Fill Out Your Chiropractic Treatment Plan Form
The Chiropractic Treatment Plan form serves as a crucial tool in outlining the details of a patient’s care within chiropractic practice. This form captures essential patient information, including their personal details, health history, and current conditions. It requires documentation of prior diagnoses along with corresponding ICD9 codes, ensuring a comprehensive record of treatment over the previous year. Providers are also asked to indicate the patient’s type—whether they are new to the office or established—but presenting with a new injury or ongoing care needs. Integral to formulating a treatment plan, clinicians must describe the etiology of the current condition and the primary complaint of the patient. The form assesses treatment progress by noting initial and current pain levels, along with the percentage of recovery achieved thus far. Moreover, it directly addresses whether the acute phase of treatment is complete and the level of patient compliance. By mandating clear, organized responses, this form facilitates effective communication between treating doctors and insurance providers and aims to ensure that all relevant information is available for determining coverage and authorization of future treatment. Those filling out the form must do so accurately, as incomplete submissions can lead to delays and denials of necessary care. In sum, the Chiropractic Treatment Plan form is not merely administrative; it is a foundational document that supports patient care while navigating the complexities of healthcare delivery.
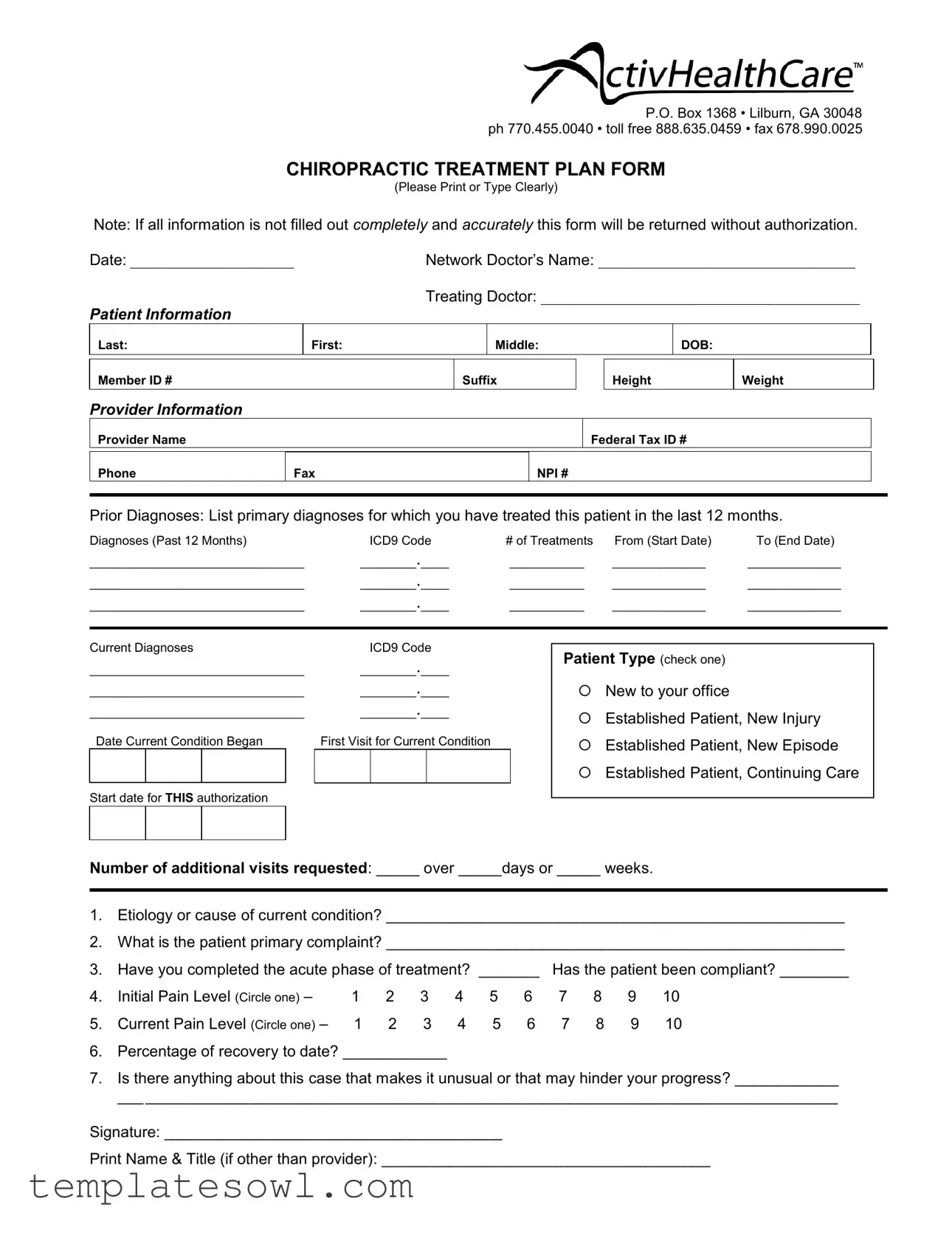
Chiropractic Treatment Plan Example
P.O. Box 1368 • Lilburn, GA 30048 ph 770.455.0040 • toll free 888.635.0459 • fax 678.990.0025
CHIROPRACTIC TREATMENT PLAN FORM
(Please Print or Type Clearly)
Note: If all information is not filled out completely and accurately this form will be returned without authorization.
Date: _____________________
PATIENT INFORMATION
Last:
Network Doctor’s Name: _________________________________
Treating Doctor: _________________________________________
First: |
Middle: |
DOB: |
|
|
|
Member ID #
Suffix
Height
Weight
PROVIDER INFORMATION
Provider Name
Federal Tax ID #
Phone
Fax
NPI #
Prior Diagnoses: List primary diagnoses for which you have treated this patient in the last 12 months.
Diagnoses (Past 12 Months) |
ICD9 Code |
# of Treatments |
From (Start Date) |
To (End Date) |
||||||
_______________________ |
______.___ |
________ |
__________ |
__________ |
||||||
_______________________ |
______.___ |
________ |
__________ |
__________ |
||||||
_______________________ |
______.___ |
________ |
__________ |
__________ |
||||||
|
|
|
|
|
|
|||||
Current Diagnoses |
ICD9 Code |
|
Patient Type (check one) |
|
||||||
_______________________ |
______.___ |
|
|
|||||||
|
|
|
|
|||||||
_______________________ |
______.___ |
|
New to your office |
|
||||||
_______________________ |
______.___ |
|
