Fill Out Your Ca Participating Application Form
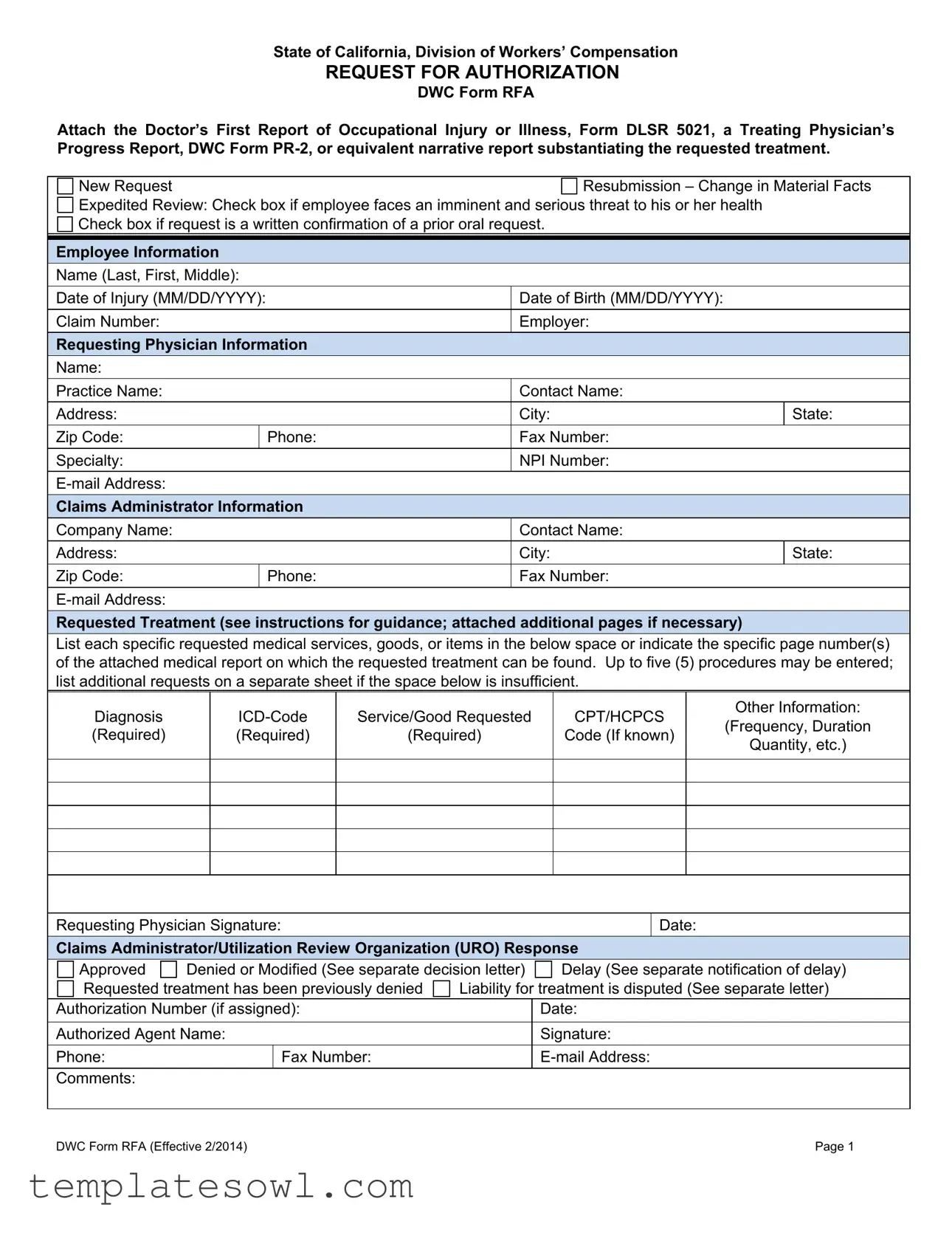
The California Participating Application form, also known as DWC Form RFA, plays a crucial role in the Workers' Compensation system. It serves as a formal request for authorization of medical treatment needed by an injured employee. This essential document must be filled out completely by the employee’s treating physician and includes information such as the patient's name, date of injury, and the claim number. To ensure the request is valid, it requires the attachment of supporting documentation, which could be the Doctor’s First Report of Occupational Injury or Illness or a Treating Physician’s Progress Report. The form provides specific checkboxes that help clarify whether the application is a new request, a resubmission due to changes in the employee's condition, or a request for expedited review due to an imminent health threat. Furthermore, the requested treatment section demands detailed descriptions of medical services, diagnostic codes, and any relevant information regarding the frequency and duration of treatment. Clearly articulated physician details and a signature verify the authenticity of the request. Once submitted, the claims administrator is tasked with responding within defined timeframes, providing either approval or detailed reasons for any denials, ensuring that the process is as transparent as possible for all parties involved.
