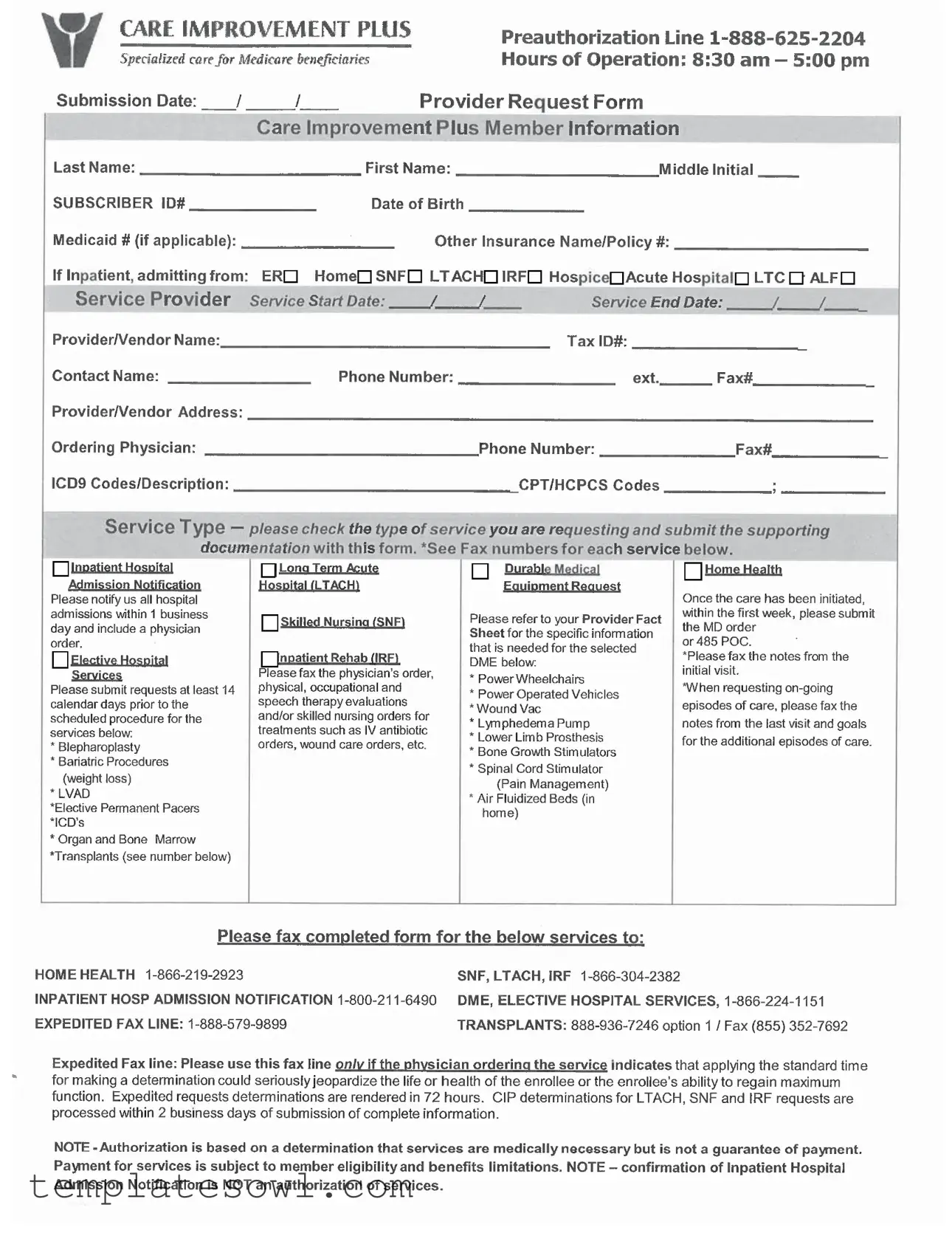
Fill Out Your Care Improvement Plus Authorization Form
The Care Improvement Plus Authorization form plays a crucial role in managing specialized care for Medicare beneficiaries. This form is essential for health care providers seeking preauthorization for various services, including inpatient admissions, outpatient procedures, and durable medical equipment. It requires specific member information, such as the subscriber ID, date of birth, and details about any other insurance coverage. Each service type, whether it’s skilled nursing, long-term acute care, or durable medical equipment, demands accompanying documentation to ensure a smooth review process. Providers are reminded to notify Care Improvement Plus of hospital admissions within one business day and to submit requests for elective services at least 14 days in advance. The form outlines crucial communication details, including fax numbers for different service requests and the hours of operation for preauthorization inquiries. Importantly, while the authorization indicates medical necessity, it does not guarantee payment, as reimbursement is dependent on the member's eligibility and specific benefit limitations. Understanding this form's requirements can facilitate efficient care coordination and ensure beneficiaries receive the necessary services promptly.
