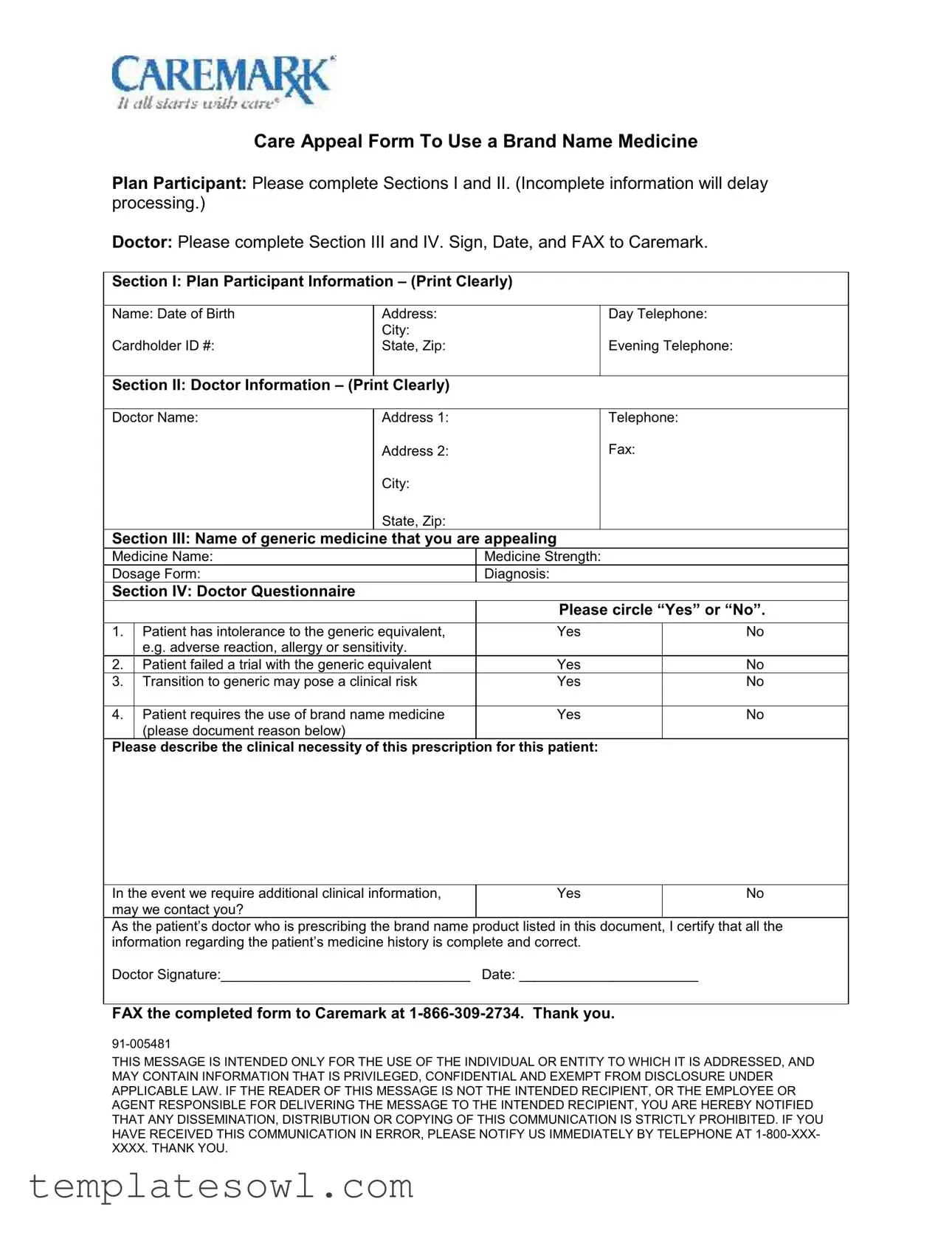
Fill Out Your Caremark Appeal Form
The Caremark Appeal form serves as a vital tool for individuals seeking to contest decisions made by Caremark regarding their prescription drug benefits. This form outlines necessary information for submission, including personal identification, details of the disputed claim, and the reason for the appeal. It is imperative that individuals provide accurate and complete data to facilitate a comprehensive review of their situation. Furthermore, specific documentation may be required to support the appeal, ensuring that all relevant medical information and previous correspondence are included. Timeliness is essential; appeals must be submitted within a designated timeframe following the receipt of the initial determination. As individuals complete this form, they must be aware of the potential for different outcomes, including possible approvals or denials, both of which can greatly impact their access to medications. Understanding the nuances of the Caremark Appeal process can enhance the effectiveness of the appeal and provide individuals with a better chance of achieving a favorable resolution.
