Fill Out Your Cigna Prior Auth Form
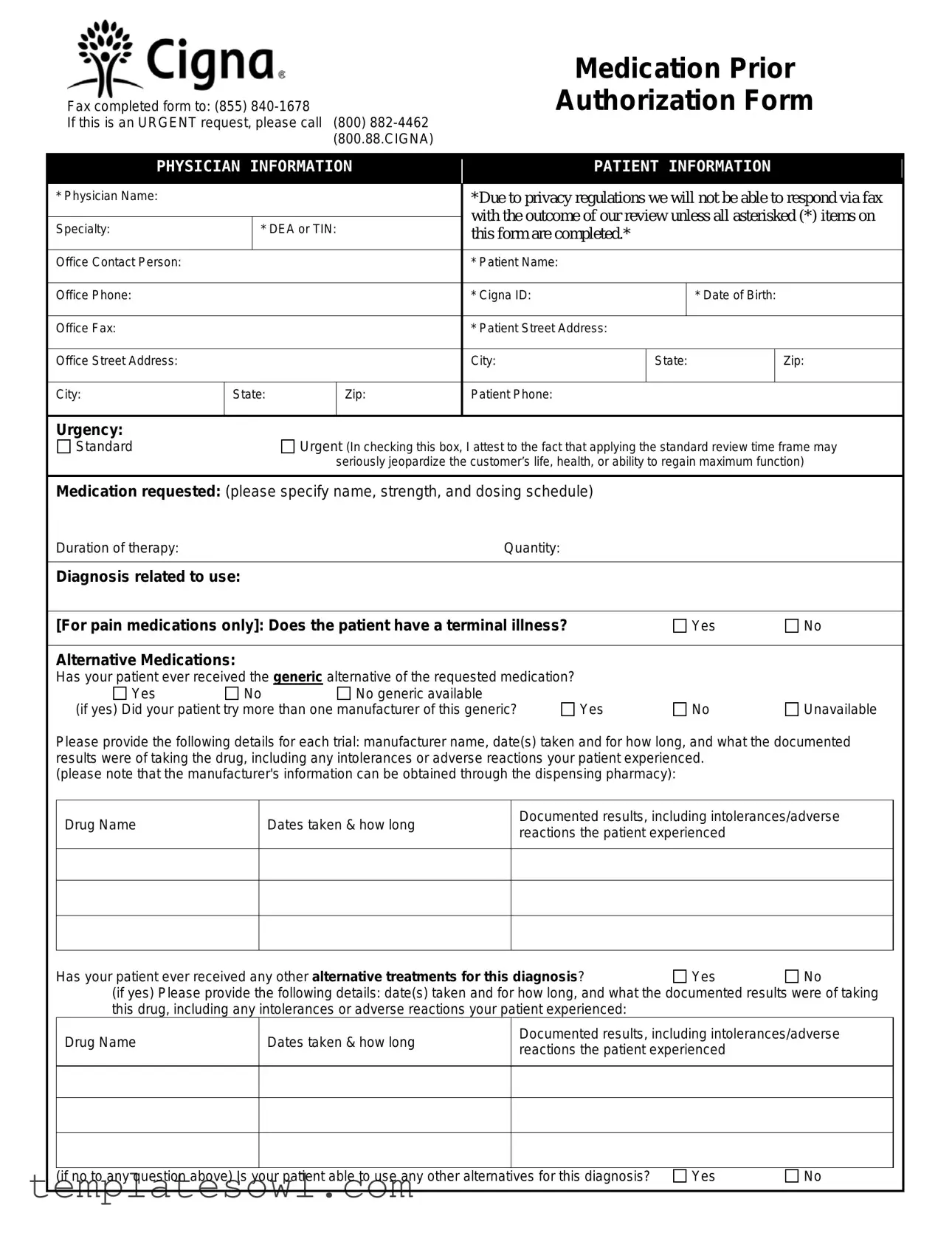
The Cigna Prior Authorization form is a critical tool for healthcare providers seeking approval for specific medications. It streamlines the process of reviewing medication requests, ensuring that patients receive the necessary treatments in a timely manner. The form requires essential information about both the physician and patient, such as names, contact details, and insurance identification. The urgency of the request can be indicated, allowing for faster processing when time is of the essence. In addition to basic details, the form captures vital clinical information, including the requested medication's name, dosage, duration of therapy, and the patient’s relevant medical history, including past treatments and adverse reactions. Furthermore, the form includes queries about alternative medications tried, documenting the outcomes of those trials. This thorough approach not only assists in expedited approvals but also protects patient privacy, as certain sections are marked with privacy regulations. For urgent requests, direct contact options are available, emphasizing the importance of timely communication in healthcare. The form can be submitted online for an even quicker response, enhancing efficiency for medical staff and better serving patient needs.