Ca Participating Application Example
State of California, Division of Workers’ Compensation
REQUEST FOR AUTHORIZATION
DWC Form RFA
Attach the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form
New Request |
|
Resubmission – Change in Material Facts |
||
Expedited Review: Check box if employee faces an imminent and serious threat to his or her health |
|
|||
Check box if request is a written confirmation of a prior oral request. |
|
|||
|
|
|
|
|
Employee Information |
|
|
|
|
Name (Last, First, Middle): |
|
|
|
|
|
|
|
|
|
Date of Injury (MM/DD/YYYY): |
|
Date of Birth (MM/DD/YYYY): |
|
|
|
|
|
|
|
Claim Number: |
|
Employer: |
|
|
Requesting Physician Information |
|
|
||
Name: |
|
|
|
|
|
|
|
|
|
Practice Name: |
|
Contact Name: |
|
|
|
|
|
|
|
Address: |
|
City: |
State: |
|
|
|
|
|
|
Zip Code: |
|
Phone: |
Fax Number: |
|
|
|
|
|
|
Specialty: |
|
NPI Number: |
|
|
|
|
|
||
Claims Administrator Information |
|
|
||
Company Name: |
|
Contact Name: |
|
|
|
|
|
|
|
Address: |
|
City: |
State: |
|
|
|
|
|
|
Zip Code: |
|
Phone: |
Fax Number: |
|
|
|
|
|
|
|
|
|
||
Requested Treatment (see instructions for guidance; attached additional pages if necessary)
List each specific requested medical services, goods, or items in the below space or indicate the specific page number(s) of the attached medical report on which the requested treatment can be found. Up to five (5) procedures may be entered; list additional requests on a separate sheet if the space below is insufficient.
|
Diagnosis |
|
Service/Good Requested |
|
CPT/HCPCS |
|
Other Information: |
||||
|
|
|
|
(Frequency, Duration |
|||||||
|
(Required) |
|
(Required) |
(Required) |
|
Code (If known) |
|
||||
|
|
|
|
Quantity, etc.) |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Requesting Physician Signature: |
|
|
|
|
Date: |
|
||||
|
Claims Administrator/Utilization Review Organization (URO) Response |
|
|||||||||
|
Approved |
Denied or Modified (See separate decision letter) |
|
Delay (See separate notification of delay) |
|||||||
|
Requested treatment has been previously denied |
Liability for treatment is disputed (See separate letter) |
|||||||||
|
Authorization Number (if assigned): |
|
|
Date: |
|
||||||
|
|
|
|
|
|
|
|
||||
|
Authorized Agent Name: |
|
|
Signature: |
|
||||||
|
|
|
|
|
|
|
|
||||
|
Phone: |
|
|
Fax Number: |
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
Comments: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
DWC Form RFA (Effective 2/2014) |
|
|
|
|
|
|
Page 1 |
|||

Instructions for Request for Authorization Form
Warning: Private healthcare information is contained in the Request for Authorization for Medical Treatment, DWC Form RFA. The form can only go to other treating providers and to the claims administrator.