Caremark Appeal Example
!" #$%& ' #'($)"!)*+)#$%& '
!" #$%& ' #'($)!)*(0)!' !)*'$!-
|
|
|
|
|
|
|
|
|
|
|
!% 3!' |
|
|
**- ""3 |
|
|
|
!/ &4$) 3 |
|
||
|
|
|
('/3 |
|
|
|
|
|||
|
|
'!' 6(&3 |
|
|
|
7 )()0 &4$) 3 |
|
|||
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
**- ""3 |
|
|
|
&4$) 3 |
|
|||
|
|
|
|
|
|
|
||||
|
|
|
**- ""83 |
|
|
|
!93 |
|
||
|
|
|
|
|
|
|
||||
|
|
|
('/3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
'!' 6(&3 |
|
|
|
|
|
|
!"#! |
|
|
|
|
||||||
*(#() !% 3 |
|
|
|
|
*(#() '- )0'43 |
|
||||
$"!0 |
|
|
|
|
(!0)$"("3 |
|
|
|
|
|
$%# |
|
|
|
|
|
|
|
|||
|
|
|
|
|
&'(&() |
|||||
!'( )'4!"()'$ |
:;(7! )' |
|
" |
|
$ |
|||||
|
0!*7 |
|
|
|
|
|
|
|||
8 |
!'( )',!( |
) |
|
" |
|
$ |
||||
< |
|
" |
|
$ |
||||||
|
|
|
|
|
|
|
|
|
|
|
= |
!'( |
% *(#() |
|
" |
|
$ |
||||
|
+& !" *$#;% )'- !"$)> $.1 |
|
|
|
|
|
|
|
||
*""" |
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
)'4 7 )'. |
|
" |
|
$ |
||||||
%!/. #$)'!#'/$;? |
|
|
|
|
|
|
|
|
|
|
"'4 &!'( |
||||||||||
#' |
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
BC=
Form Characteristics
| Fact Name | Detail |
|---|---|
| Form Purpose | The Caremark Appeal form is used to request a review of benefits denials. |
| Eligibility Criteria | Individuals must be enrolled in a Caremark plan to submit an appeal. |
| Governing Law | In many states, the appeal process is governed by the Employee Retirement Income Security Act (ERISA). |
| Submission Deadline | Appeals must typically be submitted within 180 days from the date of the denial notice. |
| Contact Information | For questions regarding the form or the appeal process, individuals can reach Caremark's customer service. |
Guidelines on Utilizing Caremark Appeal
Before starting the process, ensure you have all necessary documents and information on hand. This will help streamline the completion of the Caremark Appeal form. Carefully follow the steps outlined below to complete the form accurately.
- Begin by downloading the Caremark Appeal form from the official website.
- Review the entire form to understand the sections that need to be filled out.
- Fill in your personal information, including your full name, address, and contact details at the top of the form.
- Provide your Caremark member ID number. This can usually be found on your membership card.
- Enter the date of the original decision on the relevant line.
- Clearly state the reason for your appeal in the designated section. Be concise and specific.
- Attach any necessary supporting documents that reinforce your appeal.
- Review the completed form for any errors or omissions. Ensure all sections are filled out properly.
- Sign the form at the bottom to certify that all information provided is accurate.
- Make a copy of the completed form and all attachments for your records.
- Mail the form to the address specified on the document. Make sure to send it via a method that allows for tracking.
After submitting the form, you will receive confirmation of receipt from Caremark. Be prepared to wait for their response regarding the appeal decision. Checking back periodically can help ensure you stay updated on the status of your appeal.
What You Should Know About This Form
What is the purpose of the Caremark Appeal form?
The Caremark Appeal form allows individuals to request a review of a decision made regarding prescription drug coverage. This could include denials for coverage, exclusions, or limitations imposed by the insurance plan. Completing this form initiates the appeal process, ensuring that your concerns are formally considered.
Who should complete the Caremark Appeal form?
The form should be completed by the member whose prescription coverage is being appealed. If the member prefers, a designated representative, such as a family member or healthcare provider, can also complete the form on their behalf. Ensure all relevant information is provided for a smooth review process.
