Fill Out Your Case Conceptualization Form
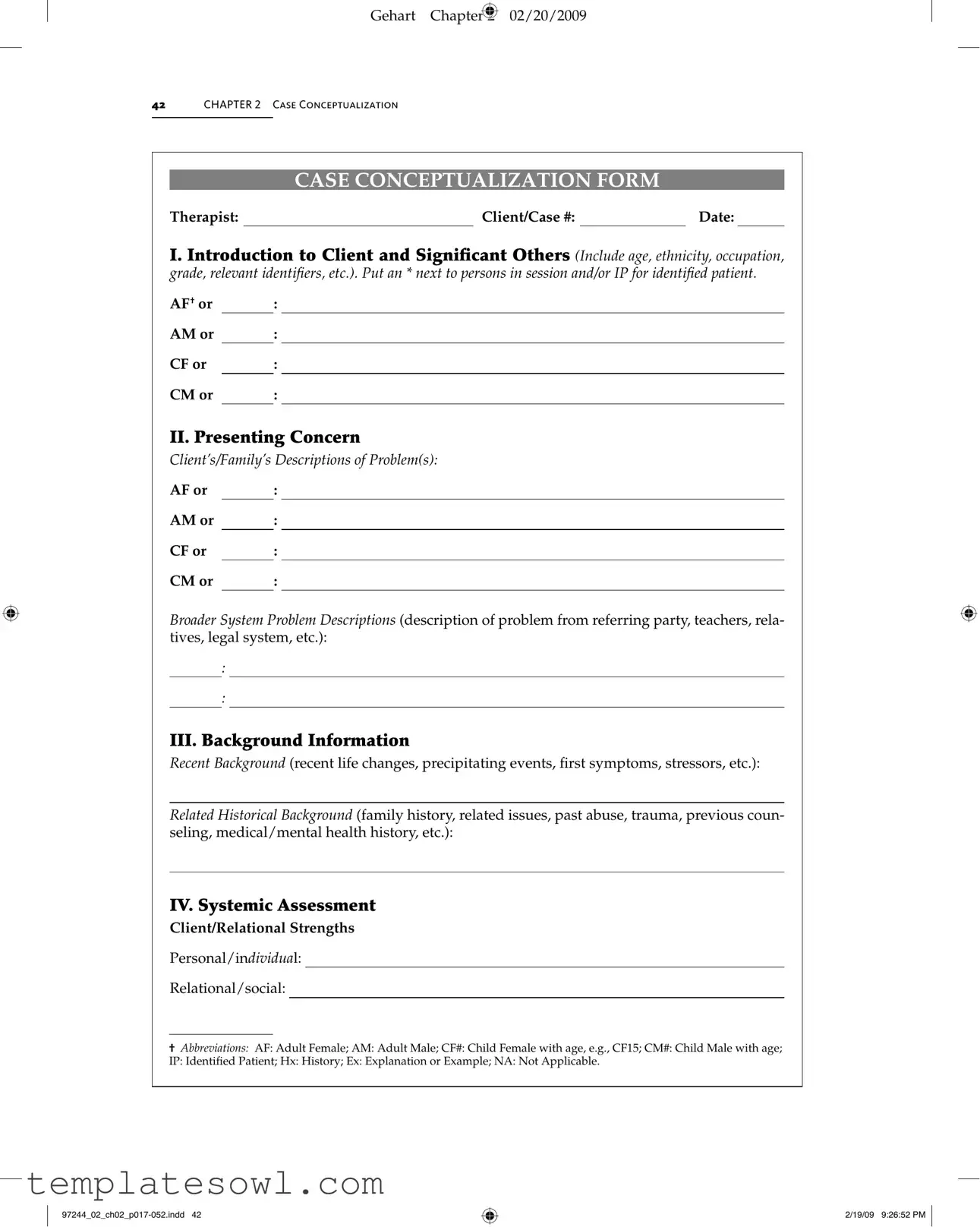
The Case Conceptualization form serves as a structured tool for therapists to gather and organize essential information about clients and their significant others. It begins with an introduction to the client, including demographic details such as age, ethnicity, and occupation, as well as identifiers for individuals present during sessions. The second section focuses on the presenting concerns from both the clients and their broader social systems, providing a comprehensive view of the issues at play. Subsequently, the form gathers background information on recent and historical life events that may influence the client's situation. An in-depth systemic assessment follows, where the therapist evaluates relational strengths and family dynamics, including communication patterns and interaction styles. This assessment extends to considering the broader family life cycle stages and the hierarchy between adults and children within the family. The form also encourages the exploration of intergenerational patterns and historical incidents that could inform the current dynamics. Lastly, it prompts the therapist to assess client perspectives on the identified problems and areas of disagreement, serving as a guide for facilitating respectful dialogue. By documenting these various aspects, the Case Conceptualization form enables a multi-faceted understanding of the client’s situation, which can lead to more effective interventions.
