Fill Out Your Certification Of Incapacity Form
The Certification of Incapacity form plays a critical role in medical decision-making for patients who are unable to communicate their treatment preferences. It requires the evaluation of two qualified physicians who must attest to the patient's capacity to understand their medical situation. The form begins with a certification from the attending physician, who must document the patient's condition and assert that the patient cannot make informed decisions about their treatment options. This includes understanding the nature of the proposed treatments as well as weighing the potential risks and benefits. The second physician's certification serves as a safeguard, ensuring that another medical professional agrees with the assessment. Both certifications must be completed within a two-hour window of each examination, emphasizing the time-sensitive nature of patient care. Clarity and precision are crucial throughout the form, as it aims to protect the patient's rights while ensuring that medical professionals have the necessary authority to act in the patient's best interests when the patient cannot do so themselves.
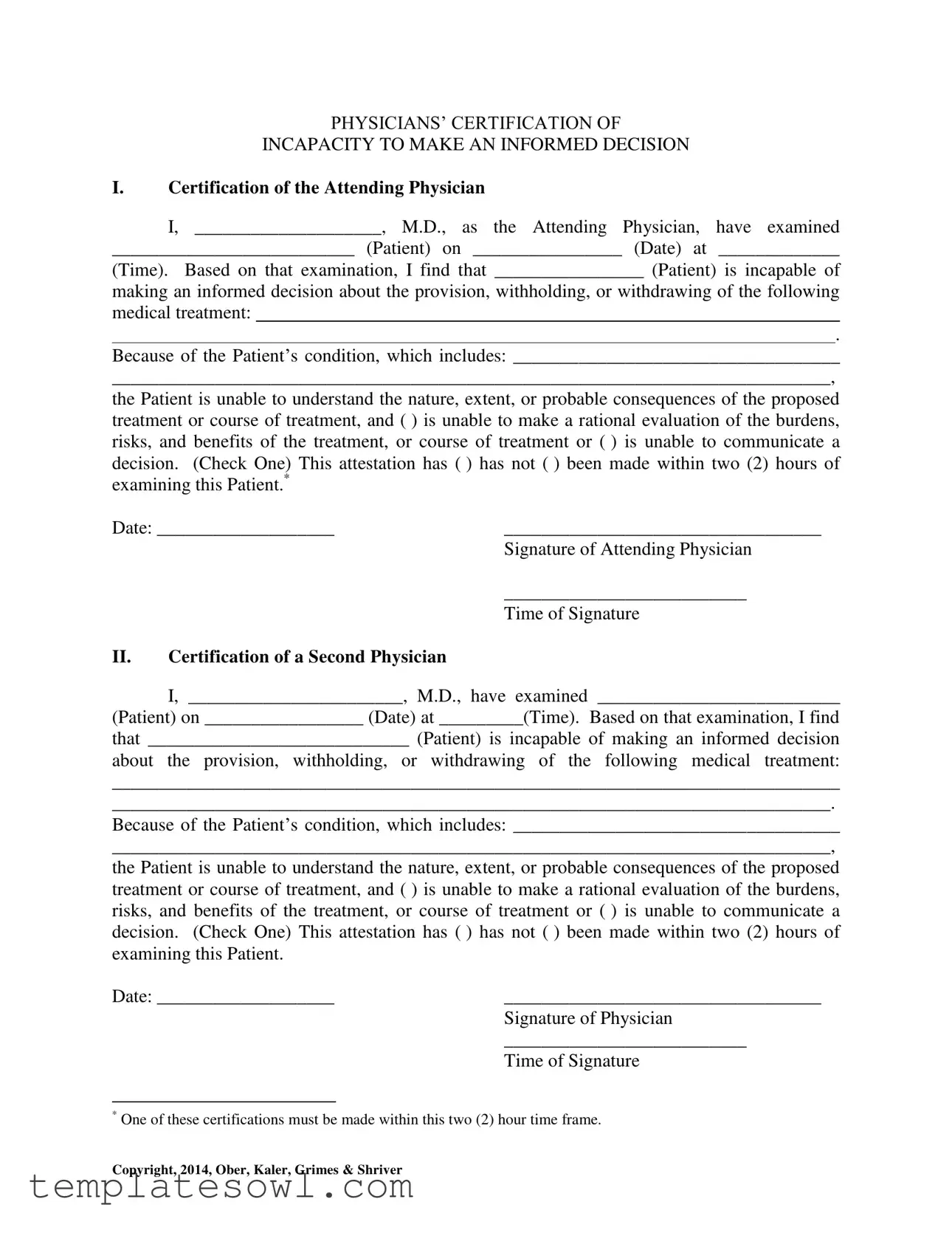
Certification Of Incapacity Example
PHYSICIANS’ CERTIFICATION OF
INCAPACITY TO MAKE AN INFORMED DECISION
I.Certification of the Attending Physician
I, ____________________, M.D., as the Attending Physician, have examined
__________________________ (Patient) on ________________ (Date) at _____________
(Time). Based on that examination, I find that ________________ (Patient) is incapable of
making an informed decision about the provision, withholding, or withdrawing of the following medical treatment:
.
