Fill Out Your Champva Claim Va 10 7959A Form
When navigating the world of healthcare benefits, understanding the necessary forms can be daunting. The CHAMPVA Claim VA Form 10-7959A plays a crucial role in the process of claiming benefits through the Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA). This form is specifically designed for beneficiaries to submit their healthcare claims and is essential for patient, sponsor, or guardian completion. It is important to remember that this form is not for provider claims, ensuring that all submissions come directly from those applying for benefits. Included on the form are important sections that request personal details such as patient and sponsor information, as well as any other health insurance coverage the applicant may have. Additionally, guidelines specify the necessity of attaching itemized billing statements from providers, reflecting service dates and appropriate coding for each service. The form emphasizes timeliness—claims must be submitted within one year of the service date or discharge date to be considered valid. Furthermore, users are reminded that any falsifying of information is taken seriously under federal law. With the right understanding and careful completion of the CHAMPVA Claim VA Form 10-7959A, beneficiaries can effectively navigate the claims process and work towards obtaining the medical benefits they need.
Champva Claim Va 10 7959A Example
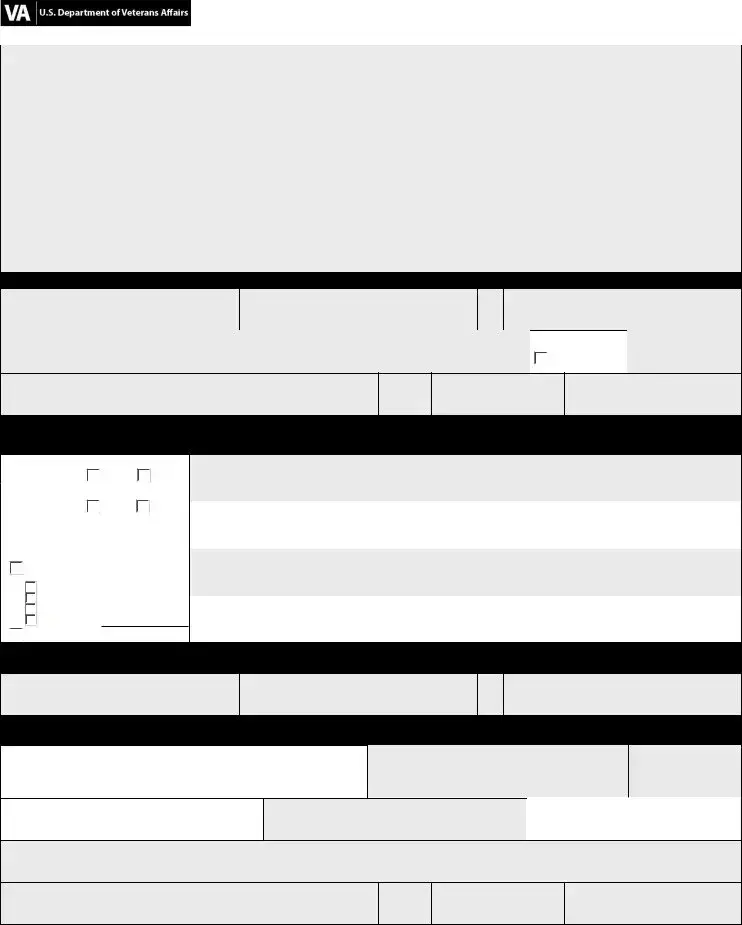
|
|
OMB Number: |
|
|
|
|
|
CHAMPVA Claim Form |
VA Health Administration Center |
CHAMPVA PO Box 469064 Denver CO |
|
Attention: After reviewing the following information, complete the form in its entirety (print or type only) and return with the required documentation.
Claim form usage: This form is to be completed by the patient, sponsor, or guardian and is mandatory for all beneficiary claims. This claim form is NOT to be used for provider submitted claims.
Other health insurance (OHI): If OHI exists, attach OHI’s Explanation of Benefits (EOB) to the provider’s itemized billing statement(s). Dates of service and provider charges on EOB must match billing statements.
Timely filing requirement: Claims must be received no later than one year after the date of service or, in the case of inpatient care, within one year of the discharge date.