Case Conceptualization Example

Gehart Chapter 2 02/20/2009
42CHAPTER 2 Case Conceptualization
CASE CONCEPTUALIZATION FORM
Therapist: |
|
Client/Case #: |
|
Date: |
I. Introduction to Client and Signiicant Others (Include age, ethnicity, occupation, grade, relevant identii ers, etc.). Put an * next to persons in session and/or IP for identiied patient.
AF† or |
|
: |
AM or |
|
: |
CF or |
|
: |
CM or |
|
: |
II. Presenting Concern
Clients/Familys Descriptions of Problem(s):
AF or |
|
: |
AM or |
|
: |
CF or |
|
: |
CM or |
|
: |
Broader System Problem Descriptions (description of problem from referring party, teachers, rela- tives, legal system, etc.):
:
:
III. Background Information
Recent Background (recent life changes, precipitating events, irst symptoms, stressors, etc.):
Related Historical Background (family history, related issues, past abuse, trauma, previous coun- seling, medical/mental health history, etc.):
IV. Systemic Assessment
Client/Relational Strengths
Personal/individual:
Relational/social:
†Abbreviations: AF: Adult Female; AM: Adult Male; CF#: Child Female with age, e.g., CF15; CM#: Child Male with age; IP: Identiied Patient; Hx: History; Ex: Explanation or Example; NA: Not Applicable.
2/19/09 9:26:52 PM
Gehart Chapter 2 02/20/2009
Case Conceptualization Form |
43 |
|
|
|
|
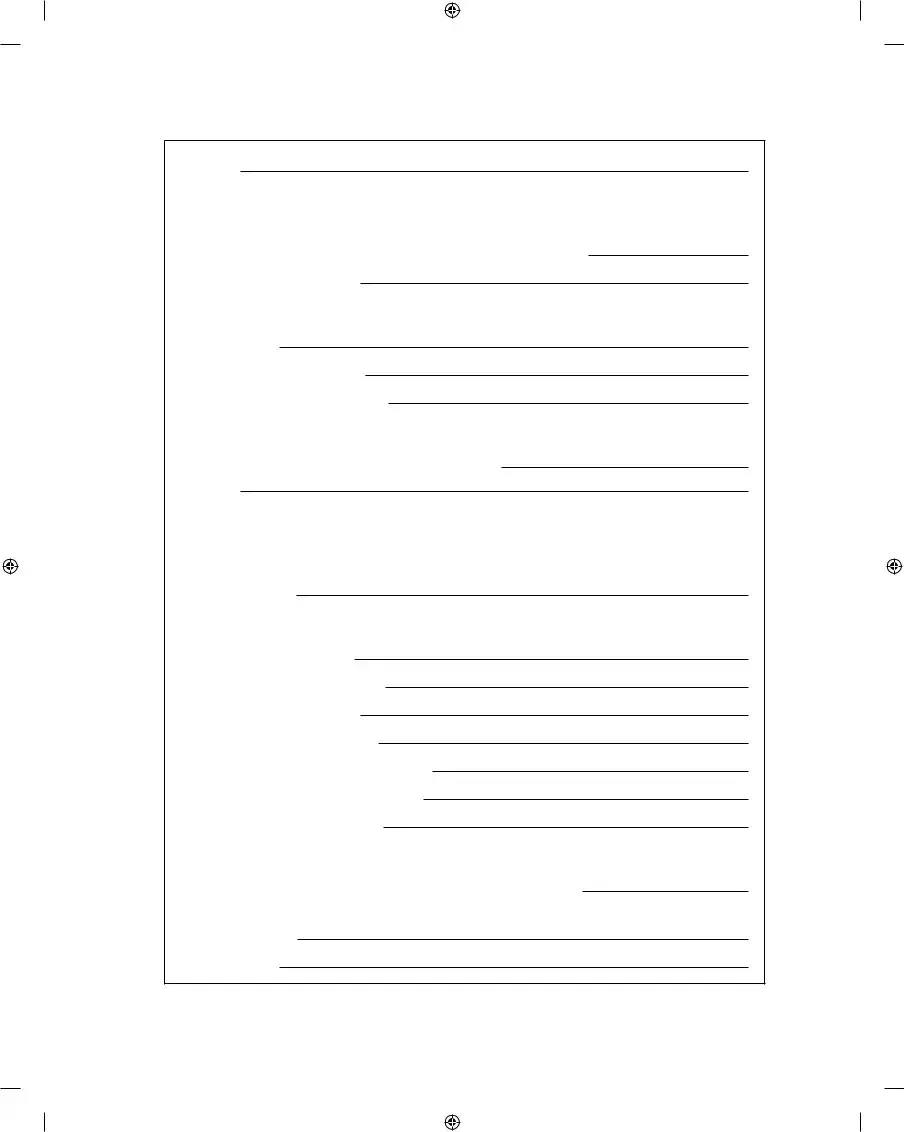
Spiritual:
Family Structure and Interaction Patterns