Cigna Prior Auth Example
Fax completed form to: (855)
If this is an URGENT request, please call (800)
Medication Prior
Authorization Form
|
|
PHYSICIAN INFORMATION |
|
|
PATIENT INFORMATION |
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
* Physician Name: |
|
|
|
|
|
*Due to privacy regulations we will not be able to respond via fax |
|
|||||
|
|
|
|
|
|
|
|
with the outcome of our review unless all asterisked (*) items on |
|
|||||
|
|
Specialty: |
|
* DEA or TIN: |
|
|
|
|||||||
|
|
|
|
|
this form are completed.* |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Office Contact Person: |
|
|
|
|
|
* Patient Name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Office Phone: |
|
|
|
|
|
* Cigna ID: |
|
|
* Date of Birth: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Office Fax: |
|
|
|
|
|
* Patient Street Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Office Street Address: |
|
|
|
|
|
City: |
|
State: |
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
City: |
State: |
|
Zip: |
|
Patient Phone: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Urgency: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Standard |
|
Urgent (In checking this box, I attest to the fact that applying the standard review time frame may |
|
|||||||||
|
|
|
|
|
seriously jeopardize the customer’s life, health, or ability to regain maximum function) |
|
||||||||
|
|
|
|
|
|
|
|
|||||||
|
|
Medication requested: (please specify name, strength, and dosing schedule) |
|
|
|
|
|
|||||||
|
|
Duration of therapy: |
|
|
|
|
|
Quantity: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
Diagnosis related to use: |
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|||||||
|
|
[For pain medications only]: Does the patient have a terminal illness? |
|
|
Yes |
No |
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
Alternative Medications: |
|
|
|
|
|
|
|
|
|
|||
|
|
Has your patient ever received the generic alternative of the requested medication? |
|
|
|
|
|
|
||||||
|
|
Yes |
No |
No generic available |
|
|
|
|
|
|
||||
|
|
(if yes) Did your patient try more than one manufacturer of this generic? |
Yes |
|
No |
Unavailable |
|
|||||||
Please provide the following details for each trial: manufacturer name, date(s) taken and for how long, and what the documented results were of taking the drug, including any intolerances or adverse reactions your patient experienced.
(please note that the manufacturer's information can be obtained through the dispensing pharmacy):
Drug Name |
Dates taken & how long |
Documented results, including intolerances/adverse |
||
reactions the patient experienced |
|
|||
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Has your patient ever received any other alternative treatments for this diagnosis? |
Yes |
No |
||
(if yes) Please provide the following details: date(s) taken and for how long, and what the documented results were of taking |
||||
this drug, including any intolerances or adverse reactions your patient experienced: |
|
|
||
Drug Name |
Dates taken & how long |
Documented results, including intolerances/adverse |
||
reactions the patient experienced |
|
|||
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(if no to any question above) Is your patient able to use any other alternatives for this diagnosis? |
Yes |
No |
||
(if no) Please provide the reason(s) why your patient is unable to use the available alternative(s):
Additional pertinent information: (please include other clinical reasons for drug, relevant lab values, etc.)