Care Improvement Plus Authorization Example
Form Characteristics
| Fact Name | Fact Description |
|---|---|
| Purpose | The Care Improvement Plus Authorization form is designed for Medicare beneficiaries to obtain preauthorization for specialized medical services. |
| Preauthorization Line | A dedicated preauthorization line is available at 1-888-625-2204, operating from 8:30 AM to 5:00 PM. |
| Submission Date | Healthcare providers must include the submission date on the form to ensure timely processing of requests. |
| Service Provider Details | Providers must fill in their name, tax ID, address, contact details, and service start and end dates for their requests. |
| Service Types | Request forms should indicate the type of service being requested, such as inpatient care or durable medical equipment. |
| Standard Fax Lines | Different services have specific fax lines for submission, ensuring proper tracking and processing. |
| Expedited Requests | Requests involving urgent health situations can be processed within 72 hours via an expedited fax line. |
| Authorization Limitations | Authorization signifies that services are deemed medically necessary, but does not guarantee payment. Eligibility will still be verified. |
| Inpatient Notification | Notification of inpatient admissions must occur within one business day, accompanied by a physician's order. |
| Governing Laws | This authorization process is governed by various state laws addressing Medicare service provisions and patient care standards. |
Guidelines on Utilizing Care Improvement Plus Authorization
Filling out the Care Improvement Plus Authorization form involves several steps. By completing this form, you are initiating a process that allows healthcare providers to get approval for necessary services. Make sure to provide accurate information to avoid delays in receiving care. Here’s how to complete the form effectively:
- Gather Required Information: Before you start, collect all necessary information such as patient identification, provider details, and service specifications.
- Fill Out Member Information: Enter the patient's last name, first name, middle initial, subscriber ID number, date of birth, and Medicaid number if applicable. Include other insurance name and policy number as needed.
- Detail the Service Provider: Provide the service provider's name, tax ID number, contact name, address, phone number, and fax number.
- Include Provider Details: Write down the ordering physician’s name, phone number, and fax number.
- Specify Service Start and End Dates: Clearly indicate the dates for when the service will begin and end.
- List Relevant Codes: Fill in the ICD9 codes with their descriptions, as well as the CPT/HCPCS codes related to the requested service.
- Select Service Type: Check the appropriate service type you are requesting—this could range from inpatient admissions to durable medical equipment.
- Submit Supporting Documentation: Make sure to include any additional documentation required for the service you’re requesting, like physician orders or therapy evaluations.
- Fax the Completed Form: Send the completed form along with the necessary documentation to the appropriate fax number provided for the service you are seeking.
Once you have submitted the form, the healthcare provider will review it to ensure that the requested services are medically necessary. It’s essential to keep track of the submission for any follow-ups you may need to make. Be aware that authorization does not guarantee payment, as eligibility and benefits will also be assessed.
What You Should Know About This Form
What is the purpose of the Care Improvement Plus Authorization form?
The Care Improvement Plus Authorization form is designed to facilitate the preauthorization process for specialized care services for Medicare beneficiaries. It helps ensure that providers obtain necessary approvals before rendering specific medical services, thus improving coordination of care and minimizing delays in treatment.
What information is needed to complete the authorization form?
To complete the authorization form, providers must provide detailed information including the member's last name, subscriber ID, date of birth, and any applicable Medicaid or other insurance information. Additionally, service provider details, service start and end dates, contact information, and specific procedure codes are required to accurately process the request.
How can providers submit the Care Improvement Plus Authorization form?
Providers can submit the form via fax to the appropriate fax number designated for the type of service being requested. This includes separate fax lines for home health, inpatient services, durable medical equipment, and elective hospital services. It is important to follow the guidelines and include all supporting documentation to expedite the review process.
What happens if the request is urgent?
If a request requires urgent attention, the expedited fax line should be used. This option is available when there is a concern that adhering to standard timelines could jeopardize the patient's health or recovery. Expedite requests are processed within 72 hours, ensuring timely access to necessary medical services.
Can authorization guarantee payment for services?
