Fill Out Your Cigna Appeal Form
Navigating health insurance can often feel overwhelming, especially when faced with an adverse decision regarding coverage. The Cigna Appeal form provides a structured way to address these challenges. This form serves as your official request to reassess a previous decision by Cigna that denied or reduced benefits. Whether you or a designated representative—like a physician—are filing the appeal, understanding the process can significantly impact the outcome. The first step involves reaching out to Cigna’s Customer Service Department, where representatives can provide immediate assistance and may even resolve the issue without requiring a formal appeal. If that doesn’t work, Step Two entails completing the appeal form and submitting it alongside any supporting documentation to the designated address. Timeliness is crucial; most appeals should be submitted within 180 days, while your specific plan may allow for a longer timeline. Essential information, such as participant details and the nature of the denial, needs to be included to streamline the process. A comprehensive submission will facilitate a prompt review by Cigna's team, leading to a decision conveyed in writing. With the right preparation and understanding of the requirements, individuals can advocate more effectively for their healthcare needs.
Cigna Appeal Example
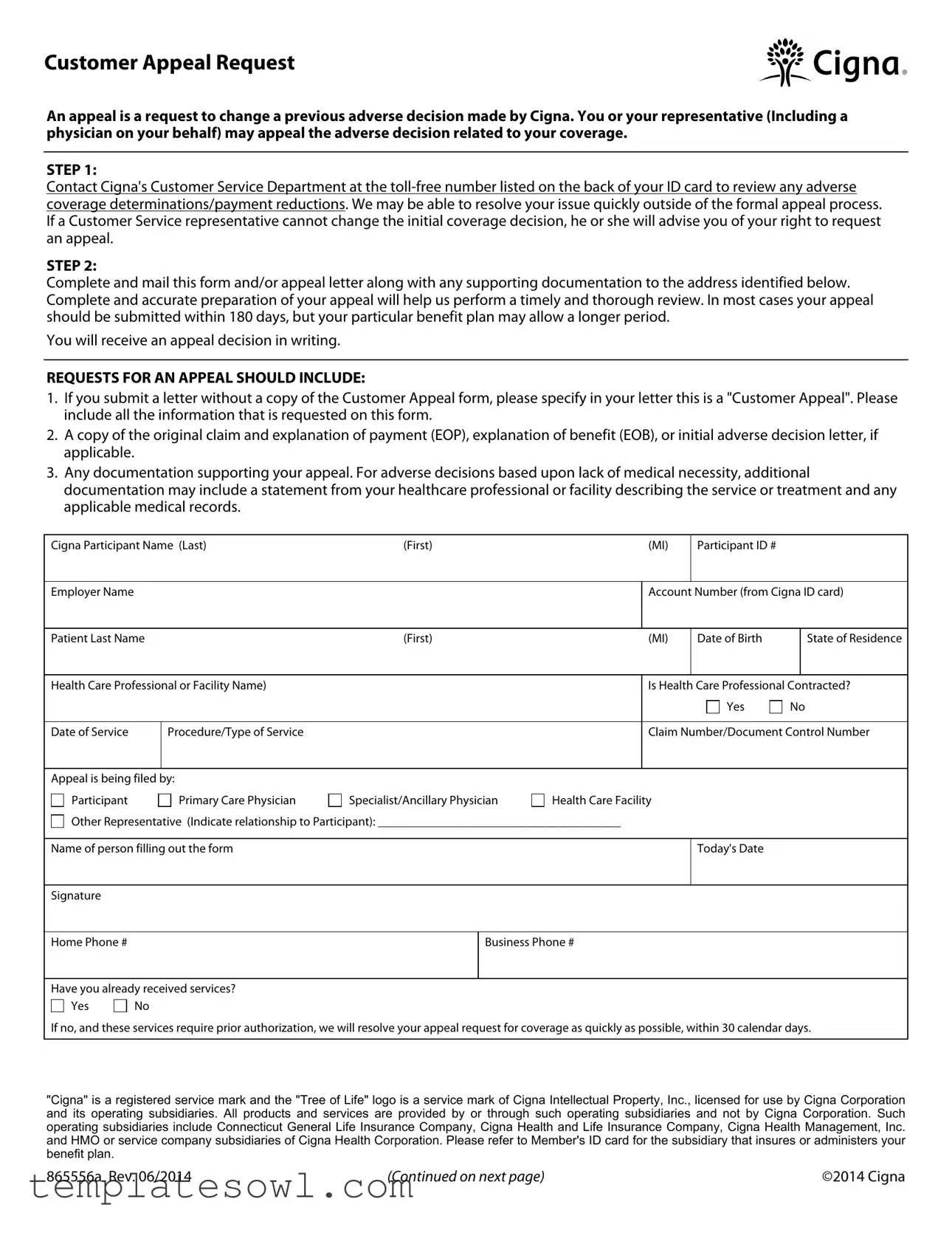
Customer Appeal Request
An appeal is a request to change a previous adverse decision made by Cigna. You or your representative (Including a physician on your behalf) may appeal the adverse decision related to your coverage.
STEP 1:
Contact Cigna's Customer Service Department at the
STEP 2:
Complete and mail this form and/or appeal letter along with any supporting documentation to the address identified below. Complete and accurate preparation of your appeal will help us perform a timely and thorough review. In most cases your appeal should be submitted within 180 days, but your particular benefit plan may allow a longer period.
You will receive an appeal decision in writing.
REQUESTS FOR AN APPEAL SHOULD INCLUDE:
1.If you submit a letter without a copy of the Customer Appeal form, please specify in your letter this is a "Customer Appeal". Please include all the information that is requested on this form.
2.A copy of the original claim and explanation of payment (EOP), explanation of benefit (EOB), or initial adverse decision letter, if applicable.
3.Any documentation supporting your appeal. For adverse decisions based upon lack of medical necessity, additional documentation may include a statement from your healthcare professional or facility describing the service or treatment and any applicable medical records.