Save Time! Submit Online at:
Our standard response time for prescription drug coverage requests is 5 business days. If your request is urgent, it is important that
you call us to expedite the request. View our Prescription Drug List and Coverage Policies online at cigna.com.
v091619
“Cigna" is a registered service mark, and the “Tree of Life” logo is a service mark, of Cigna Intellectual Property, Inc., licensed for use by Cigna Corporation and its operating subsidiaries. All products and services are provided by or through such operating subsidiaries and not by Cigna Corporation. Such operating subsidiaries include, for example, Cigna Health and Life Insurance Company and Cigna Health Management, Inc. Address: Cigna Pharmacy Services, PO Box 42005,
Phoenix AZ
Form Characteristics
| Fact Name | Description |
|---|---|
| Submission Method | Complete and fax the form to (855) 840-1678 for processing. |
| Urgent Requests | If the request is urgent, call (800) 882-4462 to expedite the review process. |
| Response Time | The standard response time for requests is 5 business days, unless marked as urgent. |
| Privacy Compliance | All asterisked items on the form must be completed to receive outcomes via fax, ensuring privacy compliance. |
Guidelines on Utilizing Cigna Prior Auth
Completing the Cigna Prior Authorization form can feel daunting, but taking it step by step will simplify the process. Once this form is correctly filled out, you will be able to submit it and await a response from Cigna regarding the authorization of the requested medication.
- Start by filling in the Physician Information section. Include your name, specialty, DEA or TIN, and contact details such as the office phone and fax numbers.
- Proceed to the Patient Information section. Here, enter the patient's name, Cigna ID, date of birth, phone number, street address, city, state, and zip code.
- Indicate the urgency of the request by checking either "Standard" or "Urgent." If you're marking it as urgent, confirm that the standard review time may endanger the patient's health.
- For the medication requested, specify the name, strength, and dosing schedule of the medication.
- Complete the duration of therapy and the quantity needed.
- For the diagnosis related to the use of the medication, provide the relevant diagnosis.
- Answer whether the patient has a terminal illness by selecting "Yes" or "No."
- In the Alternative Medications section, indicate if the patient has tried the generic version of the requested medication. Check "Yes," "No," or "No generic available." If the answer is yes, provide detailed information about any trials of the generic medication.
- Next, address any other alternative treatments the patient might have received. Specify the names of the drugs, dates taken, duration, and documented results.
- If relevant, state whether the patient is able to use any other alternatives for the diagnosis. If the answer is no, provide reasons for this decision.
- Lastly, add any additional pertinent information that may help with the review, including clinical reasons for the drug request and relevant lab values.
Once the form is filled out completely, fax it to (855) 840-1678. If urgent, call (800) 882-4462 to expedite the request. Keep in mind that the average response time is five business days, but urgent requests may receive faster attention.
What You Should Know About This Form
What is the Cigna Prior Authorization form used for?
The Cigna Prior Authorization form is required to obtain approval for certain medications before they can be covered by Cigna insurance. This process helps ensure that prescribed medications are necessary and appropriate for the patient’s treatment plan.
How do I submit the Cigna Prior Authorization form?
You can submit the completed Cigna Prior Authorization form by faxing it to (855) 840-1678. For urgent requests, it is recommended that you call (800) 882-4462 for immediate assistance.
What information is needed to complete the form?
The form requires specific information such as physician and patient details, medication requested, the duration of therapy, alternative medications, and any historical treatment information. All fields marked with an asterisk (*) must be filled out to ensure a timely response.
What should I do if my request is urgent?
If your request qualifies as urgent, check the appropriate box on the form to indicate its urgency. Additionally, make sure to call (800) 882-4462 to expedite the review process, as standard submissions can take up to 5 business days.
Can I submit the Prior Authorization form online?
Yes, you can save time by submitting the form online at www.covermymeds.com. Another option is to submit it via SureScripts in your Electronic Health Record (EHR) system. Both methods can help streamline the process.
What is the expected response time for a standard request?
The typical response time for prescription drug coverage requests is up to 5 business days. If your request is urgent, you should call to expedite the response.
What if my patient has previously tried other alternatives?
If your patient has previously tried alternative medications or treatments, detailed information must be provided. This includes the names of the drugs, dates taken, duration, and any documented results or adverse reactions experienced.
Is it necessary to provide alternative medication details?
Yes, detailing any alternative medications attempted by the patient is crucial. This information helps justify the need for the requested medication. Include specific results and any intolerances to support your request.
Where can I find Cigna’s Prescription Drug List and Coverage Policies?