Overview: The Request for Authorization for Medical Treatment (DWC Form RFA) is required for the employee’s treating physician to initiate the utilization review process required by Labor Code section 4610. A Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form
Checkboxes: Check the appropriate box at the top of the form. Indicate whether:
This is a new treatment request for the employee or the resubmission of a previously denied request based on a change in material facts regarding the employee’s condition. A resubmission is appropriate if the facts that provided the basis for the initial utilization review decision have subsequently changed such that the decision is no longer applicable to the employee’s current condition. Include documentation supporting your claim.
Review should be expedited based on an imminent and serious threat to the employee’s health. A request for expedited review must be supported by documentation substantiating the employee’s condition.
The request is a written confirmation of an earlier oral request.
Routing Information: This form can be mailed, faxed, or
Requested Treatment: The DWC Form RFA must contain all the information needed to substantiate the request for authorization. If the request is to continue a treatment plan or therapy, please attach documentation indicating progress, if applicable.
List the diagnosis (required), the ICD Code (required), the specific service/good requested (required), and applicable CPT/HCPCS code (if known).
Include, as necessary, the frequency, duration, quantity, etc. Reference to specific guidelines used to support treatment should also be included.
For requested treatment that is: (a) inconsistent with the Medical Treatment Utilization Schedule (MTUS) found at California Code of Regulations, title 8, section 9792.20, et seq.; or (b) for a condition or injury not addressed by the MTUS, you may include scientifically based evidence published in
Requesting Physician Signature: Signature/Date line is located under the requested treatment box. A signature by the treating physician is mandatory.
Claims Administrator/URO Response: Upon receipt of the DWC Form RFA, a claims administrator must respond within the timeframes and in the manner set forth in Labor Code section 4610 and California Code of Regulations, title 8, section 9792.9.1. To communicate its approval on requested treatment, the claims administrator may complete the lower portion of the DWC Form RFA and fax it back to the requesting provider. (Use of the DWC Form RFA is optional when communicating approvals of treatment; a claims administrator may utilize other means of written notification.) If multiple treatments are requested, indicate in comments section if any individual request is being denied or referred to utilization review.
DWC Form RFA (Effective 2/2014) |
Page 2 |
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Purpose | The DWC Form RFA allows a physician to request authorization for medical treatment under California's workers' compensation system. |
| Required Attachments | Submit the Doctor’s First Report of Occupational Injury or Illness (Form DLSR 5021) or a Treating Physician’s Progress Report (DWC Form PR-2) with the form. |
| Submission Options | The form can be mailed, faxed, or emailed to the designated claims administrator. |
| Response Timeframe | Claims administrators must respond to the requests within specified time limits according to Labor Code section 4610. |
| Utilization Review | The form initiates the utilization review process as mandated by California law, ensuring proper medical treatment authorization. |
| Expiration Information | The form is effective as of February 2014, and must be used by practitioners in compliance with ongoing regulations. |
Guidelines on Utilizing Ca Participating Application
Filling out the California Participating Application form is an important step in the process of requesting medical treatment authorization. It is essential to ensure that all required information is accurately provided to facilitate a smooth review process. Below are the steps to complete the form effectively.
- Read the Instructions: Before starting, familiarize yourself with the requirements and components of the form.
- Check the Appropriate Box: At the top of the form, indicate whether this is a new request, a resubmission based on a change in material facts, or a request for expedited review.
- Fill Out Employee Information: Provide the employee's name, date of injury, date of birth, claim number, and employer’s details in the designated fields.
- Enter Requesting Physician Information: Include the physician’s name, practice name, contact name, address, city, state, zip code, phone number, fax number, specialty, NPI number, and email address.