Itemized billing statements: An itemized statement must be attached and contain:
•patient name, date of birth, and CHAMPVA Identification Card
•provider name, degree, tax identification number (TIN), address and telephone number; and
•service dates, itemized charges and appropriate procedure/diagnosis codes for each service (i.e.
Section I - Patient Information
Last Name (this is a mandatory field)
First Name (this is a mandatory field)
MI
CHAMPVA Member Number (this is a mandatory field)
Street Address |
|
Date of Birth (mm/dd/yyyy) |
 Check if new
Check if new
City
State
ZIP Code
Telephone Number (include area code)
Section II - Other Health Insurance (OHI) Information
By law, other coverage must be reported. Except for CHAMPVA supplemental policies, CHAMPVA is always the secondary payer.
If more space is needed, please continue in the same format on a separate sheet.
• Was treatment for a
condition? |
Yes |
No |
|
•Was treatment for an injury or accident outside of work?
Yes |
No |
•Is patient covered by other primary health insurance to include coverage through a family member (supplemental or secondary insurance excluded)?
Yes (check type below and provide coverage information on the right)
 employer sponsored (group) private (non group)
employer sponsored (group) private (non group)
 Medicare (Part A or B) other (specify)
Medicare (Part A or B) other (specify)

 no (proceed to Section III)
no (proceed to Section III)
Name of Other Health Insurance (OHI)
|
|
OHI Policy Number |
OHI Telephone Number (include area code) |
|
|
|
|
Name of Other Health Insurance (OHI)
OHI Policy Number |
OHI Telephone Number (include area code) |
|
|
Section III - Sponsor Information
Last Name
First Name
MI
CHAMPVA Member Number (this is a mandatory field)
Section IV - Claimant Certification
Federal Laws (18 USC 287 and 1001) provide for criminal penalties for knowingly submitting or making false, fictitious, or fraudulent statements or claims.
I certify that the above information and attachments are correct and represent actual services, dates, and fees charged. (Sign and
4date on right.) If certification is signed by a person other than the
patient, complete the information the signature and date.
Signature (type if electronic)
Date
Last Name
First Name
|
MI |
Relationship to Patient |
|
|
|
Street Address
City
State
ZIP Code
Telephone Number (include area code)
VA FORM |
|
MAY 2010 |
CHAMPVA Claim Form
Notice: Termination of marriage by divorce or annulment to the qualifying sponsor ends CHAMPVA eligibility as of midnight on the effective date of the dissolution of marriage. Changes in status should be reported immediately to CHAMPVA, ATTN: Eligibility Unit, PO Box 469028, Denver, CO
PRIVACY ACT INFORMATION: The authority for collection of the requested information on this form is 38 U.S.C. 501 and 1781. The purpose of collecting this information is to adjudicate and process claims for CHAMPVA benefits. You do not have to provide the requested information but if any or all of the requested information is not provided, it may delay or result in denial of your request for CHAMPVA benefits. Failure to furnish the requested information will have no adverse impact on any other VA benefit to which you may be entitled. The responses you submit are considered confidential and may be disclosed outside VA only if the disclosure is authorized under the Privacy Act, including the routine uses identified in the VA system of records 54VA16, titled "Health Administration Center Civilian Health and Medical Program Records
PAPERWORK REDUCTION ACT: This information collection is in accordance with the clearance requirements of Section 3507 of the Paperwork Reduction Act of 1995. Public reporting burden for this collection of information is estimated to average 10 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed and completing and reviewing the collection of information. Comments regarding this burden estimate or any other aspect of this collection, including suggestions for reducing the burden, may be addressed by calling the CHAMPVA Help Line,
VA FORM |
|
MAY 2010 |
Form Characteristics
| Fact Name | Fact Description |
|---|---|
| OMB Number | The form is assigned OMB Number 2900-0219. |
| Estimated Burden | Completing the form takes approximately 10 minutes on average. |
| Submission Details | Send the completed form and required documentation to the CHAMPVA Health Administration Center in Denver, Colorado. |
| Mandatory Use | This form must be completed for all beneficiary claims by the patient, sponsor, or guardian. |
| Not for Providers | This claim form is not intended for use by healthcare providers submitting claims. |
| Timely Filing | Claims must be received within one year of the date of service or one year post-discharge for inpatient care. |
| Itemized Billing Information | Attach an itemized statement that includes specific patient and provider details along with service codes. |
| Other Health Insurance | It is required to report other health insurance coverage, if applicable. CHAMPVA is usually the secondary payer. |
| Claimant Certification | The form must be signed to certify that all information is accurate and represents actual services provided. |
| Privacy Act Compliance | Information provided on this form is confidential and is collected in compliance with the Privacy Act. |
Guidelines on Utilizing Champva Claim Va 10 7959A
Once the Champva Claim VA 10 7959A form is completed with all necessary information, it should be submitted along with any required supporting documentation. Ensuring accuracy and completeness is vital for processing the claim efficiently.