You can view Cigna's Prescription Drug List and corresponding coverage policies on their official website at cigna.com. This resource can assist in understanding what medications are covered under the insurance plan.
Common mistakes
Filling out the Cigna Prior Authorization form requires attention to detail. One common mistake is leaving out required fields. For instance, the form has several fields marked with an asterisk (*) that are mandatory. If any of these fields are incomplete, Cigna will not respond via fax with the outcome of the review. Such oversights can delay the approval process significantly.
Another frequent error is failing to provide adequate information about alternative medications. The form asks whether the patient has tried generic alternatives or other treatments. Incomplete responses can lead to unnecessary delays, as Cigna requires comprehensive documentation of any previous trials, including details like the manufacturer name and the outcomes of those trials. Without this information, claims may be rejected or delayed.
Some individuals erroneously check the "urgent" box without considering the implications. Marking a request as urgent means that it is critical for the patient's wellbeing. However, if the situation does not genuinely warrant urgent treatment, this misclassification may strain resources and lead to reputational penalties or less timely care for those with true urgent needs.
Additionally, not including relevant clinical information can hinder the approval process. The form provides a section for additional pertinent information, which could be crucial in justifying the need for the medication. This can include recent lab values or unique clinical circumstances that support the request. Omitting such details may prevent Cigna from fully understanding the necessity of the treatment.
Submitting the form via fax without ensuring that all necessary documentation is included represents another mistake. Completeness is essential. If supporting documentation, such as medical records or previous treatment histories, is not submitted along with the form, the authorization process can be extended, leading to treatment delays.
Lastly, individuals often neglect the option to submit the form online. Utilizing the online submission process can save time and reduce complications associated with faxing. The form mentions an online portal for submission, which can streamline the process and ensure a quicker response. Failing to take advantage of such technology may unnecessarily lengthen the timeframe for approval.
Documents used along the form
When navigating the prior authorization process, it is essential to utilize various forms and documents alongside the Cigna Prior Authorization Form. Each document plays a crucial role in ensuring that requests are complete and adequately supported for a timely review. Below is a list of commonly used documents.
- Medication History Form: This document provides a detailed account of a patient's prescription history. It outlines previously prescribed medications, dosages, and any relevant medication compliance issues. This history helps in assessing the necessity of the requested medication.
- Clinical Notes: These notes from the physician detail the patient’s medical condition, treatment history, and the rationale for the requested medication. They can include observations from physical examinations, lab results, and other relevant medical information that supports the authorization request.
- Patient Consent Form: A consent form is critical for obtaining permission to access the patient's medical records. This document complies with privacy regulations and ensures that the appropriate parties can share necessary health information without violating confidentiality.
- Specialist Referral Form: This form is used to document referrals to specialists for further evaluation or treatment. It often includes the reason for the referral, relevant medical history, and the specific expertise required from the specialist, which can be pertinent in the authorization process.
Utilizing these documents along with the Cigna Prior Authorization Form can streamline the process and help ensure that all necessary information is readily available for review. By being thorough in your submissions, you help facilitate a smoother approval journey for the patient.
Similar forms
When navigating the world of medication requests, it's helpful to understand how certain forms relate to one another. The Cigna Prior Authorization Form shares similarities with several other documents used in healthcare settings. Here are four documents that are comparable to it:
- Medicare Prior Authorization Form: This document is utilized when Medicare beneficiaries seek approval for specific treatments or medications. Like the Cigna form, it requires details about the patient, physician, and the requested service. It also emphasizes the need for thorough documentation of medical necessity.
- Medicaid Prior Authorization Request: Medicaid programs often require prior authorization for prescription drugs and certain services. This form aligns closely with the Cigna form by collecting patient information, including diagnosis and treatment history, making it crucial for the approval process.
- Commercial Insurance Prior Authorization Form: Many private insurers require their version of a prior authorization document. Similar to the Cigna form, it requests information about the patient’s identity, medical necessity, and previous treatment attempts to evaluate the appropriateness of the requested medication.