Couple Subsystem (to be assessed): □ Personal current □ Personal past □ Parents
Couple Boundaries: □ Clear □ Enmeshed □ Disengaged □ Other:
Rules for closeness/distance:
Couple Problem Interaction Pattern (A ⇄ B):
Start of tension:
Conlict/symptom escalation:
Return to “normal”/homeostasis:
Couple Complementary Patterns: □ Pursuer/distancer □ Over/under functioner
□Emotional/logical □ Good/bad parent □ Other: Describe:
Satirs Communication Stances:
AF: □ Congruent □ Placator □ Blamer □ Superreasonable □ Irrelevant
AM: □ Congruent □ Placator □ Blamer □ Superreasonable □ Irrelevant Describe dynamic:
Gottmans Divorce Indicators:
Criticism: □ AF □ AM Ex:
Defensiveness: □ AF □ AM Ex:
Contempt: □ AF □ AM Ex:
Stonewalling: □ AF □ AM Ex:
Failed repair attempts: □ AF □ AM Ex:
Not accept inluence: □ AF □ AM Ex:
Harsh startup: □ AF □ AM Ex:
Parental Subsystem: □ Family of procreation □ Family of origin
Membership in Family Subsystems: Parental: □ AF □ AM □ Other:
Is parental subsystem distinct from couple subsystem? □ Yes □ No □ NA (divorce) Sibling subsystem:
Special interest:
(continued)
2/19/09 9:26:52 PM
Gehart Chapter 2 02/20/2009
44CHAPTER 2 Case Conceptualization
(continued)
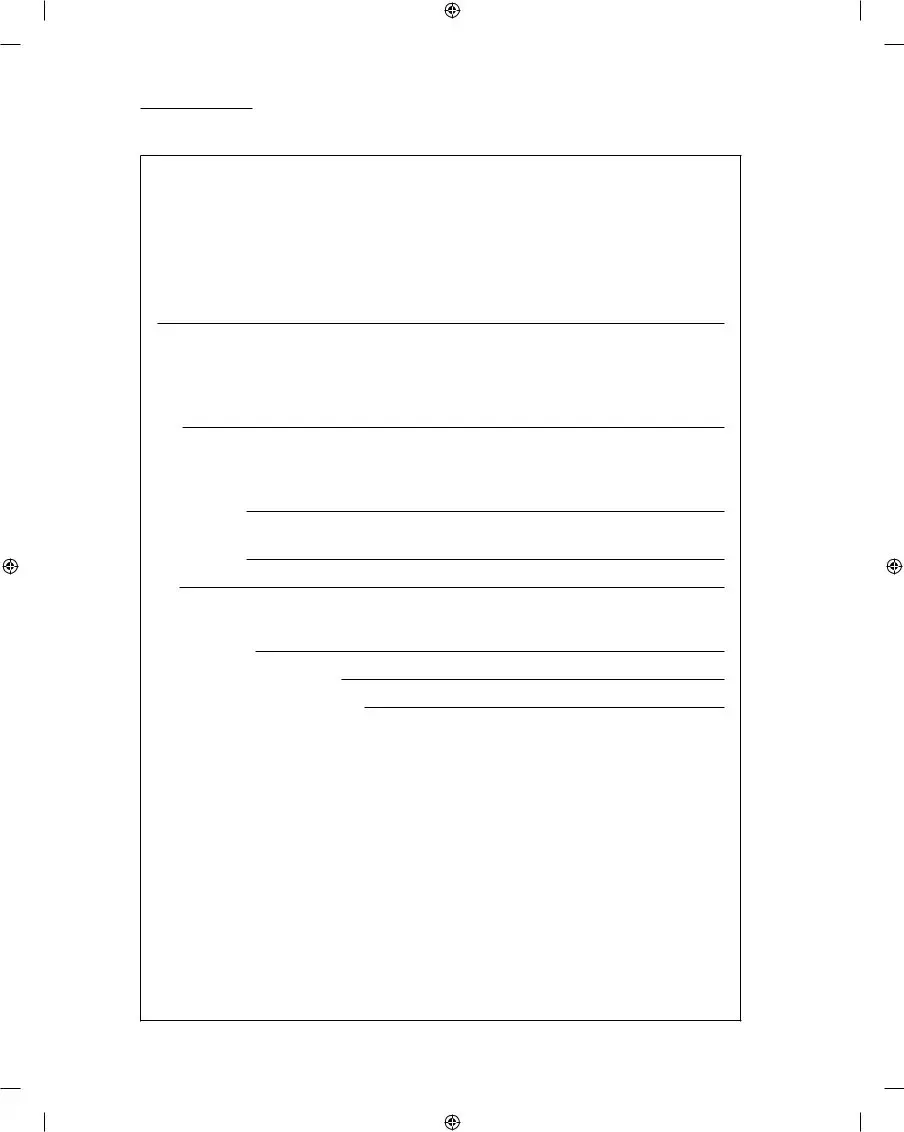
IV. Systemic Assessment
Family Structure and Interaction Patterns
Family Life Cycle Stage:
□Single adult □ Marriage □ Family with young children
□Family with adolescent children □ Launching children □ Later life Describe struggles with mastering developmental tasks in one of these stages:
Hierarchy Between Child/Parents:
AF: □ Effective □ Insuficient (permissive) □ Excessive (authoritarian) □ Inconsistent
AM: □ Effective □ Insuficient (permissive) □ Excessive (authoritarian) □ Inconsistent
Ex:
Emotional Boundaries with Children:
AF: □ Clear/balanced □ Enmeshed (reactive) □ Disengaged (disinterested)
□Other:
AM: □ Clear/balanced □ Enmeshed (reactive) □ Disengaged (disinterested)
□Other:
Ex:
Problem Interaction Pattern (A ⇄ B):
Start of tension:
Conlict/symptom escalation:
Return to “normal”/homeostasis:
Triangles/Coalitions: |
|
|
|
|
□ AF and C |
|
against AM: Ex: |
|
|
□ AM and C |
|
against AF: Ex: |
|
|
□ Other: Ex: |
|
|
|
|
Communication Stances:
AF or |
|
|
: □ Congruent □ Placator □ Blamer □ Superreasonable □ Irrelevant |
|
AM or |
|
|
: □ Congruent □ Placator □ Blamer □ Superreasonable □ Irrelevant |
|
CF or |
|
|
: □ Congruent □ Placator □ Blamer □ Superreasonable □ Irrelevant |
|
CM or |
|
|
: □ Congruent □ Placator □ Blamer □ Superreasonable □ Irrelevant |
|
Ex: |
|
|
|
|
2/19/09 9:26:52 PM

Gehart Chapter 2 02/20/2009
Case Conceptualization Form |
45 |
|
|
|
|
Hypothesis (Describe possible role or function of symptom in maintaining family homeostasis):
Intergenerational Patterns
Substance/alcohol abuse: □ NA □ Hx:
Sexual/physical/emotional abuse: □ NA □ Hx:
Parent/child relations: □ NA □ Hx:
Physical/mental disorders: □ NA □ Hx:
Historical incidents of presenting problem: □ NA □ Hx:
Family strengths:
Previous Solutions and Unique Outcomes
Solutions that DIDN
Solutions that DID work:
Narratives, Dominant Discourses, and Diversity
Dominant Discourses informing deinition of problem:
Cultural, ethnic, SES, etc.:
Gender, sex orientation, etc.:
Other social inluences:
Identity Narratives that have developed around problem for AF, AM, and/or CM/F:
Local or Preferred Discourses:
Other Inluential Discourses:
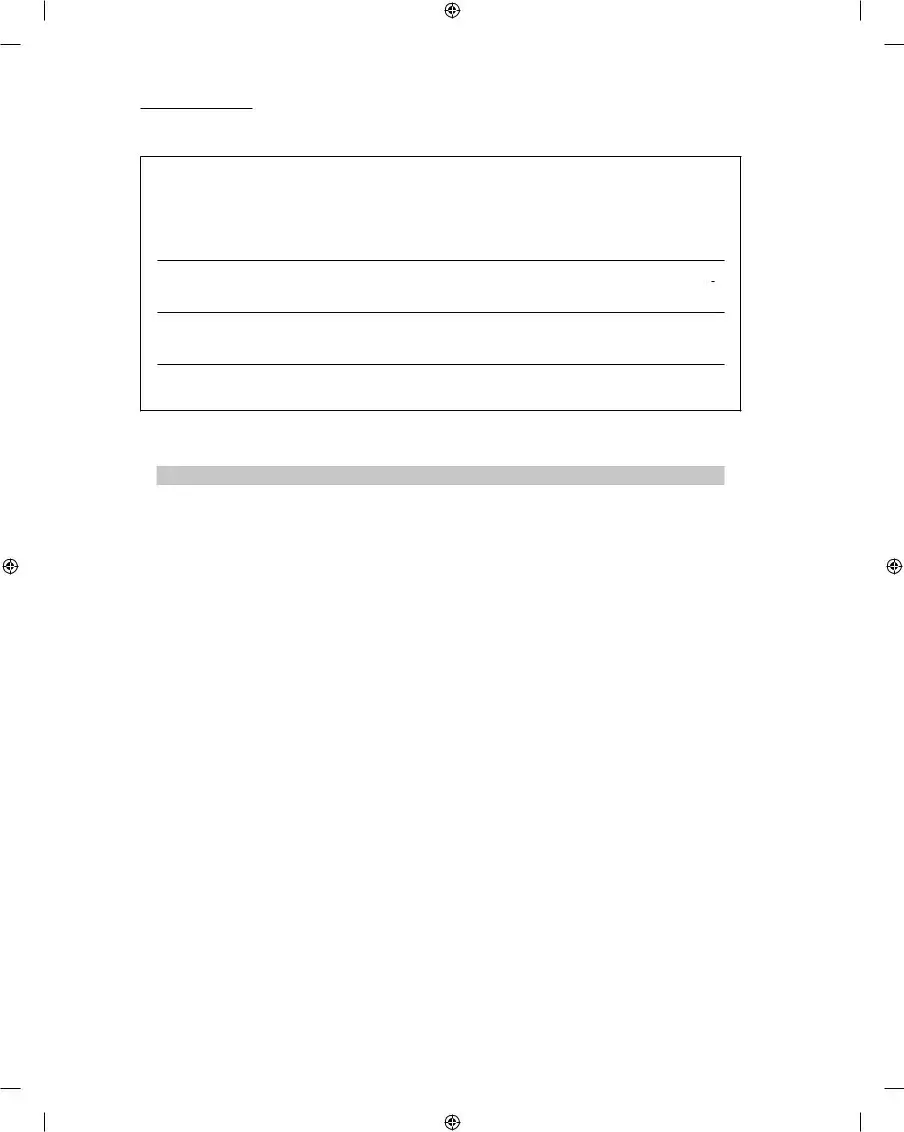
V. Genogram
Construct a family genogram and include all relevant information, including:
•ages, birth/death dates
•names
•relational patterns
•occupations
•medical history
•psychiatric disorders
•abuse history
Also include a couple of adjectives for persons frequently discussed in session (these should describe personal qualities and/or relational patterns, e.g., quiet, family caretaker, emotionally distant, perfectionist, helpless, etc.). Genogram should be attached to report.
(continued)
2/19/09 9:26:53 PM
Gehart Chapter 2 02/20/2009
46CHAPTER 2 Case Conceptualization
(continued)
VI. Client Perspectives
Areas of Agreement: Based on what the client(s) has(ve) said, what parts of the above assessment do they agree with or are likely to agree with?
Areas of Disagreement: What parts do they disagree with or are likely to disagree with? Why?
How do you plan to respectfully work with areas of disagreement?