Because of the Patient’s condition, which includes: ___________________________________
_____________________________________________________________________________,
the Patient is unable to understand the nature, extent, or probable consequences of the proposed treatment or course of treatment, and ( ) is unable to make a rational evaluation of the burdens, risks, and benefits of the treatment, or course of treatment or ( ) is unable to communicate a decision. (Check One) This attestation has ( ) has not ( ) been made within two (2) hours of examining this Patient.*
Date: ___________________ |
__________________________________ |
|
Signature of Attending Physician |
|
__________________________ |
|
Time of Signature |
II.Certification of a Second Physician
I, _______________________, M.D., have examined __________________________
(Patient) on _________________ (Date) at _________(Time). Based on that examination, I find
that ____________________________ (Patient) is incapable of making an informed decision
about the provision, withholding, or withdrawing of the following medical treatment:
______________________________________________________________________________
_____________________________________________________________________________.
Because of the Patient’s condition, which includes: ___________________________________
_____________________________________________________________________________,
the Patient is unable to understand the nature, extent, or probable consequences of the proposed treatment or course of treatment, and ( ) is unable to make a rational evaluation of the burdens, risks, and benefits of the treatment, or course of treatment or ( ) is unable to communicate a decision. (Check One) This attestation has ( ) has not ( ) been made within two (2) hours of examining this Patient.
Date: ___________________ |
__________________________________ |
|
Signature of Physician |
|
__________________________ |
|
Time of Signature |
*One of these certifications must be made within this two (2) hour time frame.
Copyright, 2014, Ober, Kaler, Grimes & Shriver
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of the Form | This form certifies that a patient is unable to make informed medical decisions regarding their treatment. |
| Physician's Certification | It requires the signature of two physicians, confirming the patient's incapacity to make decisions. |
| Time Frame for Certification | At least one of the physician certifications must be documented within two hours of examining the patient. |
| State-Specific Law | Laws governing this form may vary by state. For instance, in California, it follows the Health & Safety Code § 7100. |
| Patient's Condition | The form requires a detailed description of the patient’s current medical condition impacting their decision-making ability. |
Guidelines on Utilizing Certification Of Incapacity
Filling out the Certification of Incapacity form involves several steps that require careful attention to detail. This process begins with a medical examination and requires input from two physicians to assess the patient's ability to make informed medical decisions. Following the completion of this form, the patient's healthcare team will use the information to guide treatment decisions.
- Obtain the form and ensure you have a clear understanding of the patient's situation.
- As the Attending Physician, fill in your name and credentials at the top of the first section of the form.
- Enter the patient’s full name, examination date, and time of examination in the designated spaces.
- Provide a clear explanation regarding the patient’s incapacity to make informed decisions related to specified medical treatments.
- Detail the patient's condition that contributes to their inability to understand the proposed treatment options.
- Check the box that corresponds to the specific reason for the patient’s incapacity: unable to evaluate the treatment or unable to communicate a decision.
- Indicate whether the attestation was made within two hours of the examination by checking the appropriate box.
- Date the document, then provide your signature along with the time of signing.
- For the second physician, repeat steps 2 through 8, ensuring all information is accurate and complete.
What You Should Know About This Form
What is the purpose of the Certification of Incapacity form?
This form serves a crucial function in documenting that a patient is unable to make informed decisions regarding their medical treatment. It is created following an examination by a physician, who attests to the patient's incapacity based on their evaluation. This certification can be vital in situations where critical medical decisions need to be made on behalf of a patient who cannot communicate their wishes.
Who can complete the Certification of Incapacity form?
The form must be completed by an attending physician who examines the patient. In some cases, a second physician may also need to evaluate the patient and provide their certification. This dual assessment helps ensure that the determination of incapacity is thorough and reliable.
What conditions might lead to a patient being deemed incapable of making informed decisions?
