Fill Out Your Ciwa Ar Form
The CIWA-Ar form, or the Clinical Institute Withdrawal Assessment for Alcohol-Revised, serves as a crucial tool in the assessment of individuals undergoing alcohol withdrawal. This standardized scale helps healthcare providers evaluate ten specific criteria that reflect the severity of withdrawal symptoms. These criteria include nausea and vomiting, anxiety, tremors, agitation, sweating, and various sensory disturbances. Each criterion is scored on a scale, enabling a precise measurement of the patient’s condition. For instance, the evaluation of nausea ranges from none to constant nausea with frequent vomiting, while anxiety levels can escalate to acute panic states in severe cases. Tactile and visual disruptions are also assessed, with patients asked about sensations such as itching or seeing disturbing images. Important for continuity of care, the CIWA-Ar requires regular assessment and documentation of scores, allowing healthcare teams to implement timely interventions. A total score of 8 or higher typically indicates the need for prophylactic medication, emphasizing the importance of early intervention. The CIWA-Ar form, therefore, not only provides a systematic approach to monitoring withdrawal symptoms but also plays an essential role in treatment protocols, ensuring that patients receive the appropriate care and support during a critical time in their recovery journey.
Ciwa Ar Example
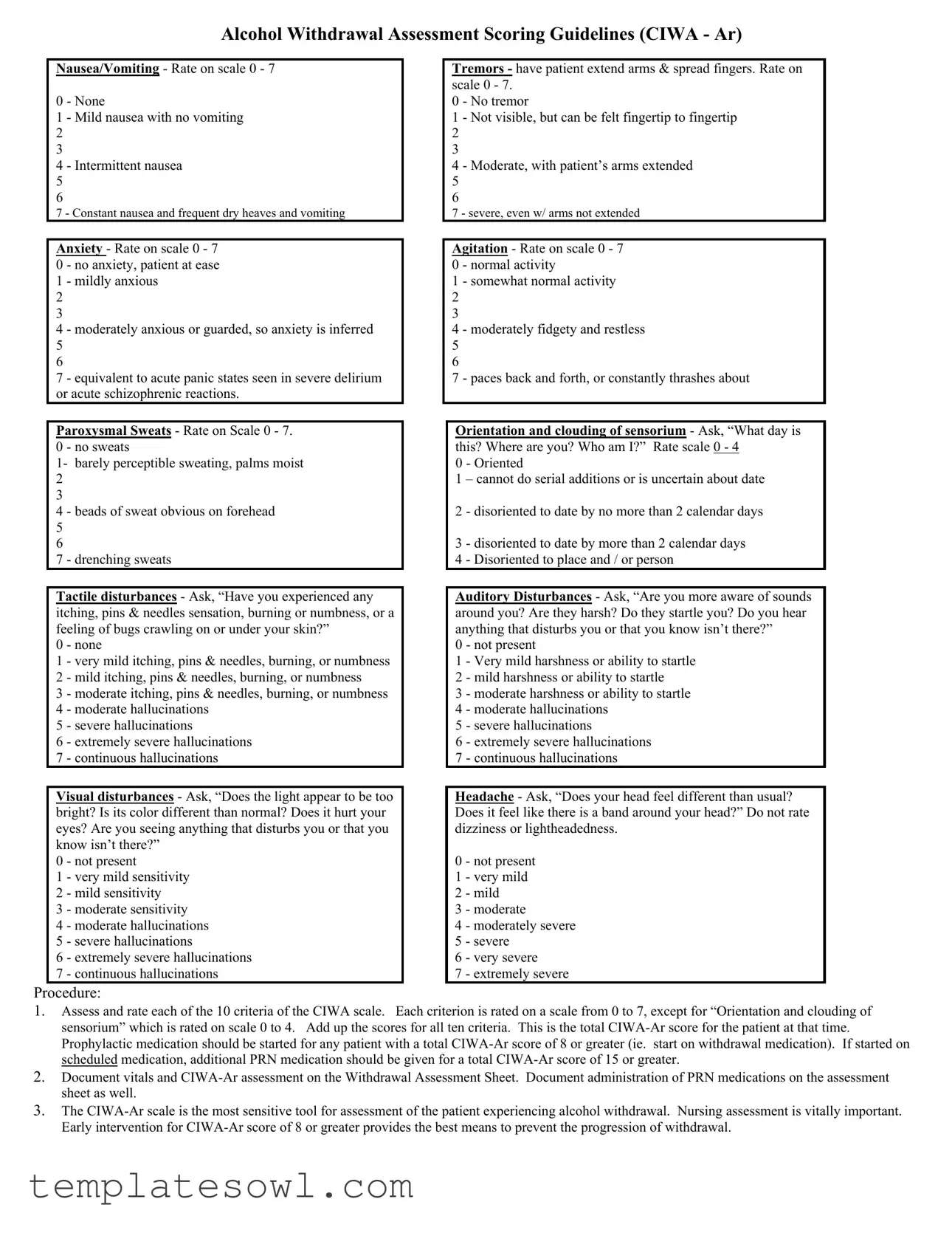
Alcohol Withdrawal Assessment Scoring Guidelines (CIWA - Ar)
Nausea/Vomiting - Rate on scale 0 - 7
0 - None
1 - Mild nausea with no vomiting
2
3
4 - Intermittent nausea
5
6
7 - Constant nausea and frequent dry heaves and vomiting
Anxiety - Rate on scale 0 - 7
0 - no anxiety, patient at ease
1 - mildly anxious
2
3
4 - moderately anxious or guarded, so anxiety is inferred 5 6
7 - equivalent to acute panic states seen in severe delirium or acute schizophrenic reactions.
Paroxysmal Sweats - Rate on Scale 0 - 7.
0 - no sweats
1- barely perceptible sweating, palms moist
2
3
4 - beads of sweat obvious on forehead
5
6
7 - drenching sweats