©2007. Diane R. Gehart
CASE CONCEPTUALIZATION SCORING RUBRIC
The following scoring rubric describes the differences between exemplary, adequate, and deicient case conceptualizations. By closely attending to these requirements, you can hone in on what your instructors and supervisors are looking for when they grade your work.
2/19/09 9:26:53 PM |
Form Characteristics
| Fact Name | Fact Description |
|---|---|
| Purpose | The Case Conceptualization form helps therapists systematically evaluate and document a client's situation, including problems, strengths, and background. |
| Client Information | It requires personal details about the client, including age, ethnicity, and relevant identifiers, ensuring a comprehensive understanding of the subject. |
| Presenting Concerns | The therapist must detail the client's and their family's descriptions of problems, which provides insight into the client's perspective on their challenges. |
| Background Assessment | Sections exist to capture recent and historical background information, which are crucial for understanding the client's overall context and history. |
| Family and Social Interaction | The form assesses family structure and interaction patterns, including subsystem dynamics, communication styles, and generational issues. |
| State-Specific Guidelines | In some states, certain laws govern the use and format of the Case Conceptualization form, ensuring adherence to legal and ethical standards in client reporting. |
Guidelines on Utilizing Case Conceptualization
Filling out the Case Conceptualization form is an important step in understanding a client's situation and the dynamics within their family or relational system. By gathering thorough information, a clearer picture emerges that can guide future therapy sessions. Follow the steps listed below to complete this form effectively.
- Begin with Client Details: Write down the therapist's name, client or case number, and date at the top of the form. Include details about the client, such as age, ethnicity, and occupation, as well as marking any individuals in the session with an asterisk (*) or identifying the patient (IP).
- Presenting Concerns: Describe the client’s or family’s issues as they perceive them. Also, include how others, like teachers or relatives, view the presenting problems.
- Gather Background Information: Document recent changes and stressors in the client’s life, as well as any related historical background, such as family history or prior counseling experiences.
- Conduct Systemic Assessment: Assess the client’s strengths and social relationships. Include information about the family structure and interaction patterns, and make note of any couple dynamics and communication styles as described in the form.
- Explore Hypotheses: Describe any thoughts on how the presenting symptoms might be keeping the family stable. Also, note intergenerational patterns related to issues like substance abuse or trauma.
- Identify Previous Solutions: List what has worked and what hasn't in the past when addressing the identified issues.
- Include Identity Narratives: Examine any cultural or social influences on the problem and the narratives that have evolved around it for each relevant individual.
- Create a Genogram: Draw a family genogram that includes essential details like ages, birth and death dates, names, occupations, and relevant medical or psychological histories. Attach this to your report.
- Summarize Client Perspectives: Record areas of agreement and disagreement based on the client's input and outline ways to work respectfully through discrepancies.
What You Should Know About This Form
What is the purpose of the Case Conceptualization form?
The Case Conceptualization form serves as a structured tool for therapists to gather comprehensive information about a client and their circumstances. It helps in identifying the client's concerns and situating them within a broader systemic context. This process aids in formulating treatment plans that are tailored to the unique needs of each individual or family.
Who should complete the Case Conceptualization form?
The therapist, counselor, or mental health professional involved in the client’s treatment should complete the form. It is designed for use during or after the initial assessment phase, ensuring that the therapist captures all relevant information in a systematic way.
What types of information are included in the introduction section?
The introduction section requires details about the client including age, ethnicity, occupation, and any significant others that may impact the case. This section sets the foundation for understanding the client's background and context.
How are presenting concerns documented in the form?
Presenting concerns are documented through descriptions provided by the client and their family. This captures their perspective on the problems faced. Additionally, information from external sources such as teachers or relatives may also be included, offering a holistic view of the issue.
What is meant by "systemic assessment" in the form?
The systemic assessment examines the client’s strengths, interaction patterns within the family, and relationships among family members. This analysis enables the therapist to identify dynamics that may contribute to the presenting concerns.
Why is it important to include a genogram in the Case Conceptualization?
A genogram visually represents family relationships and history, including ages, occupations, and medical conditions. This detailed illustration helps therapists understand patterns, dynamics, and potential areas of concern that may influence the client's current situation.
What do "areas of agreement" and "areas of disagreement" refer to in the context of client perspectives?
Areas of agreement reflect points within the assessment that the client acknowledges as accurate or relevant. Conversely, areas of disagreement highlight aspects the client challenges. Understanding these perspectives is crucial for fostering a collaborative therapeutic relationship.