A range of medical conditions could contribute to a patient's incapacity, including cognitive impairments, severe mental health issues, unconsciousness, or significant physical ailments that affect their cognitive function. The specific conditions must be documented on the form, reflecting the physician's observations and findings during the examination.
Is there a time frame within which the certifications must occur?
Yes, at least one of the physician's certifications must be completed within two hours of examining the patient. This time-sensitive condition helps ensure that the assessments are relevant to the patient’s current state and can accurately reflect their ability or inability to make informed decisions.
What information is required in the Certification of Incapacity form?
The form requires several key pieces of information. It includes the names and signatures of the attending physician and any second physician, patient's name, examination date and time, a description of the proposed treatment, and the specific reasons for the determination of incapacity. Both physicians must check one of two options regarding the patient’s ability to evaluate treatment options or communicate decisions.
Can the form be used for any medical treatment?
The Certification of Incapacity form can be utilized for various medical treatments, including the provision, withholding, or withdrawal of treatment. It allows for flexibility in different healthcare scenarios while maintaining clarity about the patient's capacity to make informed decisions regarding their medical care.
What happens if a patient regains their capacity to make decisions?
If a patient regains the ability to make informed decisions, they can resume control over their medical treatment choices. It is essential for healthcare providers to continuously assess a patient's capacity, as this can change over time due to the nature of their medical condition or treatment responses.
How should patients or their families proceed if they have questions about the form?
Patients or their families should discuss any questions or concerns with their healthcare providers. Open communication is vital in understanding the implications of the Certification of Incapacity. Healthcare professionals can offer guidance and clarify any uncertainties related to the form and its use in specific medical situations.
Common mistakes
When completing the Certification of Incapacity form, individuals often overlook essential details that can lead to complications. One common mistake is failing to include the correct details about the patient. The patient's name, date, and time of the examination are crucial elements needed for the document to be valid and serve its purpose. Omitting this information can render the certification incomplete and ineffective.
Another frequent error occurs when physicians do not accurately describe the patient’s condition. This section is vital, as it provides context for the incapacity and outlines the specific medical issues at hand. Vague statements or generalizations fail to convey the seriousness of the situation and can make the certification less credible.
Checking the appropriate boxes regarding the patient's ability to make decisions is another area where mistakes arise. There are specific options intended to clarify whether the patient is unable to evaluate risks or communicate a decision. Misinterpreting these options or selecting both can lead to confusion. It is important to choose only one that accurately reflects the patient's condition.
Completing the form within the required timeframe is essential, yet some physicians neglect this requirement. The instructions specify that one of the certifications must be made within two hours of examining the patient. Not adhering to this guideline can lead to questions about the validity of the certification and may complicate legal or medical proceedings.
Finally, neglecting to sign and date the form correctly is a mistake that can undermine the entire certification process. The signatures of both physicians must be clear. The dates must coincide with the examination dates to establish a timeline. It is also advisable to double-check that all sections are filled out adequately before submitting the form.
Documents used along the form
The Certification of Incapacity form typically works in conjunction with several other important documents. Understanding these forms can help ensure that a patient's health care decisions are handled properly when they cannot make choices for themselves. Below is a list of forms that are often used alongside the Certification of Incapacity.
- Advanced Healthcare Directive: This document allows individuals to outline their preferences for medical treatment if they become unable to communicate. It enables patients to appoint a healthcare proxy to make decisions on their behalf.
- Durable Power of Attorney for Healthcare: This form designates a specific person to make healthcare decisions for someone if they are incapacitated. It grants the appointed agent the authority to act in the best interests of the patient.
- Do Not Resuscitate (DNR) Order: A DNR order instructs medical personnel not to perform CPR if the patient's heart stops or they stop breathing. It must be signed by a physician and is crucial for end-of-life preferences.
- Physician Orders for Life-Sustaining Treatment (POLST): This medical order translates a patient’s wishes about treatment into actionable orders for healthcare providers. It is suitable for seriously ill patients and complements advance directives.
- Declaration of Guardian: In this document, individuals can express their preference for a guardian who would manage their affairs should they become incapable of doing so. This ensures the person making decisions is trusted and chosen by the individual.
- Medical Information Release Authorization: This form allows patients to authorize the sharing of their medical information with designated individuals or organizations. This is crucial for the appointed healthcare proxy or guardian to make informed decisions.
Each of these forms plays a vital role in medical and legal decisions when a patient is unable to advocate for themselves. Proper completion and sharing of these documents can provide peace of mind and clarity in critical situations.