- Drug Utilization Review (DUR) Request: This document helps pharmacists assess appropriate medication use before dispensing. It mirrors the Cigna form by requiring patient and physician details, as well as the medication's dosing and patient history regarding alternative treatments or reactions.
Understanding how these documents relate can facilitate smoother interactions with healthcare providers and insurance companies.
Dos and Don'ts
When filling out the Cigna Prior Auth form, it is crucial to follow certain guidelines to ensure a smooth process. Below are five essential do's and don'ts to keep in mind.
- Do ensure all asterisked (*) fields are completed before submission. This is vital for receiving a timely response.
- Do include comprehensive details about the medication requested, including name, strength, and dosing schedule.
- Do provide accurate patient information, including Cigna ID and date of birth, to avoid processing delays.
- Do verify if the patient has tried alternative medications and document their experiences, especially intolerances or adverse reactions.
- Do call the Cigna helpline for urgent requests to expedite your authorization.
- Don't forget to include the physician's contact information. This makes communication easier if further clarification is needed.
- Don't submit the form without checking for accuracy. Errors can prolong the authorization process.
- Don't neglect to explain why alternative treatments cannot be used if applicable. This information can be crucial to the review process.
- Don't overlook the importance of timely submission. Allow at least five business days for non-urgent requests to be processed.
- Don't rely solely on faxing the form. Use online submission options whenever possible, as they may streamline the process.
Misconceptions
There are several misconceptions regarding the Cigna Prior Authorization form that can lead to confusion during the completion process. Here are six of the most common misunderstandings:
- Every item must be filled out for all requests. While it is crucial to provide all required information, not every question needs an answer for every situation. Only the items marked with an asterisk (*) must be completed.
- Fax is the only method to submit the form. Many people believe that faxing is the sole option for submission. In reality, the form can also be submitted online through a designated website, which is often more efficient.
- The outcome cannot be communicated if the form is submitted without every detail. It's true that Cigna cannot share outcomes via fax if required fields are missing, but providers can receive a response through other communication means if minimum necessities are met.
- Urgent requests always take priority over standard requests. Although urgent requests are prioritized, it is essential to still provide all relevant information promptly to ensure that processing can occur as quickly as possible.
- The standard response time is always five business days. This is the usual time frame, but urgent requests will often be addressed sooner. Specific circumstances might also affect response times, so calling directly for urgent matters is advisable.
- Cigna only accepts information previously documented by the patient. While documentation is vital, it is also acceptable to supply additional contextual information, such as relevant lab values or clinical details, to enhance the processing of the request.
Understanding these misconceptions can streamline the process and improve communication regarding medication prior authorizations. Accurately completing and submitting the form will help ensure that both patients and healthcare providers receive the necessary support.
Key takeaways
When filling out the Cigna Prior Authorization (Prior Auth) form, several key points will help ensure completion and submission are accurate and efficient.
- Complete All Required Fields: Make sure to fill in all asterisked (*) items to receive a timely response.
- Submit Via Fax or Online: You can fax the form to (855) 840-1678. Alternatively, you can submit online at www.covermymeds.com.
- Indicate Urgency: If the request is urgent, indicate this on the form and call (800) 882-4462 for faster processing.
- Provide Medication Details: Clearly specify the medication name, strength, dosage schedule, and duration of therapy required.
- Outline Previous Trials: If the patient has tried alternative medications, include details such as manufacturer name, dates taken, and any adverse reactions.
- Document Alternatives and Reactions: Include information on any alternative treatments the patient has received and document results or reactions experienced.
- Include Additional Information: Provide any relevant clinical reasons, lab values, or other pertinent information to support the authorization request.
- Response Time Frame: The standard review time for the authorization request is 5 business days, so plan accordingly.
- Check Coverage Policies: Be aware of Cigna’s prescription drug list and coverage policies. This information can be found on their website.
By following these takeaways, one can enhance the likelihood of a successful authorization request with Cigna.
Browse Other Templates
How to Make a Schedule of Values - Retainage values are included to hold back a portion of payments until project completion.
Horse Training Contract Template - Owner should notify Trainer of any changes in contact information as needed.
Superbill for Family Practice - Keeping accurate records via the Superbill can lead to improved patient satisfaction and trust.