Cigna Participant Name (Last) |
|
(First) |
|
|
(MI) |
Participant ID # |
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Employer Name |
|
|
|
|
|
|
|
|
|
Account Number (from Cigna ID card) |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
Patient Last Name |
|
(First) |
|
|
(MI) |
Date of Birth |
|
State of Residence |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Health Care Professional or Facility Name) |
|
|
|
|
|
Is Health Care Professional Contracted? |
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date of Service |
|
|
Procedure/Type of Service |
|
|
|
|
|
Claim Number/Document Control Number |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Appeal is being filed by: |
|
|
|
|
|
|
|
|
|
||||||||
|
|
Participant |
|
|
|
Primary Care Physician |
|
Specialist/Ancillary Physician |
|
Health Care Facility |
|
|
|
||||
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
Other Representative (Indicate relationship to Participant): _______________________________________ |
|
|
|
||||||||||||
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
||||||
Name of person filling out the form |
|
|
|
|
|
|
Today's Date |
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
Signature |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
Home Phone # |
|
|
|
|
|
|
Business Phone # |
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
||||||
Have you already received services? |
|
|
|
|
|
|
|
|
|
||||||||
|
|
Yes |
|
|
No |
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
||||||
If no, and these services require prior authorization, we will resolve your appeal request for coverage as quickly as possible, within 30 calendar days.
"Cigna" is a registered service mark and the "Tree of Life" logo is a service mark of Cigna Intellectual Property, Inc., licensed for use by Cigna Corporation and its operating subsidiaries. All products and services are provided by or through such operating subsidiaries and not by Cigna Corporation. Such operating subsidiaries include Connecticut General Life Insurance Company, Cigna Health and Life Insurance Company, Cigna Health Management, Inc. and HMO or service company subsidiaries of Cigna Health Corporation. Please refer to Member's ID card for the subsidiary that insures or administers your benefit plan.
865556a Rev. 06/2014 |
(Continued on next page) |
©2014 Cigna |
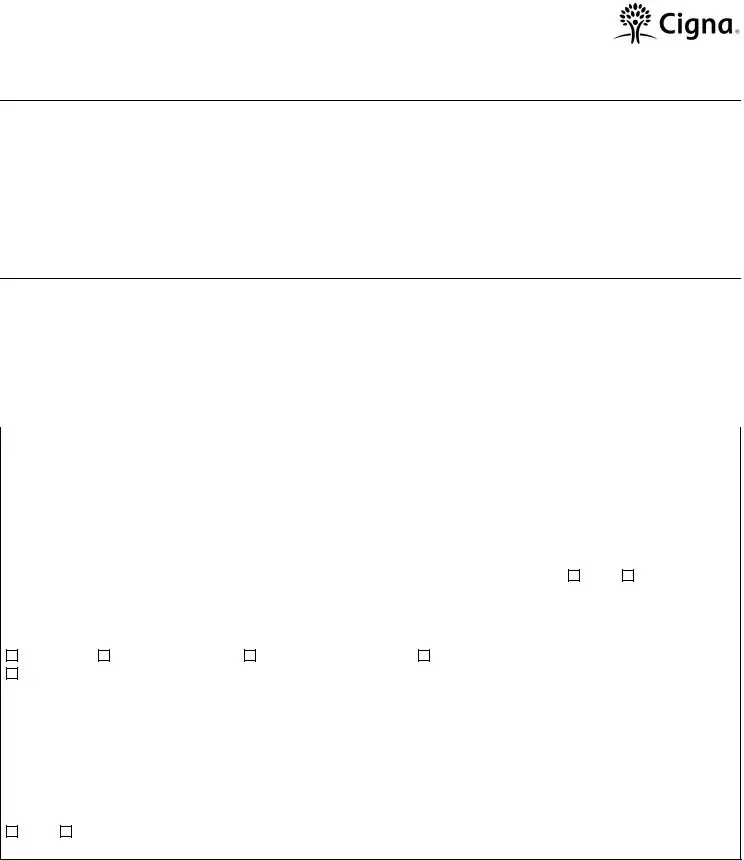
If allowed by your Plan, is this a second appeal or external review request? |
Yes |
No |
Please check off the selection that best describes your appeal:

 Request for
Request for

 Coverage Exclusion or Limitation
Coverage Exclusion or Limitation

 Maximum Reimbursable Amount
Maximum Reimbursable Amount

 Inpatient Facility Denial (Level of Care, Length of Stay)
Inpatient Facility Denial (Level of Care, Length of Stay)

 Mutually Exclusive, Incidental procedure code denials
Mutually Exclusive, Incidental procedure code denials

 Additional reimbursement to your out of network health care professional for a procedure code modifier
Additional reimbursement to your out of network health care professional for a procedure code modifier

 Experimental/Investigational Procedure
Experimental/Investigational Procedure

 Medical Necessity
Medical Necessity

 Timely Claim Filing (without proof)
Timely Claim Filing (without proof)

 Benefits reduced due to
Benefits reduced due to
Reason why you believe the adverse coverage decision was incorrect and what you feel the expected outcome should be. As a reminder, please attach any supporting documentation (for medical
Additional Comments:
Refer to your ID card to determine the appeal address to use below.
Mail the completed Appeal Request Form or Appeal Letter along with all supporting documentation to the address below:
If the ID card indicates: Cigna Network |
If the ID card indicates: GW - Cigna Network |
Cigna Appeals Unit |
Cigna Appeals Unit |
P.O. Box 188011 |
P.O. Box 188062 |
Chattanooga, TN |
Chattanooga, TN |
IMPORTANT: This address is intended only for appeals of coverage denials. Any other requests sent to this address will be forwarded to the appropriate Cigna location, which may result in a delay in handling your request or processing your claim.
865556a Rev. 06/2014
Clear Form
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of the Appeal | The Cigna Appeal form is used to request a review and potential reversal of a previous adverse decision made by Cigna regarding coverage or payment issues. |
| Submission Timeframe | Typically, appeals should be submitted within 180 days from the date of the initial adverse decision, although specific plans may allow for a longer period. |
| Required Documentation | To file an appeal, submit this form along with any necessary supporting documents, such as the original claim and explanation of payment or a letter addressing the adverse decision. |
| Communication with Cigna | Before formally appealing, it's advisable to contact Cigna's Customer Service to discuss the adverse decision. Often, issues may be resolved over the phone without needing to file a formal appeal. |
| State-Specific Regulations | In certain states, specific laws may apply to the appeal process. For example, Texas laws may establish different guidelines regarding the appeal timeframe and documentation requirements. |
Guidelines on Utilizing Cigna Appeal
Once you've taken the necessary steps to understand your situation, it's time to fill out the Cigna Appeal form. Completing this form accurately will help ensure that your appeal is processed swiftly. After submitting the appeal, you can expect to receive a decision in writing, allowing you to understand the outcome of your request.
- Contact Cigna's Customer Service Department using the toll-free number on the back of your ID card. This will allow you to discuss the adverse decision and see if it can be resolved without the appeal process.
- If you need to proceed with filing an appeal, download and print the appeal form.
- Fill out your personal information, including your name, participant ID number, employer name, and any other relevant details about the patient and healthcare professional.
- Clearly indicate if you are the participant or if someone else is filing the appeal on your behalf.
- Specify the reason for your appeal by checking the appropriate box on the form.
- Provide a detailed explanation of why you believe the adverse decision was incorrect. Be specific about the expected outcome.
- Gather and attach all necessary supporting documents, including the original claim, explanation of payment, and any medical records that support your case.
- Check the appeal address on your ID card and mail the completed form along with all supporting documentation to the correct address.
- Keep a copy of the appeal form and all documents for your records before mailing them.
What You Should Know About This Form
What is the Cigna Appeal form used for?
The Cigna Appeal form is used to formally request a review of a previous decision made by Cigna regarding your coverage. You or your representative can use this form to appeal decisions that affect your health care benefits. This may include denials of coverage or payment reductions.
How do I start the appeal process with Cigna?
First, contact Cigna's Customer Service Department using the toll-free number on the back of your ID card. Discuss the adverse coverage determination with a representative. In some cases, issues can be resolved quickly without needing to file a formal appeal. If the representative cannot alter the initial decision, they will inform you about your right to appeal.