- Complete Claims Administrator Information: Provide the name of the claims administrator, contact name, address, city, state, zip code, phone number, fax number, and email address.
- List the Requested Treatment: Clearly specify the medical services, goods, or items being requested, including diagnosis ICD-code, CPT/HCPCS code, quantity, and any other relevant information. If necessary, attach additional pages.
- Obtain the Signature: The requesting physician must sign and date the form at the bottom of the requested treatment section.
- Submit the Form: Mail, fax, or email the completed form to the claims administrator using the contact details provided.
Following these steps ensures that the application is complete, thereby helping to expedite the review and authorization of the requested medical treatment. Be sure to keep copies of all documents sent for your records as well.
What You Should Know About This Form
What is the purpose of the CA Participating Application Form?
The CA Participating Application Form, also known as the Request for Authorization (DWC Form RFA), is used by an employee's treating physician to initiate the process of obtaining authorization for medical treatment or services covered under California's workers' compensation system. It serves as a formal request to the claims administrator for non-emergency treatment based on the employee's work-related injury or illness.
What documents must be attached to the application?
When submitting the DWC Form RFA, it’s essential to attach certain initial reports that substantiate the request for treatment. This includes a Doctor’s First Report of Occupational Injury or Illness (Form DLSR 5021) or a Treating Physician’s Progress Report (DWC Form PR-2). These reports provide necessary context and evidence for the requested treatment, ensuring proper review by the claims administrator.
What information is required on the form?
Several essential details must be filled out on the DWC Form RFA. You will need to provide the employee's full name, date of injury, date of birth, claim number, and employer's name. The requesting physician's information, including their name, practice name, contact details, and applicable specialty, must also be included. Lastly, details about the requested treatment, including diagnosis, specific services, and codes, are critical for review.
How do I indicate if this is an urgent request?
If the request for treatment is urgent, there's a specific section at the top of the DWC Form RFA where you can check a box indicating the request should be expedited due to an imminent and serious threat to the employee’s health. This helps prioritize the review process for urgent cases.
Can I resubmit a previously denied request?
Yes, if there's been a change in material facts regarding the employee's condition, you can resubmit a previously denied request. You must indicate that this is a resubmission on the form and provide supporting documentation that shows the changes to the employee's condition, justifying a different review outcome.
What should I do if there are multiple treatment requests?
In cases where you are requesting multiple treatments, you can list up to five procedures on the DWC Form RFA. If you require additional entries, you should attach a separate sheet. The claims administrator needs all the details to effectively review each request, especially if some treatments may need different justifications.
What happens after I submit the DWC Form RFA?
Upon receiving the form, the claims administrator is required to respond within specific timeframes outlined in California workers' compensation laws. They can either approve, deny, or modify the request. The administrator may communicate their decision back using the lower portion of the RFA or through other written means. You will likely receive a decision letter detailing the outcome of your request.
Do I need a signature on the form?
Yes, a signature from the treating physician is mandatory. This indicates that the physician has reviewed the request and stands by the information provided in the DWC Form RFA. The signature is typically located at the bottom of the treatment request section.
What if my requested treatment is not consistent with established guidelines?
If the requested treatment is inconsistent with the Medical Treatment Utilization Schedule (MTUS) or concerns an injury not covered by the MTUS, you may include scientific evidence from peer-reviewed journals to support your request. Providing this information can help justify the need for the specific treatment being requested.
How is private healthcare information handled?
It’s important to recognize that the DWC Form RFA contains sensitive private healthcare information. The form can only be shared with other treating physicians and the claims administrator. Care should be taken to protect this information throughout the submission and review process.
Common mistakes
Completing the California Participating Application form can be straightforward, but mistakes can lead to delays or denials of treatment requests. One common error is failing to attach necessary documentation. This form requires specific reports, including the Doctor’s First Report of Occupational Injury or Illness and a Treating Physician’s Progress Report. Without these, the request might be incomplete, causing extra steps later.