Tactile disturbances - Ask, “Have you experienced any itching, pins & needles sensation, burning or numbness, or a feeling of bugs crawling on or under your skin?”
0 - none
1 - very mild itching, pins & needles, burning, or numbness 2 - mild itching, pins & needles, burning, or numbness
3 - moderate itching, pins & needles, burning, or numbness 4 - moderate hallucinations
5 - severe hallucinations
6 - extremely severe hallucinations
7 - continuous hallucinations
Visual disturbances - Ask, “Does the light appear to be too bright? Is its color different than normal? Does it hurt your eyes? Are you seeing anything that disturbs you or that you know isn’t there?”
0 - not present
1 - very mild sensitivity
2 - mild sensitivity
3 - moderate sensitivity
4 - moderate hallucinations
5 - severe hallucinations
6 - extremely severe hallucinations
7 - continuous hallucinations
Tremors - have patient extend arms & spread fingers. Rate on scale 0 - 7.
0 - No tremor
1 - Not visible, but can be felt fingertip to fingertip 2 3
4 - Moderate, with patient’s arms extended
5
6
7 - severe, even w/ arms not extended
Agitation - Rate on scale 0 - 7 0 - normal activity
1 - somewhat normal activity
2
3
4 - moderately fidgety and restless
5
6
7 - paces back and forth, or constantly thrashes about
Orientation and clouding of sensorium - Ask, “What day is this? Where are you? Who am I?” Rate scale 0 - 4
0 - Oriented
1 – cannot do serial additions or is uncertain about date
2 - disoriented to date by no more than 2 calendar days
3 - disoriented to date by more than 2 calendar days 4 - Disoriented to place and / or person
Auditory Disturbances - Ask, “Are you more aware of sounds around you? Are they harsh? Do they startle you? Do you hear anything that disturbs you or that you know isn’t there?”
0 - not present
1 - Very mild harshness or ability to startle
2 - mild harshness or ability to startle
3 - moderate harshness or ability to startle
4 - moderate hallucinations
5 - severe hallucinations
6 - extremely severe hallucinations
7 - continuous hallucinations
Headache - Ask, “Does your head feel different than usual? Does it feel like there is a band around your head?” Do not rate dizziness or lightheadedness.