Established Patient, New Injury |
|||||||
|
|
|
|
|
|
|
|
|||
Date Current Condition Began |
First Visit for Current Condition |
|
Established Patient, New Episode |
|||||||
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
Established Patient, Continuing Care |
||
Start date for THIS authorization |
|
|
|
|
|
|
|
|||
|
|
|
|
|
||||||
Number of additional visits requested: _____ over _____days or _____ weeks. |
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
1.Etiology or cause of current condition? _____________________________________________________
2.What is the patient primary complaint? _____________________________________________________
3. |
Have you completed the acute phase of treatment? _______ |
Has the patient been compliant? ________ |
|||||||||
4. |
Initial Pain Level (Circle one) – |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
5. |
Current Pain Level (Circle one) – |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
6.Percentage of recovery to date? ____________
7.Is there anything about this case that makes it unusual or that may hinder your progress? ____________
___________________________________________________________________________________
Signature: _______________________________________
Print Name & Title (if other than provider): ______________________________________
Form Characteristics
| Fact Title | Description |
|---|---|
| Form Purpose | The Chiropractic Treatment Plan Form is used to provide essential information about a patient's treatment plan for authorization purposes. |
| Patient Information | It requires detailed patient information, including the patient’s last name, first name, date of birth, height, and weight. |
| Provider Details | Providers must include their name, Federal Tax ID number, phone, fax, and NPI number to ensure proper identification. |
| Prior Diagnoses | Providers are required to list primary diagnoses treated within the past 12 months, along with corresponding ICD9 Codes. |
| Current Diagnostics | Current diagnoses and ICD9 codes must be documented to clearly outline the patient's ongoing medical situation. |
| Patient Type | The form classifies patients based on their familiarity with the provider's office, distinguishing between new and established patients. |
| Treatment Duration | Providers can document the start and end dates of treatment along with the number of visits requested over a specified timeframe. |
| Compliance Check | The form includes questions regarding the patient's compliance with treatment and the completion of the acute phase. |
| Unique Case Notes | Providers can indicate any unusual circumstances that might impact treatment progress, ensuring comprehensive care. |
Guidelines on Utilizing Chiropractic Treatment Plan
The Chiropractic Treatment Plan form must be completed accurately to avoid delays in authorization. Follow these steps to ensure all necessary information is provided:
- Fill in the date.