What information is required to fill out the Caremark Appeal form?
You will need to provide personal details, including your name, address, and member ID. Additionally, it’s essential to include specific information about the medication in question, such as the name, dosage, and any relevant prior authorization numbers. Supporting documents, like medical records or letters from healthcare providers, may also be helpful.
How long does it take to process a Caremark Appeal?
The processing time for an appeal can vary. Generally, you can expect to receive a decision within 30 days if it is a standard appeal. If you request an expedited review, which may be needed in urgent cases, you could receive a decision in as little as 72 hours. Be sure to follow up if you do not receive communication within the expected timeframe.
What happens if the appeal is denied?
If your appeal is denied, you will receive a written notification detailing the reasons for the denial. This letter should explain how you can request a further review or pursue additional avenues for appeal. It's important to review the reasons carefully and consider any new evidence or documentation you can provide for a subsequent appeal.
Can I appeal a decision more than once?
Yes, you can appeal a decision multiple times. Each appeal requires the submission of the Caremark Appeal form along with any new information or evidence to support your case. Keep in mind that following the proper channels and deadlines for each appeal is critical to having your request considered.
Common mistakes
Filling out the Caremark Appeal form can be a straightforward process—if done correctly. However, many individuals make common mistakes that can lead to confusion and delays in processing their appeals. Here are ten of those mistakes to avoid.
One major mistake is not reading the instructions carefully. Each section of the form has specific guidelines that must be followed for the appeal to be valid. Ignoring these instructions may lead to incomplete information and potential rejection of the appeal.
Another frequent error is providing insufficient documentation. While individuals may think their explanation is enough, it’s crucial to include all relevant medical records, invoices, and any supportive statements from healthcare providers. Documentation can be the deciding factor in whether an appeal is approved or denied.
Many people fail to check the deadlines. Appeals typically have strict timelines. Missing a deadline can mean losing the right to appeal entirely. Keeping a careful eye on these dates is essential to ensure the appeal is submitted on time.
Providing inaccurate or outdated personal information is another common mistake. This can include misspelled names, incorrect addresses, or wrong policy numbers. Double-checking this information can prevent unnecessary complications down the line.
Individuals often neglect to sign the form. An unsigned form can be considered invalid. It’s a simple yet serious oversight that can jeopardize an otherwise well-prepared appeal.
Some people underestimate the importance of clarity in their explanations. When stating the reason for the appeal, being vague may lead to misunderstandings. Using clear and concise language is vital for the reviewers to grasp the specific points of the case.
Failing to follow the required format is also a common issue. Whether it’s font size, spacing, or using the correct form version, these details matter. Not adhering to the format can result in the appeal being disregarded or delayed.
Many forget to keep copies of everything submitted. Having a personal record can be a lifesaver if anything goes wrong or if follow-up information is needed later. It helps track the progress of the appeal and reference the original submission.
Overlooking support from others can hinder an appeal. Seeking help from a lawyer or a knowledgeable individual can provide guidance and reinforce arguments. Understanding the process can significantly improve the chances of a successful appeal.
Lastly, impatience can lead to frustration. After submitting an appeal, some people expect immediate results. It’s important to remember that reviews take time. Being patient and checking in at appropriate intervals can ease anxiety while waiting for a response.
By avoiding these ten mistakes, individuals can improve their experience with the Caremark Appeal process. Being thorough and attentive can make a significant difference in achieving a favorable outcome.
Documents used along the form
When submitting a Caremark Appeal form, there are several other documents that may often accompany it. These documents can help strengthen your case and provide essential information to the reviewers. Below is a list of these common forms and documents.
- Explanation of Benefits (EOB): This document outlines the benefits provided by your insurance plan for the specific service or prescription in question. It details what was covered and what the patient's financial responsibility is.
- Doctor's Letter of Medical Necessity: This letter is written by your healthcare provider explaining why a particular treatment, medication, or procedure is necessary for your health. It serves to clarify the medical reasons behind the appeal.
- Prior Authorization Request: If the prescription needed prior approval, this document shows that a request was submitted. It may include the details of the initial appeal process and any communications with the insurance provider.
- Supporting Medical Records: These records include relevant test results, diagnoses, and treatment histories that support your case. They provide essential context for the appeal and validate the need for the requested services.
- Appeal Letter: This is a formal letter that outlines your reasons for the appeal in a clear and concise manner. It explains why the original claim should be overturned and emphasizes essential information contained in the accompanying documents.