- Obtain the Champva Claim VA 10 7959A form from a verified source.
- Fill out Section I - Patient Information:
- Enter the patient's last name (mandatory).
- Enter the patient's first name (mandatory).
- Include the middle initial, street address, date of birth (mm/dd/yyyy), and check if the address is new.
- Fill in the city, state, ZIP code, and telephone number (with area code).
- Move to Section II - Other Health Insurance (OHI) Information:
- Indicate if treatment was for a work-related injury or an injury outside of work (yes/no).
- Note if the patient has other primary health insurance and select the type (employer-sponsored, private, Medicare, etc.).
- If applicable, provide the name, policy number, and telephone number of the OHI.
- Proceed to Section III - Sponsor Information:
- Enter the sponsor's last name, first name, middle initial, and CHAMPVA Member Number (mandatory).
- Fill out Section IV - Claimant Certification:
- Read the certification statement regarding the accuracy of the information.
- Sign and date the form. Note the relationship to the patient, and provide the address and telephone number of the person signing, if applicable.
- Attach required documentation:
- Provide an itemized billing statement for each item billed, including essential details such as the patient’s name, date of birth, provider information, service dates, and charges.
- Include any other health insurance’s Explanation of Benefits (EOB) if applicable.
- Send the completed form and documentation to:
- CHAMPVA
- PO Box 469064
- Denver, CO 80246-9064
Confirm that all sections are complete and the correct documentation accompanies the form before submission. Upon filing, retain copies of submitted materials for your records.
What You Should Know About This Form
What is the purpose of the CHAMPVA Claim Form VA 10-7959A?
This form is designed for patients, sponsors, or guardians to submit claims for healthcare services covered by the Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA). It is essential for all beneficiary claims and is not used for claims submitted by healthcare providers directly.
Who should complete the CHAMPVA Claim Form?
The form should be filled out by the patient themselves, their sponsor, or a legal guardian. It is vital that the form is completed in its entirety, either by printing clearly or typing to ensure that all information is legible and accurate.
What documentation is required to accompany the claim form?
You must include an itemized billing statement from the provider that contains specific details such as the patient’s name, the services provided, and the associated charges. Additionally, if you have other health insurance coverage, you will need to attach the Explanation of Benefits (EOB) provided by that insurer to the billing statement.
What happens if I miss the filing deadline?
Claims should be submitted no later than one year from the date of service or, in cases involving inpatient care, within one year of the discharge date. If you fail to submit within this timeframe, your claim may be denied. It is crucial to adhere to these timelines to ensure your benefits are processed effectively.
Do I need to provide information about other health insurance?
Yes, reporting information about any other health insurance coverage is mandatory, except for CHAMPVA supplemental policies. If other coverage exists, CHAMPVA acts as a secondary payer, and the details must be correctly filled out in the form.
What details should be included in the itemized billing statement?
The billing statement must include the patient’s name, date of birth, and CHAMPVA Member Number. Additionally, it should detail the provider's name, tax identification number, service dates, and itemized charges for each service rendered, along with the proper procedure and diagnosis codes.
Is there a penalty for submitting false information on the claim form?
Yes, knowingly submitting false or misleading information on the claim form is considered a serious offense and can result in criminal penalties. It is essential to certify the accuracy of all information provided and ensure compliance with federal laws.