- Enter patient information:
- Last Name
- First Name
- Middle Initial
- Date of Birth
- Member ID Number
- Suffix
- Height
- Weight
- Provide provider information:
- Provider Name
- Federal Tax ID Number
- Phone Number
- Fax Number
- NPI Number
- List prior diagnoses:
- Diagnoses from the past 12 months.
- ICD9 Code associated with each diagnosis.
- Number of treatments for each diagnosis.
- Start date and end date of treatment for each diagnosis.
- Enter current diagnoses:
- Current diagnoses with corresponding ICD9 Code.
- Select patient type (check one):
- New to your office
- Established Patient, New Injury
- Established Patient, New Episode
- Established Patient, Continuing Care
- Provide details on the current condition:
- Start date for THIS authorization.
- Number of additional visits requested over a specified period.
- Answer the following questions:
- Etiology or cause of current condition.
- Patient's primary complaint.
- Indicate if the acute phase of treatment is complete and if the patient has been compliant.
- Circle the initial pain level (1-10).
- Circle the current pain level (1-10).
- Percentage of recovery to date.
- Note any unusual case details that may hinder progress.
- Sign the form:
- Signature of provider.
- Print Name & Title (if different from provider).
Once completed, review the form for any missing information before submitting it for authorization. Accuracy will help speed up the process.
What You Should Know About This Form
What is the Chiropractic Treatment Plan form?
The Chiropractic Treatment Plan form is essential for documenting a patient's diagnosis, treatment plan, and progress in a chiropractic practice. It allows healthcare providers to outline the patient's care needs and ensures that insurance documentation is accurate and complete. By filling out this form, practitioners can secure the necessary authorizations for treatment from insurance providers.
Why is it important to fill out the form completely?
Completing the form fully and accurately is crucial, as any missing or incorrect information can lead to delays in treatment authorization. Insurers often require detailed documentation to process claims. If the form isn’t filled out completely, it will be returned without authorization, potentially hindering the patient's access to necessary care.
What information is required in the form?
The form requires several key pieces of information, including patient information (name, date of birth, etc.), provider details (name, tax ID number), diagnoses (both prior and current), the patient's treatment history, and specific treatment goals. This comprehensive data ensures that everyone involved in the patient's care has a clear understanding of their medical needs.
What is the significance of the ICD-9 codes listed on the form?
ICD-9 codes serve as standardized identifiers for diagnoses. They play an important role in billing and insurance claims, ensuring that treatments align with the correct medical conditions. These codes help communicate the reasons for treatment clearly, which is vital when working with insurance companies.
How does the form address ongoing treatment needs?
The Chiropractic Treatment Plan form specifically asks about the number of additional visits requested and the timeline for those visits. By detailing the patient's treatment plan, the provider can effectively communicate how many sessions are necessary and over what period, which is crucial for both patient care and insurance purposes.
What does the section about pain levels indicate?