Including these documents with your Caremark Appeal can enhance your submission and provide a clearer picture to those reviewing your appeal. Always ensure that all paperwork is complete and accurate to improve the chances of a positive outcome.
Similar forms
- Claim Denial Letter: Like the Caremark Appeal form, a Claim Denial Letter explains why a claim was denied. It provides detailed information on the reasons for the denial and outlines the next steps the claimant can take.
- Grievance Form: The Grievance Form is similar because it allows individuals to voice their dissatisfaction about a service or decision. Both documents serve as pathways for addressing grievances within a healthcare system.
- Prior Authorization Request: This document is used to request approval for a specific treatment or medication before it is provided. The Caremark Appeal form also seeks to obtain approval, focusing on reversing a prior denial.
- Pharmacy Benefit Claim Form: Both forms are used in the context of healthcare benefits and claims. While the Pharmacy Benefit Claim Form is used to submit a claim for medication, the Caremark Appeal form challenges denied benefits related to pharmacy claims.
- Insurance Appeal Form: The Insurance Appeal Form enables policyholders to contest decisions made by their insurance providers. Much like the Caremark Appeal form, it outlines the basis for the appeal and requests reconsideration of a determination.
Dos and Don'ts
When filling out the Caremark Appeal form, consider these important do's and don'ts to ensure your submission is complete and clear.
- Do read the instructions carefully before starting.
- Do provide all requested information accurately.
- Do double-check your contact details to avoid delays in communication.
- Don't leave any sections blank; incomplete forms can lead to rejection.
- Don't use abbreviations or jargon that may confuse the reviewer.
- Don't submit the form without a final review; errors can complicate the appeal process.
Misconceptions
Here are ten common misconceptions about the Caremark Appeal form, along with clear explanations for each:
- The Caremark Appeal form is only for denied claims. Many believe this form is exclusively for denied claims, but it can also be used for issues such as delays or misunderstandings related to the claims process.
- Filling out the form guarantees approval. This misconception assumes that submitting the form will automatically result in a favorable outcome. However, the decision ultimately depends on the evidence and circumstances of each individual case.
- You need a lawyer to file an appeal. Some think that legal representation is required to complete the Caremark Appeal form. This is not true; individuals can fill out the form themselves.
- All appeals must be done in writing. While most appeals do require written documentation, certain situations allow for verbal appeals. It’s important to check specifically for options available to you.
- I can appeal any decision. Many individuals believe they can appeal any decision made by Caremark. However, there are specific guidelines and timelines for filing appeals that must be followed.
- The process is the same for all insurance companies. This misconception suggests that all appeals processes are uniform. In reality, each insurance company may have its own rules and procedures that need to be followed.
- You must have a valid reason to appeal. While a valid reason strengthens your case, you can still appeal based on procedural issues or lack of communication, even if the original reason was technically sound.
- The form must be submitted immediately. Many believe that appeals must be filed immediately after a claim denial. There is often a set timeframe that varies by insurer; knowing your deadlines is crucial.
- You can’t appeal if your claim was partially paid. Some think that if a claim has been partially paid, they cannot appeal it. However, if you disagree with the amount paid, you can still file an appeal.
- Once submitted, you cannot change the appeal. It’s commonly thought that appeals are final once submitted. In fact, there’s often an opportunity to amend or add to your appeal if new information arises.
Understanding these misconceptions can help make the process of appealing a decision smoother and more efficient.
Key takeaways
Filling out the Caremark Appeal form can seem daunting, but with the right approach, you can navigate it successfully. Here are some key takeaways to keep in mind:
- Understand the Purpose: The appeal form is your opportunity to challenge a decision that may have impacted your coverage or access to medication. Knowing why you’re appealing is crucial.
- Complete Information: Provide all required details accurately. Missing information can delay the process or even result in a denied appeal.
- Be Clear and Concise: State your case clearly. Use straightforward language to explain your reasons for the appeal. This helps the reviewer understand your perspective more readily.
- Follow Up: After submitting the appeal, don’t forget to follow up. This ensures your appeal is being processed and that you can address any issues promptly.
By keeping these points in mind, you can increase your chances of a successful outcome with your Caremark Appeal form.
Browse Other Templates
California Court - Written authority must be clear for parties representing themselves.
Smith Warranty Claim - Verify that the sunglasses or goggles are the right model before returning.