Can I submit the form electronically?
The form can be submitted electronically, but a signature is still required. If you are signing on behalf of the patient, you need to include your relationship to the patient and provide your own contact information as well.
What should I do if there are changes in my marital status?
It is important to report any changes in marital status immediately to CHAMPVA. A termination of marriage by divorce or annulment affects CHAMPVA eligibility, and timely notification will help prevent any disruption in benefits.
Where should I send the completed form?
The completed CHAMPVA Claim Form should be mailed to the CHAMPVA Health Administration Center at PO Box 469064, Denver, CO 80246-9064. Be sure to keep a copy for your records and check that you have attached all necessary documentation before sending your claim.
Common mistakes
Filling out the CHAMPVA Claim VA 10-7959A form can be challenging. Many people make mistakes that can delay their claims or result in outright denials. One common mistake is not completing the form in its entirety. Every section must be filled out accurately. This includes mandatory fields like the patient’s last name, first name, and CHAMPVA member number. Omitting even one of these can lead to issues.
Another frequent error involves the attachment of documentation. It is essential to include itemized billing statements and the Other Health Insurance (OHI) Explanation of Benefits (EOB) when applicable. If OHI exists, the dates of service and provider charges on the EOB must exactly match those on the billing statements. Not doing this can create misunderstandings and delays.
Some individuals also neglect to check for timely filing requirements. Claims must be submitted within one year of the date of service or discharge. Ignoring this timeline can mean that claims are unable to be processed, leading to significant frustration for patients and their families.
Improper signatures are another area where mistakes happen. Certification is mandatory. If the signature is provided by someone other than the patient, it is important to fill out their information correctly. An incorrectly signed form can lead to difficulties in processing the claim.
Many people fail to report other health insurance coverage. By law, any existing coverage must be disclosed. This includes supplemental or secondary insurance. Failure to report these can complicate the processing of the claim and potentially lead to denials.
While filling out the form, ensure that the information corresponds with the official records. Discrepancies, like mismatched names or identification numbers, can lead to confusion and delays. Always double-check the spellings and numbers before submitting the form.
Lastly, individuals often forget to keep copies of their submissions. This is a vital part of the process. Having records of what has been sent can be invaluable if there are further questions or if the claim needs to be followed up on.
By avoiding these common pitfalls, you can streamline the claims process and improve your chances of a successful outcome when submitting the CHAMPVA Claim VA 10-7959A form.
Documents used along the form
Filing a claim using the CHAMPVA Claim VA 10-7959A form is just one component of the process to secure health benefits for eligible individuals. To enhance the effectiveness of your claim, several other forms and documents are often needed. Below is a list of essential documents that may accompany your claim, ensuring all necessary information is submitted for processing.
- Itemized Billing Statement: This document provides a detailed breakdown of charges from healthcare providers. It must include patient information, provider details, dates of service, and specific charges, making it a crucial part of the claims process.
- Explanation of Benefits (EOB) from Other Insurance: If other health insurance exists, the EOB outlines coverage specifics and any amounts the insurer has paid. This is vital for verifying secondary payment responsibilities.
- CHAMPVA Eligibility Verification: This document confirms that the patient is indeed eligible for CHAMPVA benefits, providing necessary identification details for the claim process.
- Medical Records: These records may be necessary to verify the services provided and justify the medical necessity of treatments received. They should be dated and signed by the provider.
- Patient Authorization Form: If someone other than the patient is handling the claim, this form gives them permission to act on behalf of the patient, ensuring compliance with privacy laws.
- Provider’s Tax Identification Number (TIN): Including a TIN is important for verifying the identity of the healthcare provider and ensuring proper payment routing for services rendered.
- Claimant Certification: This is a necessary declaration signed by the claimant, ensuring that all information provided is accurate, which affirms the legitimacy of the claim.
Each of these documents plays an integral role in ensuring a smooth claims process for CHAMPVA benefits. Having everything prepared and in order can significantly speed up the review and approval of the claim, allowing for timely access to necessary healthcare services.
