copy for your records. The report needs to be filed in a timely manner, particularly if any follow-up actions are required.
- Gather necessary information, including the name and contact details of your facility.
- Fill in the facility file number and telephone number.
- Complete the address section with the city, state, and ZIP code.
- Enter the client's full name along with their date of birth and sex.
- Provide the date of admission for the client.
- Record the date and time of death.
- Specify the place of death clearly.
- Describe the immediate cause of death, and if a coroner's report exists, note that you will send a copy within 30 days.
- Outline any conditions that were present prior to or contributed to the death.
- Explain the immediate actions taken following the death, including all persons contacted.
- Indicate whether medical treatment was necessary by choosing 'Yes' or 'No.' If yes, give details on the nature of that treatment.
- Enter the name of the attending physician.
- Include the name of the mortician.
- Sign your name and title in the section provided for the person submitting the report.
- Include the date the report was submitted.
- Have the report reviewed and approved, filling in the names and titles in the designated areas.
- Notify the relevant agencies or individuals, providing their names and telephone numbers as required.
What You Should Know About This Form
What is the purpose of the California Death Report form?
The California Death Report form is used to notify the relevant authorities about the death of a client in care. This includes the licensing agency, placement agency, and any responsible persons. Reporting ensures compliance with state regulations and allows for proper oversight and investigation if necessary.
Who is required to submit the Death Report?
The licensee of the facility must submit the Death Report. Additionally, any responsible persons associated with the client must also be notified. This includes caregivers and facility staff involved in the client's care.
When must the Death Report be submitted?
The report must be submitted within 7 days of the client's death. Moreover, the responsible parties must notify the appropriate licensing agency and placement agency by the next working day after the death occurs.
What information is needed on the Death Report?
Key details required on the report include the client’s name, date of birth, sex, date and time of death, cause of death, any contributing conditions, and actions taken immediately after the death. The form also requires names of involved medical personnel and agencies notified regarding the death.
What should be done if a coroner's report is made?
If a coroner's report is issued, a copy must be submitted with the Death Report within 30 days of the client’s death. This ensures that the licensing agency has all the relevant information for review.
Where should copies of the Death Report be kept?
A copy of the Death Report should be retained in the client's file at the facility. This documentation may be crucial for future audits and for maintaining accurate records regarding the care provided to the client.
Common mistakes
Filling out the California Death Report form can be a straightforward process, yet many individuals make critical errors that could delay necessary actions. One common mistake is failing to submit the report within the mandated timeframe. The licensee must notify the relevant agencies and submit the written report within seven days of the death occurring. Missing this deadline can lead to compliance issues.
Another frequent error involves incomplete or inaccurate information about the deceased. For example, ensuring that the client’s name, date of birth, and other personal details are correct is essential. If these details are incorrect, it can complicate record-keeping and any subsequent investigations.
Inadequate descriptions of the cause of death and contributing factors also present a serious issue. The form requires a clear explanation of the immediate cause of death. Providing vague or minimal information can hinder proper documentation and lead to unwanted questions in the future.
Additionally, some individuals neglect to mention actions taken immediately after the death or the people contacted. This omission might create confusion regarding the response to the situation. Detailed documentation of the immediate actions and who was informed can significantly aid in clarifying events surrounding the death.
Indicating whether medical treatment was necessary is another area where mistakes occur. Respondents may mistakenly select "no" when treatment was, in fact, needed. This leads to discrepancies in care records and can affect the investigations initiated thereafter.
Often, the individuals filling out the form forget to include the names and contact information of all relevant parties notified, including law enforcement and protective services. Failure to document this properly could result in complications during follow-up procedures.
Lastly, a lack of proper review and approval of the report before submission is a critical error that should not be overlooked. It is vital to have the form reviewed by someone knowledgeable to ensure all sections are completed correctly. This practice helps to prevent misunderstandings and ensures that all necessary actions have been reported accurately.
Documents used along the form
The California Death Report form plays a crucial role in documenting the death of individuals in care facilities. Several other forms and documents are often used in conjunction with this report. Below is a list of these supportive documents along with brief descriptions of their purposes.
- Coroner’s Report: This document provides official findings related to the cause of death. It is generated by the coroner's office and is required for certain types of deaths, especially those that are sudden or unexplained.
- Autopsy Report: Conducted when additional investigation is necessary, the autopsy report details the medical examination of the deceased. It helps determine any underlying issues that may have contributed to the death.
- Medical Records: These files contain the individual’s complete medical history, including treatments received and assessments made prior to the death. They are essential for understanding the health context of the deceased.
- Incident Report: This document records the specific circumstances of the individual’s death, especially if it involved a fall, injury, or other incident that may need further review or investigation.
- Facility’s Licensing Report: This report summarizes compliance with state regulations around patient care and safety. It can be important in evaluating the facility's practices leading up to the death.
- Patient Care Plan: A detailed outline of care strategies and interventions tailored for the client. This plan reveals the agreed-upon actions and therapies that were to be implemented during their care.
- Notification to Next of Kin: A formal document confirming that the family or legal guardians have been informed of the patient’s death. This ensures transparency and communication with the loved ones.