How can past solutions and unique outcomes inform current treatment?
Documenting past solutions and unique outcomes provides insights into what has or hasn’t worked for the client previously. This knowledge can guide current therapeutic strategies, helping avoid ineffective approaches while building on successful tactics.
What role does cultural context play in the Case Conceptualization?
Cultural context is essential in shaping the client's experiences and perceptions. The form prompts the inclusion of various cultural factors, such as gender, socioeconomic status, and ethnicity, allowing for a more nuanced understanding of the problems presented.
How does the Case Conceptualization form contribute to the treatment plan?
Once completed, the Case Conceptualization form guides the development of a targeted treatment plan. It assists the therapist in identifying specific goals, strategies, and interventions that align with the client's unique needs and circumstances.
Common mistakes
Filling out the Case Conceptualization form correctly is essential for effective therapy and understanding clients. However, there are common mistakes that people often make. One big error is failing to provide enough detail in the Introduction to Client section. The more background information you include—like age, ethnicity, and relevant identifiers—the better your understanding of the client will be. Omitting these details can hinder the therapeutic process.
Another frequent mistake is not capturing the full scope of the Presenting Concern. When clients describe their problems, it’s important to get a clear and comprehensive understanding. If you only write down superficial aspects, you might miss crucial information that affects treatment. Remember to include not only the client’s view but also how others in their environment perceive the issues.
In the Background Information section, people sometimes skip over describing significant life changes or events. These changes can be key to understanding the client's current state. Ignoring them can lead to a lack of context for the issues being addressed in therapy. Similarly, not including past trauma or previous counseling experiences can result in missing elements that might influence the client’s behavior and attitudes.
When assessing the family structure and interaction patterns, individuals often overlook the importance of family dynamics. It’s essential to note how family roles and relationships influence the client. Failing to assess the hierarchy between parents and children can lead to misinterpretations of behaviors, further complicating therapy goals.
Another common mistake is neglecting to provide adequate information in the section about client perspectives. The areas of agreement and disagreement can reveal significant insights into what the client values and how they perceive their situation. Without this information, it’s challenging to build a strong therapeutic relationship, as understanding the client’s views is fundamental.
Lastly, many forget to include a thorough genogram. This visual representation should include important details about family history and relationships. Omitting this can prevent a comprehensive understanding of the family dynamics at play. Taking the time to create an accurate genogram can make a significant difference when analyzing patterns and influences in the client's life.
Documents used along the form
When working with clients, several documents often accompany the Case Conceptualization form to offer a more comprehensive view of the client's situation and therapeutic needs. Each form serves a specific purpose, ensuring that all aspects of the client’s life and challenges are addressed. Below is a list of related documents that you may encounter.
- Intake Form: This initial document is essential for gathering basic information about the client. It typically includes personal details, contact information, and a brief overview of the reasons for seeking therapy.
- Informed Consent Form: This form outlines the therapeutic process and the rights of the client. It is crucial for establishing trust, as it ensures clients understand the nature of their sessions, confidentiality, and their rights.
- Treatment Plan: This document details the objectives and goals for therapy. It outlines strategies and interventions that will be used to guide the therapeutic process, adapting as the client progresses.
- Progress Notes: Progress notes provide a record of each session, summarizing interactions, changes in the client's condition, and any significant events. This documentation helps track progress over time.
- Referral Form: When clients need additional services or specialists, a referral form offers a formal way to identify and recommend those resources. It ensures clients receive the in-depth support they may require.
- Assessment Tools: Various standardized assessment tools can be used to evaluate specific issues, such as depression or anxiety levels. These tools help guide the treatment approach effectively.
- Genogram: A visual representation of family relationships, a genogram helps illustrate dynamics within families and can reveal patterns of behavior or relational issues that might inform treatment.
- Termination Summary: When therapy concludes, a termination summary provides an overview of the client’s journey, including accomplishments and areas to continue working on in the future. This document is valuable for both the therapist and the client in reflecting on the therapeutic process.
Each of these documents plays a vital role in the therapeutic process. Together, they create a clearer picture of the client's needs and facilitate a more effective therapeutic journey. Understanding what each document communicates ensures good practice and enhances the overall success of therapy.
Similar forms
- Clinical Intake Form: Similar to the Case Conceptualization form, this document collects essential client information, such as personal history and presenting concerns, to help therapists understand the client’s situation.