Authorization obtained through the Care Improvement Plus form does not guarantee payment. While it verifies that the services are medically necessary, payment is contingent upon the member's eligibility and benefit limitations. Providers should verify coverage directly with the member's insurance policy prior to delivering services.
What should be done in the case of hospital admissions?
For inpatient hospital admissions, providers must notify Care Improvement Plus within one business day. It is necessary to include a physician order for the admission. However, it’s important to note that confirmation of notification does not constitute an authorization for payment of services rendered during the inpatient stay.
Common mistakes
Filling out the Care Improvement Plus Authorization form can be a daunting task, especially for those unfamiliar with the requirements. Mistakes made during this process can lead to delays, denials, or complications in receiving necessary care. Here are ten common mistakes to avoid when completing this important form.
One frequent error is the omission of the subscriber ID number. This number is crucial for identifying the beneficiary's record and ensuring that the request is processed correctly. Without it, the form may be returned or delayed.
Another mistake occurs with the incomplete member information. It’s vital to provide the full name, including the last name, first name, and middle initial, along with the date of birth and any applicable Medicaid number. Inaccuracies in this section can lead to unnecessary follow-up communication and potential disruptions in care.
Many people also overlook the service start and end dates. Not specifying these dates can cause confusion regarding the duration of the requested services. This detail is particularly important for approval processes, as it informs the provider and insurer about the timeline for the requested care.
Additionally, the section for ICD9 and CPT/HCPCS codes is often filled incorrectly. These codes categorize the medical necessity of the services requested. Inaccurate coding can impact authorization and reimbursement, leading to possible denials of claims down the line.
An overlooked section is checking the type of service requested. Without this, the processing team might not have clear direction on how to categorize the request. Failing to check a box could mean that essential documentation is lost or misdirected.
Not including supporting documentation is another frequent pitfall. This documentation provides context for the request and validates the medical necessity of the services. Submitting the form without these crucial papers can lead to instant rejection.
Incorrectly filling out the provider/vendor information is another common error. Ensure that the tax identification number, phone number, and address of the service provider are accurate. Payment and communication rely heavily on this information being correct.
Some individuals fail to inform the insurance provider within the required time frame regarding hospital admissions. A notification must occur within one business day to avoid complications in receiving care and authorization. Delays in this could result in higher costs or payment denials.
Another mistake is using the wrong fax number for submissions. Each service type has specific designated fax numbers. Submitting to the incorrect number can lead to unnecessary delays in processing, potentially compromising the timing of care.
Finally, it is essential to understand the distinction between an authorization of services and the determination of medical necessity. Many people think that completing this form guarantees payment, while in fact, it is subject to eligibility and limitations set by the insurance plan.
Being aware of these common mistakes can transform the process of completing the Care Improvement Plus Authorization form from a burden into a smoother experience. Careful attention to detail will not only expedite the processing of requests but will also ensure that beneficiaries receive the essential care they need without unnecessary hitches.
Documents used along the form
The Care Improvement Plus Authorization form is an essential document for Medicare beneficiaries seeking specialized care. However, this form is usually accompanied by other important documentation that helps streamline the authorization process. Here are a few commonly used forms that complement the Care Improvement Plus Authorization form.
- Provider Request Form: This form collects detailed information from the healthcare provider about the services being requested. It includes patient information, diagnosis codes, and specifics about the requested procedures, ensuring that the care team has everything needed to make an informed decision.
- Physician’s Order: This document outlines the specific services or treatments that a physician recommends for a patient. It's often required to support the authorization request and helps validate the medical necessity of the requested services.
- Progress Notes: After care has commenced, these notes provide a record of the patient's ongoing treatment and recovery. They often need to be submitted for ongoing episodes of care, allowing payers to assess the continuity and effectiveness of the treatment.
- Plan of Care (POC) or 485 Form: This form details the patient's care plan, including all prescribed services and goals for their treatment. It serves as a guide for home health services and is often required shortly after care initiation to ensure proper oversight by the insurance provider.
Each of these forms plays a crucial role in the authorization process for health services. Having them ready and correctly filled out can significantly expedite approval and ensure that patients receive the care they need without unnecessary delays.
Similar forms
Prior Authorization Form: Similar to the Care Improvement Plus Authorization form, this document requires prior approval for specific medical services. It ensures the service is medically necessary before the provider can proceed.
Insurance Claim Form: This form helps to document and report the services provided and the associated costs. Like the Care Improvement Plus Authorization form, it plays a crucial role in obtaining reimbursement from insurers.