This section allows the practitioner to assess the patient's progress. By noting the initial and current pain levels, healthcare providers can track improvements and adjust treatment as necessary. This information not only helps in creating an effective treatment plan but also provides evidence of progress to insurance providers.
How does the form facilitate communication between the provider and the patient?
The form promotes open dialogue by including questions about the patient's condition, compliance with treatment, and any unusual circumstances impacting recovery. This captures comprehensive information, which can help in tailoring the treatment plan and addressing any barriers a patient may face during recovery.
What happens if the patient is new to the office?
If the patient is new to the office, the practitioner will need to check the corresponding box on the form, allowing the provider to identify the patient's background and treatment history. This information is critical for determining the most appropriate treatment strategy and ensuring continuity of care, particularly for new patients with no prior records.
Can the form be modified for different patients?
While the structure of the Chiropractic Treatment Plan form remains generally consistent, certain sections can be tailored based on individual patient needs. This adaptability helps ensure that the treatment plan is personalized while still adhering to insurance and documentation requirements.
Common mistakes
Completing a Chiropractic Treatment Plan form is a critical step in ensuring that patients receive the appropriate care. However, mistakes can happen during this process. A common error is not filling out all required fields. Each section of the form is designed to gather essential information. Leaving any portion blank can lead to delays, as the submission will often be returned for completion.
Another frequent issue is the use of unclear handwriting or illegible typing. This can create misunderstandings regarding the patient's information, diagnosis, or treatment plan. Clarity is vital. Hence, taking extra time to ensure that entries are easy to read can save time and prevent future errors.
Additionally, confusion about medical codes can be problematic. The ICD9 codes are critical for identifying diagnoses correctly. Using inaccurate or outdated codes may impact claims processing. It is important to verify the codes and ensure they are current, as mistakes in this area can lead to reimbursement issues. Understanding this can significantly enhance the efficiency of the treatment plan submission.
Lastly, failing to keep records of prior treatments can lead to incomplete information being submitted. Insurance companies and healthcare providers often need a full history of the patient’s care. Listing out previous treatments and their outcomes is essential. This not only helps in justifying current treatment plans but also supports a seamless continuity of care.
Documents used along the form
When a healthcare provider develops a Chiropractic Treatment Plan, several other forms and documents may need to accompany it to ensure comprehensive patient care and compliance with regulations. Below are some of the commonly used documents related to chiropractic treatment.
- Patient Consent Form: This document ensures that the patient is informed about the treatment they will receive. It covers the nature of the proposed treatment, potential risks, and alternative options, allowing the patient to give their informed consent.
- Insurance Authorization Form: This form is essential for obtaining approval from health insurance providers before starting treatment. It includes patient details, treatment codes, and the specifics of the proposed plan to seek verification of benefits.
- Initial Evaluation Form: This form is filled out during the first patient visit. It provides detailed information on the patient's medical history, current symptoms, and any prior treatments received. This evaluation aids in creating a tailored treatment plan.
- Progress Notes: These are ongoing records that document each treatment session. Progress notes help track improvements or setbacks in the patient's condition and are critical for adjusting the treatment plan if necessary.
- Financial Agreement: This document outlines the financial responsibilities of the patient, including payment structures, costs, and any agreements related to insurance claims. It ensures that both parties understand the financial aspects of the treatment.
- Discharge Summary: At the end of the treatment, a discharge summary is prepared. It summarizes the patient's progress, final assessment, and recommendations for ongoing care or referrals to other specialists if needed.
These forms work together to support the chiropractic treatment process and help ensure that both the patient and provider have a clear understanding of the treatment goals, financial responsibilities, and medical history. Maintaining well-organized documentation enhances the overall quality of care and compliance with healthcare standards.
Similar forms
-
Medical History Form: This document collects essential information about a patient's past and current medical conditions. Like the Chiropractic Treatment Plan, it requires accurate information to ensure proper care and treatment. Both forms emphasize patient details and prior treatments to create a comprehensive care plan.