- Grievance Report: Filed if the family or other parties raise concerns regarding the care or treatment received before the client's death. This report assists in addressing complaints and ensuring accountability.
- Adverse Event Report: This form is used to document any unexpected events that may have contributed to the death. It tracks incidents that could potentially reveal systemic issues in care delivery.
- Death Certificate: Issued by the government, this legal document officially declares the individual’s death and typically includes essential details such as cause and date of death.
Understanding these documents and their roles can help ensure that all necessary protocols are followed when a client passes away. Proper documentation not only assists in facilitating the mourning process for families but also contributes to improving care standards within facilities.
Similar forms
- Death Certificate: This document officially records an individual's death. It includes similar identifying information such as the deceased's name, date of birth, and cause of death, ensuring accurate record-keeping for legal and health purposes.
- Obituary: Often published in newspapers, an obituary summarizes the life and death of a person. It contains essential details like the name, date of death, and often a brief account of the circumstances leading to the death.
- Coroner’s Report: A report produced after an investigation into a death, especially if it was sudden or unexplained. Much like the Ca Death Report, it outlines the cause of death and circumstances surrounding it, though it tends to be more formal and investigative in nature.
- Morgue Report: Generated during the examination of a deceased person, this document provides detailed findings regarding the condition of the body. It is similar in that it may also address causes and contributing factors related to the death.
- Medical Record Summary: This compilation of a patient’s medical history includes information about treatments and conditions prior to death. It parallels the Ca Death Report by documenting significant medical happenings leading to the individual’s death.
- Incident Report: Used in various settings including healthcare and residential facilities, it documents unexpected events and outcomes. Like the Ca Death Report, it includes details about immediate actions taken following the incident.
- Autopsy Report: A detailed examination report that follows an autopsy of the deceased. It shares similarities through thorough documentation of findings related to the cause of death and contributing factors, providing a clear medical analysis.
- Facility Incident Log: This record is kept by care facilities to track incidents affecting residents. It resembles the Ca Death Report by noting occurrences and actions taken, ensuring accountability and transparency in care environments.
Dos and Don'ts
When filling out the California Death Report form, it is essential to follow certain guidelines to ensure the process is handled correctly. Here are nine important do's and don'ts.
- Do report the death to the licensing agency immediately, by the next working day.
- Don't delay submitting the written report; it must be submitted within seven days of the death.
- Do provide accurate client information, including the name, date of birth, and date of admission.
- Don't leave out the details regarding the immediate cause of death and any relevant conditions that contributed to it.
- Do explain the immediate actions taken following the client's death, including who was contacted.
- Don't forget to document whether medical treatment was necessary and, if so, the nature of that treatment.
- Do retain a copy of the report in the client's file for future reference.
- Don't omit the names of individuals notified, including their roles and contact information.
- Do ensure that the report is reviewed and approved by the appropriate personnel before submission.
Adhering to these guidelines helps maintain clarity and compliance when reporting a death, ensuring that all responsible parties are informed and necessary actions are documented.
Misconceptions
There are several misconceptions surrounding the California Death Report form. Clarifying these can aid in proper understanding and compliance with regulations.
- The report is only necessary for suspicious deaths. In fact, any death must be reported, regardless of the circumstances surrounding it.
- It is acceptable to report a death after several days. The licensee must report the death by the next working day and submit a written report within seven days of the occurrence.
- The form is not mandatory for all facilities. All licensed facilities must use the form when a client dies, as mandated by agency policy.
- Only medical professionals are responsible for completing the report. The licensee or responsible person is required to complete the report, not just medical staff.
- It is unnecessary to notify authorities if a coroner is involved. Even with a coroner, the facility must still notify licensing agencies and other relevant parties.
- The report is confidential and does not need to be retained. A copy of the report must be kept in the client’s file for record-keeping and accountability.
- The immediate cause of death can be vague or incomplete. Describing the immediate cause clearly is essential, particularly if a coroner’s report is available.
- Notifying the family is optional. The family or legal guardian must also be informed, as part of the notification requirements.
Key takeaways
Filling out the California Death Report form requires careful attention and timeliness. The following key takeaways can guide individuals through this important process.
- Immediate Notification: It is essential to notify the licensing agency, placement agency, and any responsible persons within one working day of the client's death.
- Written Report Deadline: A written report must be submitted within seven days of the occurrence of the death. This serves to document the event officially.
- Retain Records: A copy of the completed report should be retained in the client’s file for future reference and compliance purposes.
- Detailed Description: The form requires clear descriptions of the immediate cause of death, conditions contributing to it, and actions taken. Each section should be filled out comprehensively.
- Communication with Medical Personnel: If medical treatment was necessary, this must be indicated, along with details about the nature of that treatment. Include the names of the attending physician and mortician.
- Notify Relevant Parties: It is important to list all agencies and individuals notified about the death, ensuring that all relevant parties are informed promptly.
These takeaways highlight the essential steps in filling out and using the California Death Report form. Ensuring accuracy and adhering to deadlines reflects the compassion and professionalism required in such sensitive situations.
Browse Other Templates
When Can I Apply for Enhanced Star Program - The form includes sections for additional owners or spouses, ensuring comprehensive data collection.
Nj Real Estate Contract - Details regarding the handling of disputes over escrow funds are included.