Referral Form: A referral form is needed when a primary care physician sends a patient to a specialist. This is similar to the Care Improvement Plus Authorization form in that it initiates the approval process for specialized care.
Medication Authorization Request: Much like the Care Improvement Plus Authorization form, this document seeks approval for specific medications before they can be dispensed, ensuring the medication is necessary and covered.
Home Health Service Authorization: This document is crucial for initiating home health services. It shares similarities with the Care Improvement Plus Authorization as it outlines the need for additional services, ensuring proper care is provided.
Durable Medical Equipment (DME) Authorization Form: Similar in purpose, this form requests approval for durable medical equipment. It helps confirm that such devices are medically necessary and meets the patient’s needs.
Emergency Services Notification: This form is for notifying insurers about emergency services provided. Like the Care Improvement Plus Authorization form, it ensures that the provided services are logged and potentially eligible for coverage.
Dos and Don'ts
When filling out the Care Improvement Plus Authorization form, attention to detail is crucial. Here’s a guide on what to do and what to avoid:
- Do provide complete and accurate member information, including full name, subscriber ID, and date of birth.
- Do double-check the service start and end dates to ensure they are accurate.
- Do submit the request at least 14 calendar days before scheduled elective hospital services.
- Do include all necessary supporting documentation, such as physician orders and therapy evaluations.
- Do use the correct fax numbers provided for the specific service type requested.
- Don't leave any required fields blank on the form.
- Don't assume that providing the authorization form guarantees payment; check eligibility and benefits.
- Don't forget to follow up on submitted requests to confirm receipt and status.
- Don't neglect to inform of any inpatient admissions within the required one business day.
By following these guidelines, you enhance the chance of a smooth authorization process.
Misconceptions
Understanding the Care Improvement Plus Authorization form is crucial for both healthcare providers and patients. Here are nine common misconceptions about this form:
- Authorization guarantees payment for services. Many believe that obtaining authorization means their services will be paid for. In reality, authorization only indicates that the service is deemed medically necessary. Payment still depends on member eligibility and benefits.
- All services require the same submission process. Different types of services, like elective procedures or durable medical equipment, require unique documentation and submission procedures. It's important to know the specific requirements for each service.
- You can notify us of admissions at any time. There is a strict requirement to notify within one business day for inpatient hospital admissions. Delaying notification could lead to complications in the authorization process.
- Expedited requests are for all cases. While expedited requests are available, they should only be used when the patient's life or health is at serious risk. Not every situation qualifies for expedited processing.
- Once submitted, no further documentation is needed. This is not true. For ongoing episodes of care or additional services, further documentation such as physician orders and therapy evaluations is often required.
- Any physician can order services without limitations. Services must be ordered by a physician who is part of the Care Improvement Plus network. Using a non-network physician could hinder the authorization process.
- You can fill out the form at your convenience. The submission date is critical, especially for elective services which require requests to be submitted at least 14 days in advance. Deadlines are non-negotiable.
- The form is the only requirement for authorization. Supporting documents must accompany the form. This may include detailed clinical notes or specific evaluations to support the necessity of the requested service.
- Once authorized, changes can be made easily. Changes to authorized services may require a new authorization request. It’s essential to communicate any modifications as soon as possible to avoid service delays.
By clearing up these misconceptions, healthcare providers and patients can better navigate the Care Improvement Plus authorization process and ensure smoother service delivery.
Key takeaways
Filling out the Care Improvement Plus Authorization form accurately is crucial. Make sure to include all requested information like the member's full name, subscriber ID, and date of birth.
Always submit the form with supporting documents. For inpatient services, include a physician's order, and for home health requests, provide the notes from the initial visit.
Use the correct fax numbers provided for different service types. Each category has a specific fax line that needs to be used for timely processing.
Remember that approval of services depends on medical necessity but does not guarantee payment. Make sure to verify member eligibility and benefit limitations.
Browse Other Templates
Addendums - It includes essential clauses about appraised values, providing security for the Buyer regarding their investment.
Certificate of Conformance - The authorized certifying official must be clearly identified on the certificate.
Broker Partnership Application,Mortgage Broker Network Enrollment,UWM Affiliate Registration,Wholesale Mortgage Broker Signup,UWM Collaboration Form,Broker Integration Application,Wholesale Lending Partnership Form,Mortgage Broker Support Document,UW - List all employees and sales contacts in your submission.