What information must be included when I submit the appeal request?
Your appeal should include several key elements: 1. If you submit a letter, indicate that it is a "Customer Appeal." Include all requested information from the appeal form. 2. Attach a copy of your original claim and any related documents, such as an explanation of payment (EOP) or initial adverse decision letter. 3. Provide supporting documentation for your appeal, especially for decisions made due to lack of medical necessity. Include statements from health care professionals and relevant medical records if applicable.
What happens after I submit my appeal?
Once you submit your appeal, Cigna will conduct a thorough review. You can expect a written decision from them, typically within a set time frame. For most claims, the appeal must be submitted within 180 days, although some plans may allow longer periods. Ensure that all documentation is complete and accurate to avoid delays in processing.
Where should I send my completed Cigna Appeal form?
Mail the completed form, along with your appeal letter and supporting documents, to the address specified on your ID card. If your card identifies the Cigna Network, send it to Cigna Appeals Unit, P.O. Box 188011, Chattanooga, TN 37422-8011. If it indicates GW - Cigna Network, use P.O. Box 188062, Chattanooga, TN 37422-8062. This address is strictly for appeal requests, and other inquiries may lead to delays.
Common mistakes
Filling out the Cigna Appeal form requires attention to detail. Many individuals make mistakes that can delay their appeal or even lead to a denial. A common error is forgetting to include the Customer Appeal form itself when submitting a letter. Even if you provide all necessary information in that letter, without specifying it as a "Customer Appeal," processing can stall. Always ensure your documentation is complete.
Another frequent mistake involves failing to include supporting documentation. When your appeal concerns a denial due to lack of medical necessity, additional evidence is crucial. This could include a statement from a healthcare professional or relevant medical records. Submitting your appeal without this documentation weakens your position and may lead to an unfavorable outcome.
The timeframe for submitting your appeal also poses challenges. Many people overlook the requirement to submit their appeal within 180 days of the initial claim’s decision. While some benefit plans allow longer timeframes, ignorance of the deadline can result in losing the right to appeal. Always check the terms of your benefit plan to ensure compliance.
Using the wrong appeal address is another significant mistake. The appeal address must match the information on your ID card. If you send your appeal to the incorrect address, it will get forwarded, causing unnecessary delays. Take a moment to verify and write down the correct address before mailing your appeal.
Finally, some individuals do not fully articulate their reasons for believing that the coverage decision was incorrect. The section requesting your rationale is critical. Provide clear, detailed explanations, including the expected outcomes. A poorly explained appeal can lack the persuasion needed to influence the final decision, ultimately resulting in rejection. Take this opportunity seriously; detail matters.
Documents used along the form
When filing an appeal with Cigna concerning a denial of benefits, several other documents may be necessary to support your request. Each of these documents plays a vital role in presenting your case effectively and ensuring that all relevant information is considered. Below is a list of important forms and documents that are commonly required alongside the Cigna Appeal form.
- Original Claim Form: This document provides the details of the services or treatments that were billed to Cigna. Including it helps clarify the basis of the initial coverage decision.
- Explanation of Benefits (EOB): The EOB outlines how the claim was processed, including details on payment amounts, denials, or reductions. This provides context for your appeal.
- Adverse Decision Letter: If Cigna has formally notified you of a denied claim, this letter summarizes the reasons for the denial and is essential for your appeal.
- Medical Records: Depending on the reason for denial, relevant medical records may be needed to demonstrate the medical necessity of the services provided. These records come from your healthcare provider.
- Physician Statement: A supporting statement from your healthcare professional can clarify the necessity of the service or treatment, supporting your claim that it should be covered.
- Additional Documentation: This might include any other records, letters, or documents that can bolster your argument, including photos or notes from consultations.