Similar forms
- UB-04 (CMS-1450): The UB-04 form is used for hospital and healthcare facility billing. Like the CHAMPVA form, it requires detailed patient and provider information, itemized service descriptions, and adherence to timely filing requirements. Both forms help process claims for reimbursement from health insurance programs.
- CMS-1500: This form serves similar purposes for individual healthcare providers. It gathers patient and insurance details along with the provider's itemized billing information, facilitating claims for reimbursement under various insurance plans.
- VA Form 21-526EZ: This form is for veterans seeking disability compensation. It shares similarities regarding the need for personal documentation and verification of service and disability status, just as the CHAMPVA form does for healthcare claims.
- VA Form 10-10EZ: This application form for VA health care also requires similar patient data. Information regarding service dates and medical treatment aligns with the requirements set forth by the CHAMPVA Claim form.
- Health Insurance Claim Form (HICF): The HICF, primarily used by non-Medicare health insurers, requires patient information, provider details, and a breakdown of services similar to what the CHAMPVA form mandates.
- Medicare Secondary Payer (MSP) Questionnaire: This form is used when Medicare is not the primary payer. It gathers patient insurance information and service details, akin to the OHI information required on the CHAMPVA form.
Dos and Don'ts
When filling out the Champva Claim VA 10 7959A form, attention to detail can make a significant difference in the outcome of your claim. Here are important dos and don’ts to consider.
- Do complete the form in full. Every section must be filled out appropriately, paying special attention to mandatory fields.
- Do use clear and legible handwriting. If possible, type the information to avoid any misinterpretation of your entries.
- Do attach the necessary documentation, such as itemized billing statements and any applicable Explanation of Benefits from other health insurance providers.
- Do ensure that the itemized billing statement includes the patient’s name, date of birth, and CHAMPVA identification number, alongside the provider’s information and service details.
- Don’t forget to report any existing other health insurance. This information is vital, as CHAMPVA acts as the secondary payer.
- Don’t submit claims after the one-year deadline. Claims must be received within a year of the service date or discharge date for inpatient care.
- Don’t skip the certification section. Sign and date it to validate that all information provided is accurate.
By adhering to these guidelines, you increase your chances of a smooth and successful claims process. Approaching your claim carefully can lead to timely processing and fewer complications.
Misconceptions
Misconceptions About the CHAMPVA Claim VA 10-7959A Form
- This form can be used by providers to submit claims. This is incorrect. The form is exclusively for patients, sponsors, or guardians to submit claims.
- Claims can be submitted at any time after the date of service. In reality, claims must be received within one year of the service date or the discharge date for inpatient care.
- Other health insurance (OHI) details are optional. OHI information is required by law, and must be reported for proper processing of claims.
- All claim forms can be submitted without additional documentation. Claims must be accompanied by itemized billing statements and OHI Explanation of Benefits (EOB) when applicable.
- It does not matter if the itemized statements are incomplete. The itemized statements must contain specific information including patient and provider details, dates of service, and itemized charges.
- A signature is not necessary when submitting the form. A signature is mandatory, certifying that the provided information is accurate and represents actual services rendered.
- Changes in eligibility do not need to be reported. Changes, such as divorce, must be reported to CHAMPVA immediately to maintain accurate eligibility records.
Key takeaways
When filling out the CHAMPVA Claim VA 10-7959A form, here are some essential points to keep in mind:
- This form must be completed by the patient, sponsor, or guardian for all beneficiary claims.
- The form is not applicable for provider-submitted claims.
- Attach the Explanation of Benefits (EOB) from other health insurance if applicable; ensure the dates and charges match the billing statements.
- Submissions should be made within one year of the service date or discharge date for inpatient care to avoid denial.
- A complete and itemized billing statement is mandatory; it must include patient information, provider details, and service itemization.
- Mandatory fields in Section I include the patient’s last name, first name, MI, and CHAMPVA Member Number.
- When providing information about other health insurance, be sure to include all relevant coverage details.
- Certification of the information provided is crucial, as false claims can have serious legal consequences.
Browse Other Templates
Proof of Identity - Understand that submitting false information on this form has legal consequences.
Money Order Refund Western Union - Use of authorized signatures for processing updates.