Similar forms
- Durable Power of Attorney for Healthcare: This document allows a person to designate someone else to make healthcare decisions on their behalf when they are unable to do so. Like the Certification of Incapacity form, it emphasizes the individual's incapacity to make informed choices about their medical care.
- Living Will: A living will outlines a person's wishes regarding medical treatment in situations where they are unable to communicate. Similar to the Certification of Incapacity, it focuses on the individual's preferences and decision-making capabilities under specific medical conditions.
- Healthcare Proxy: A healthcare proxy designates someone to act on behalf of a patient regarding medical decisions if they become incapacitated. This document also mirrors the concept of the Certification of Incapacity by addressing the importance of having a representative for someone who cannot make their own decisions.
- Mental Health Declaration: This form addresses an individual's right to have a say in their mental health treatment even when they may not be able to make rational decisions. Similar to the Certification of Incapacity, it assesses mental capacity and the necessity for alternative decision-making structures.
- Do Not Resuscitate (DNR) Order: A DNR order specifies a patient’s wishes regarding resuscitation in case their heart stops. This document, like the Certification of Incapacity, arises from a determination of a patient's understanding and preferences regarding their medical treatment.
- Advance Healthcare Directive: This directive combines elements of a living will and a healthcare proxy, allowing individuals to specify their treatment preferences and appoint someone to make decisions for them. It parallels the Certification of Incapacity in its focus on a person's decisions in the face of incapacity.
- Patient Consent Form: While typically used for acknowledging understanding of a specific treatment, this form also implies the need for the patient to be capable of making informed decisions. This shares similarities with the Certification of Incapacity in assessing the individual's decision-making ability regarding medical procedures.
Dos and Don'ts
When filling out the Certification of Incapacity form, there are important guidelines to follow. The following list outlines the dos and don’ts to ensure accuracy and compliance.
- Do provide complete and accurate information for both the patient and the physician.
- Do check the box that corresponds with the patient's ability to evaluate treatment options.
- Do ensure that the certification is signed and dated by both attending and second physician.
- Do complete the form within the specified two-hour time frame.
- Don’t leave any sections of the form blank.
- Don’t use vague language when describing the patient's condition.
- Don’t forget to document the date and time clearly.
- Don’t overlook the requirement for a second physician's certification if necessary.
Misconceptions
Misconceptions about the Certification of Incapacity form can lead to confusion for patients, families, and healthcare providers alike. Understanding these can help clarify its purpose and proper use. Below are common misconceptions:
- Only one physician's signature is needed. Many believe that only one physician's certification suffices, but the form typically requires the signatures of two physicians to confirm incapacity.
- Patients must have a permanent condition. Some think the form only applies to those with permanent disabilities. However, it can be used for temporary conditions that affect decision-making.
- The form is only relevant for end-of-life decisions. This is inaccurate. The Certification of Incapacity form can apply to all kinds of medical treatments, not just those regarding life support or end-of-life care.
- It guarantees that a patient will not recover. Many assume that completing this form indicates a patient cannot improve. In reality, it addresses the patient’s current ability to make informed decisions.
- If a patient appears incapacitated, the form is unnecessary. It is a common misconception that visual signs of incapacity are enough. The form provides a formalized and documented assessment by qualified physicians.
- Families can override the form. Some believe family members can simply disregard the form. However, if the form is properly filled out, it should be respected by all healthcare providers.
- The two-hour timeframe is optional. In fact, one of the key requirements is that the certifications must occur within a two-hour period to ensure timely assessments.
- Once completed, the form is permanent. This is misleading. The form must be reevaluated and could be updated as the patient's condition changes.
By addressing these misconceptions, individuals can approach the Certification of Incapacity form with a clearer understanding of its significance and requirements.
Key takeaways
Here are some key takeaways for filling out and using the Certification of Incapacity form:
- The form requires the certification of two physicians to confirm a patient's incapacity.
- Both physicians must examine the patient and document their findings and reasoning clearly.
- It's important to indicate the specific medical treatment the patient is unable to make decisions about.
- Physicians need to check whether the patient can understand the proposed treatment or communicate a decision.
- Each certification must be completed within two hours of examining the patient.
- Make sure to include both the date and time of the examination when filling out the form.
- Both physicians must sign and date the form to make it valid and enforceable.
Browse Other Templates
Conditional Waiver and Release on Progress Payment California - Treat this waiver as an important element in safeguarding your interests in property improvements.
Mission Papers - Ensure that the recommendation forms align with the latest instructions from Church leadership.
Cac2 Form - Timely submissions help maintain the integrity of apprenticeship programs.