- Assessment Report: This report summarizes the evaluations conducted, highlighting the client’s issues and background, aligning closely with the assessment section found in the Case Conceptualization form.
- Treatment Plan: Both documents work hand in hand. The Treatment Plan outlines the strategies for addressing the client's issues, often formulated based on insights gathered in the Case Conceptualization form.
- Progress Notes: These notes track the client's sessions and progress, much like how the Case Conceptualization form reflects the client's evolving state and the effectiveness of interventions.
- Genogram: This tool visually maps family relationships and histories, similar to how the Case Conceptualization form seeks to understand the broader familial context affecting the client.
- Referral Form: This document provides information about a client referred by another professional. It often includes concerns related to treatment as seen in the Case Conceptualization form.
- Client Feedback Form: Feedback from clients about their experience can aid therapists in aligning treatment with client perspectives, paralleling the Case Conceptualization form's focus on client input.
- Risk Assessment Form: This assessment highlights potential risks the client may face, akin to how the Case Conceptualization form evaluates presenting concerns and significant stressors.
- Session Summary: These summaries capture the highlights of therapy sessions. Like the Case Conceptualization form, they reference previous discussions and outline future directions for treatment.
Dos and Don'ts
When filling out the Case Conceptualization form, it's important to be thorough and precise. Here’s a list of things you should and shouldn't do to ensure the form is completed effectively.
- Do provide accurate details about the client, including age, ethnicity, and relevant identifiers.
- Do describe the presenting concerns thoroughly. Include the perspectives of all family members involved.
- Do gather recent and historical background information. This context is crucial for understanding the client’s situation.
- Do assess relationships and family dynamics clearly. Note any patterns that may affect the client's issues.
- Do create a genogram to visualize family relationships and relevant histories.
- Don't skip sections. Each part of the form contributes to a complete understanding of the case.
- Don't use vague language. Be specific about concerns and strengths to avoid misunderstandings.
- Don't overlook the client's perspective. Document their agreement or disagreement with the issues presented.
- Don't rush through the assessment. Take your time to ensure clarity and accuracy in your observations.
Misconceptions
- Case Conceptualization Forms are Only for Therapists: Many people believe that this form is exclusively designed for therapists. In reality, anyone involved in client care, including social workers and counselors, can benefit from using it to enhance understanding and communication.
- It's a One-Size-Fits-All Approach: Some think that the Case Conceptualization form is the same for every client. However, each completed form is tailored to the unique characteristics and challenges of the individual or family being assessed.
- It’s Mainly About Diagnosing Issues: There is a misconception that the primary focus of the form is to diagnose problems. In truth, it serves a broader purpose by examining strengths, relational dynamics, and factors contributing to the presenting concerns.
- Only Negative Aspects Are Assessed: Some assume the form is solely focused on negative behavior patterns or dysfunctions. Conversely, it emphasizes client and relational strengths, promoting a more holistic view of the situation.
- Once Completed, It’s Set in Stone: People may think that the information gathered on the form is static. In actuality, the form is a living document that can be updated as new insights and developments arise during therapy.
- Client Participation is Not Necessary: There's a belief that clients do not need to engage with the form. However, involving clients in this process fosters collaboration and enhances their understanding of their circumstances.
- The Form's Use is Limited to Initial Assessment: Some might believe that the form's utility ends after the first session. In contrast, it serves as an ongoing resource for tracking progress and adapting strategies as therapy unfolds.
Key takeaways
The Case Conceptualization form is a vital tool for understanding client dynamics and needs. Here are some key takeaways for ensuring effective completion and application of this form:
- Thorough Client Overview: Provide comprehensive details about the client and significant others, including age, ethnicity, and relevant identifiers. This context sets the stage for understanding the presenting issues.
- Presenting Concerns Matter: Document both the client's and broader system’s descriptions of problems. Different perspectives can offer insights into the root causes and mutual dynamics influencing the situation.
- Historical Context is Key: Fill in recent and historical background information. Understanding past stressors, family history, and prior counseling experiences informs the current dynamics and symptoms.
- Assess Systemic Interactions: Examine family structures, interaction patterns, and communication styles. Identifying strengths and weaknesses in relationships can guide therapeutic interventions and improve client outcomes.
Browse Other Templates
Dte Poly - Communicate any changes in your circumstances that may affect your energy needs.
Electrician Certification Texas - Applicants must be at least 18 years old to qualify for the license.