Another frequent mistake is neglecting to check the appropriate box at the top of the form. Applicants sometimes forget to indicate whether they are making a new request or resubmitting a previous one. Ensuring this box is checked is crucial because it clarifies the nature of the request and ensures that it is processed correctly.
People also often overlook the importance of providing detailed treatment descriptions. The form must include specific diagnoses, ICD codes, and requested services or goods. Writing vague or incomplete details can confuse claims administrators and lead to unnecessary back-and-forth communication.
Many applicants fail to sign the form. The requesting physician's signature is mandatory, and without it, the claims administrator cannot process the request. This simple step is often dismissed, leading to further delays and complications.
Some individuals mistakenly assume that all treatment requests can fit within the designated space on the form. However, if more than five procedures need to be listed, they should use a separate sheet. Including too much information in the provided section can result in missed requests and incomplete applications.
Lastly, it's crucial to keep copies of everything submitted. Many people do not maintain records of their requests, which can cause difficulties if follow-ups are needed. Having documentation available ensures that all parties can reference prior correspondence and processes smoothly.
Documents used along the form
When submitting the California Participating Application form, several other documents may be necessary to support your request. Each of these forms plays a crucial role in ensuring that the request for authorization is complete and properly processed. Here is a brief overview of documents that are often used in conjunction with this application:
- Doctor’s First Report of Occupational Injury or Illness (DLSR Form 5021): This form provides initial details about the employee's injury or illness, including the nature of the condition and any initial treatment recommendations. It is essential for establishing the history of the case.
- Treating Physician’s Progress Report (DWC Form PR-2): This report updates the status of the employee’s treatment and recovery, documenting any changes in the condition that may influence the requested treatment plan.
- Utilization Review Request Form: This form is used to initiate the utilization review process, allowing the claims administrator to assess whether the requested treatment is necessary and appropriate based on established guidelines.
- Claim Information Form: Collects important details regarding the worker's compensation claim, often required to process treatment authorizations efficiently and accurately.
- Medical Treatment Utilization Schedule (MTUS): A reference guide used to ensure that requested treatments align with accepted medical standards. Any treatment not in accordance with this schedule may require additional justification.
- Employee Authorization to Release Information Form: Ensures that the employee provides consent for their medical information to be shared with necessary parties involved in the claims process.
- Independent Medical Examination (IME) Report: Should the claims administrator require further assessment, an IME may be conducted, and the report provides objective findings that influence treatment approvals.
- Claim Denial Appeals Form: If a previous treatment request was denied, this form can be used to appeal the decision, providing further evidence and justification for the requested medical services.
- Evidence-Based Practice Guidelines: Documentation that outlines scientifically-supported treatment options for specific conditions, helping validate less common requests that may be outside standard protocols.
Having these documents ready can significantly enhance the likelihood of a smooth approval process. They help medical professionals, claims administrators, and patients navigate the complexities of treatment requests while ensuring that every aspect of the employee’s care is considered.
Similar forms
The California Participating Application form is similar to several other important documents used in healthcare and claims processes. Each of these documents serves to request, authorize, or provide information on medical treatments. Here are seven comparable documents:
- Doctor’s First Report of Occupational Injury or Illness (Form DLSR 5021): This document provides the initial assessment of the employee’s injury, similar to how the Participating Application outlines the necessity for treatment based on the physician’s evaluation.
- Treating Physician’s Progress Report (DWC Form PR-2): Like the California Participating Application, this form updates the claims administrator about the patient's progress, supporting any treatment requests with documentation.
- Request for Authorization for Medical Treatment: This document functions like the California Participating Application by initiating the utilization review process required for treatment approval, ensuring compliance with state regulations.
- Utilization Review Request Form: Similar to the Participating Application, this form is submitted for healthcare services needing approval before the treatment begins, emphasizing the need for timely responses from claims administrators.