- Previous Appeals: If applicable, including copies of any prior appeal submissions may be helpful to show the history of your efforts to resolve the issue.
Understanding what documents to include can significantly enhance your appeal’s likelihood of success. Always make sure to send complete and accurate information to Cigna to facilitate a thorough review.
Similar forms
-
Claim Denial Letter: Similar to the Cigna Appeal form, this letter outlines the reasons for denying a claim. It allows the recipient to understand the decision and provides grounds for a potential appeal, just like the appeal form prompts you to specify reasons for disputing a coverage decision.
-
Pre-Authorization Request: This document is used to seek approval for specific medical services before they are provided. Like the appeal form, it requires detailed information about the patient, the proposed treatment, and supporting documentation to justify the request.
-
Grievance Form: A grievance form allows individuals to formally express dissatisfaction with a service or decision by Cigna. It shares similarities with the appeal form as both involve submitting information and potentially require supporting documentation to substantiate claims.
-
Request for External Review: This document is filed when a participant believes that a coverage denial should be reviewed by an independent entity. It serves a similar purpose to the Cigna Appeal form, providing a structured way to challenge a denial and requiring specific information to support the case.
Dos and Don'ts
When you are filling out the Cigna Appeal form, there are specific actions that can help streamline the process, as well as some common pitfalls to avoid. Here are four important dos and don'ts to consider:
- Do read the instructions carefully before starting the appeal. Understanding the entire process will help ensure that your appeal is complete.
- Don’t submit your appeal without all required documentation. Missing paperwork can delay your appeal significantly.
- Do provide detailed information about why you believe the previous decision was incorrect. Clarity can strengthen your case.
- Don’t delay in submitting your appeal. Most appeals should be submitted within 180 days to avoid complications with your benefit plan.
Misconceptions
Understanding the Cigna Appeal form is crucial for navigating the appeal process effectively. However, several misconceptions can hinder your efforts. Here are four common misunderstandings:
- Filing an appeal is unnecessary after speaking with customer service. Many individuals assume that if they contact customer service and receive no immediate solution, an appeal is pointless. In reality, customer service representatives may have limited authority. Following up with a formal appeal could lead to different outcomes.
- It’s sufficient to send in just the appeal letter. Some people believe a letter alone suffices for an appeal. However, Cigna requires the completion of the official Customer Appeal form along with any relevant documentation to ensure a thorough review of your case.
- You have an unlimited time to submit your appeal. A common error is thinking there are no deadlines. Most appeals need to be submitted within 180 days of the initial adverse decision. Some benefit plans may allow longer periods, but it's essential to verify this to avoid missed deadlines.
- Supporting documentation is optional. Individuals often think that documentation supporting their appeal isn’t critical. This is a misconception. Including all relevant documents, especially medical records or statements from healthcare professionals, strengthens your case significantly.
Being aware of these misconceptions can assist in preparing a stronger appeal. Each detail matters when seeking a review of an adverse decision.
Key takeaways
When filling out the Cigna Appeal form, keep these key takeaways in mind:
- Understand the appeal process: An appeal is your request to change a previous decision made by Cigna regarding your coverage. You or your representative can initiate this process.
- Be thorough and accurate: Complete the appeal form and include any necessary supporting documentation. This will ensure a timely review and improve your chances of a favorable outcome.
- Time is important: Submit your appeal within 180 days, unless your plan specifies a different timeline. Delays could jeopardize your request.
- Use the correct address: Send your completed form and documentation to the appropriate Cigna appeals address listed on your ID card, as other requests mailed there may cause delays.
Browse Other Templates
Passport Renewal Process - If the applicant has ever changed names, include former names in full.
Texas Women's Health Benefits Application,Women's Health Program Enrollment Form,Texas Health Coverage Application,Texas Women's Health Assistance Form,Health Benefits Application for Women,Women’s Health Services Registration Form,Texas Family Plann - You are encouraged to report any discrimination experienced during the process.