-
Informed Consent Form: This form outlines the risks and benefits associated with specific treatments. Similar to the Chiropractic Treatment Plan, it underscores the importance of clear communication between the provider and the patient. Both documents seek to protect the patient's rights while ensuring they understand their treatment options.
-
Progress Note: Progress notes track a patient’s development over time. These notes detail the effectiveness of ongoing treatments, just like the Chiropractic Treatment Plan tracks the progress following specific therapies. Both forms help healthcare providers assess treatment outcomes and adjust plans as needed.
-
Referral Form: A referral form is used when a healthcare provider needs to send a patient to a specialist. It shares similar elements with the Chiropractic Treatment Plan, as both require detailed information about the patient’s condition and treatment history. This helps ensure continuity of care and effective communication among providers.
Dos and Don'ts
When filling out the Chiropractic Treatment Plan form, attention to detail is crucial. Here are ten key practices to keep in mind:
- Do print or type clearly to ensure legibility.
- Do provide all required patient information, including full name, date of birth, and member ID.
- Do accurately list prior and current diagnoses with their respective ICD9 codes.
- Do specify the start and end dates for treatments to maintain a clear treatment history.
- Do indicate whether the patient is new or established, and provide details on their current condition.
- Don't leave any sections of the form blank; incomplete forms may be returned.
- Don't use vague descriptions; be as specific as possible regarding the patient's condition.
- Don't forget to sign the form; an illegible or missing signature will delay the authorization process.
- Don't overlook the patient's compliance; it is critical to note if they have adhered to the treatment plan.
- Don't misrepresent any information; accuracy maintains the integrity of the treatment plan.
Misconceptions
Here are four common misconceptions regarding the Chiropractic Treatment Plan form:
- The form is not essential for treatment. Some people believe that filling out this form is optional. However, it’s crucial for clearly documenting the patient's information and treatment plan. If not completed accurately, it may delay treatment authorization.
- Only basic details are needed. Many think that only minimal information is required. In reality, comprehensive details about the patient's condition, treatment history, and current complaints are necessary for proper assessment and planning.
- The form is only for new patients. This misconception leads some to dismiss the form if they are established patients. However, even ongoing care requires updates in the treatment plan to reflect current conditions and progress.
- Once submitted, the form won’t be reviewed again. Some might assume that after submission, no further input is needed. In fact, the form may undergo multiple reviews, and updates can be necessary as treatment progresses and patient needs change.
Key takeaways
When filling out the Chiropractic Treatment Plan form, there are several important considerations to keep in mind. Following these guidelines can enhance clarity and improve the authorization process.
- Complete Information is Crucial: All sections of the form must be filled out completely. Incomplete forms will be returned for additional information, delaying treatment approval.
- Accurate Diagnoses: Clearly list prior and current diagnoses, along with corresponding ICD9 codes. This ensures that the insurance company understands the patient's history and treatment needs.
- Patient Type Matters: Specify whether the patient is new to the office, has a new injury, is a new episode, or is continuing care. This classification plays a vital role in determining the treatment plan and insurance reimbursement.
- Pain Levels are Key: Accurately record both the initial and current pain levels. This quantifiable data can indicate the effectiveness of treatments and guide ongoing care.
- Compliance with Treatment: Indicate whether the patient has adhered to the treatment plan. This information can influence future care decisions and insurance considerations.
- Unusual Circumstances: If any factors could affect the patient's recovery, document them. Highlighting these can prepare the treating team for potential challenges in the patient’s progress.
Following these takeaways can lead to a more streamlined process for submitting the Chiropractic Treatment Plan and ensure the patient receives the necessary care without unnecessary delays.
Browse Other Templates
Retirement Forms - Withdrawal of funds not entitled to you has implications you must acknowledge.
Letter to School for Absence of Child - Aids in managing school attendance policies effectively.
Explain Biomedical Waste Management - It specifies where to keep records of training logs and certificates for compliance checks.