- Pre-Authorization Request Form: This form requests approval from insurers for specific medical services or goods, paralleling how the California Participating Application outlines required treatments needing authorization.
- Claim Adjustment Form: This document is used for modifying or appealing decisions regarding prior treatment requests, akin to the resubmission option on the California Participating Application if material facts change.
- Medical Treatment Utilization Schedule (MTUS) Compliance Form: This form ensures that treatment requests align with established medical protocols, just as the California Participating Application necessitates adherence to relevant guidelines for treatment authorization.
Dos and Don'ts
When filling out the California Participating Application form, there are important practices to follow for a smooth process. Here’s a clear list of what you should and shouldn’t do:
- Do carefully complete all sections of the form to avoid delays.
- Do attach necessary medical reports, such as the Doctor’s First Report of Occupational Injury or Illness.
- Do indicate if the request is new or a resubmission due to changed circumstances.
- Do ensure that a signature from the requesting physician is included.
- Don’t leave any required fields blank, as this can cause processing issues.
- Don’t skip the documentation that supports the requested treatment.
- Don’t check multiple boxes if they are not applicable to your situation.
- Don’t forget to verify contact information to ensure proper communication.
Misconceptions
Here are nine common misconceptions about the California Participating Application form (DWC Form RFA) along with explanations to clarify them:
- It is not necessary to attach supporting documents. Many people believe the DWC Form RFA can stand alone. However, you must attach relevant reports, such as the Doctor's First Report of Occupational Injury or Illness, to substantiate your treatment request.
- All treatment requests are automatically expedited. Some individuals assume any request will be given expedited status. In fact, you must check the appropriate box and provide documentation showing an imminent and serious threat to health for expedited review.
- The form is only required for new treatment requests. This misconception suggests that the form is unnecessary for resubmissions. In truth, if material facts change about a previously denied request, you must submit the form again with appropriate documentation.
- The claims administrator has unlimited time to respond. Many people think there is no time limit for responses. However, the claims administrator is obligated to respond within specific timeframes as outlined in Labor Code section 4610.
- The form is separately reimbursable under the Official Medical Fee Schedule. Some believe that submitting the DWC Form RFA entitles them to additional reimbursement. The truth is, this form is not separately reimbursable and should not be submitted for that purpose.
- All medical treatment requests are guaranteed approval. This is not the case. Treatment requests can be denied or modified. The outcome will depend on the justification and supporting evidence provided.
- Only the physician's signature is required. A common misconception is that only the treating physician must sign. However, the claims administrator's agent may also need to sign in certain cases, especially when responding to the request.
- You can submit the form without complete information. Some may assume that it's acceptable to submit an incomplete form. This is inaccurate. It's crucial to fill out all required fields, including diagnoses and codes, for the request to be considered.
- The form can be submitted in any format. Some think they can submit the form in various formats without restrictions. In reality, you should adhere to the specified methods—mail, fax, or email—as indicated by the claims administrator.
Key takeaways
Key Takeaways for Filling Out the California Participating Application Form
- The Request for Authorization (DWC Form RFA) is essential for starting the utilization review process mandated by California labor laws.
- Always attach required documents like the Doctor’s First Report of Occupational Injury or Illness or other supporting reports when submitting the form.
- Clearly indicate whether the request is a new submission or a resubmission based on changing facts related to the employee's condition.
- Expedited review requests require strict documentation to prove there is an imminent health threat to the employee.
- All sections of the form must be filled out completely, including detailed information about the requested treatment and associated codes.
- Signatures from the requesting physician are mandatory; this section cannot be overlooked.
- The claims administrator has specific timelines to respond to the authorization request as outlined in state regulations.
- Additional treatments must be clearly listed, especially if the provided space is insufficient; extra sheets can be attached as necessary.
Browse Other Templates
Return Authorization - Please provide your contact information, including name and email address.
Clark Atl - Counselors can provide additional comments to offer further insight into the student’s abilities and personality.