0 - not present
1 - very mild
2 - mild
3 - moderate
4 - moderately severe
5 - severe
6 - very severe
7 - extremely severe
Procedure:
1.Assess and rate each of the 10 criteria of the CIWA scale. Each criterion is rated on a scale from 0 to 7, except for “Orientation and clouding of sensorium” which is rated on scale 0 to 4. Add up the scores for all ten criteria. This is the total
2.Document vitals and
3.The
|
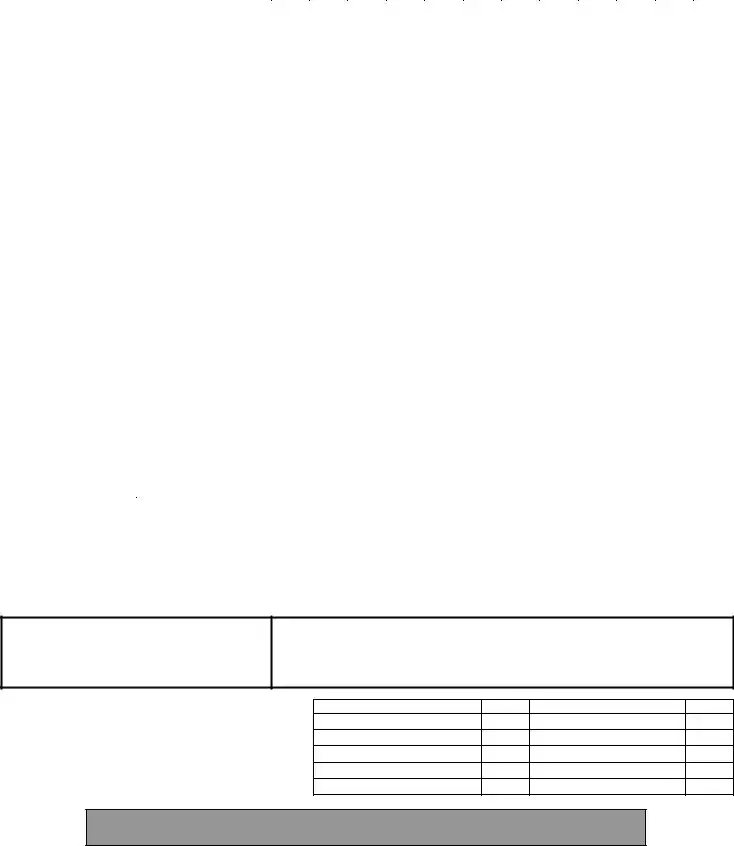
Assessment Protocol |
|
|
Date |
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
a. Vitals, Assessment Now. |
|
|
Time |
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
b. If initial score 8 repeat q1h x 8 hrs, then |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
if stable q2h x 8 hrs, then if stable q4h. |
|
Pulse |
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
c. If initial score < 8, assess q4h x 72 hrs. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
RR |
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
If score < 8 for 72 hrs, d/c assessment. |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
If score 8 at any time, go to (b) above. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
O2 sat |
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
d. If indicated, (see indications below) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
administer prn medications as ordered and |
|
BP |
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
record on MAR and below. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
Assess and rate each of the following |
Refer to reverse for detailed instructions in use of the |
|||||||||||||||||
|
Nausea/vomiting (0 - 7) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
0 |
- none; 1 - mild nausea ,no vomiting; 4 - intermittent nausea; |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
7 |
- constant nausea , frequent dry heaves & vomiting. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Tremors (0 - 7) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
0 |
- no tremor; 1 - not visible but can be felt; 4 - moderate w/ arms |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
extended; 7 - severe, even w/ arms not extended. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Anxiety (0 - 7) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
0 |
- none, at ease; 1 - mildly anxious; 4 - moderately anxious or |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
guarded; 7 - equivalent to acute panic state |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
Agitation (0 - 7) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
0 |
- normal activity; 1 - somewhat normal activity; 4 - moderately |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
fidgety/restless; 7 - paces or constantly thrashes about |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Paroxysmal Sweats (0 - 7) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
0 |
- no sweats; |
1 - barely perceptible sweating, palms moist; |
|
|
|
|
|
|
|
|
|
|
|
|
|||||
4 |
- beads of sweat obvious on forehead; |
7 - drenching sweat |
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Orientation (0 - 4) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
0 |
- oriented; 1 - uncertain about date; 2 - disoriented to date by no |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
more than 2 days; 3 - disoriented to date by > 2 days; |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
4 - disoriented to place and / or person |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
Tactile Disturbances (0 - 7) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
0 |
- none; 1 - very mild itch, P&N, ,numbness; |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
burning, numbness; 3 - moderate itch, P&N, burning ,numbness; |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
4 |
- moderate hallucinations; 5 - severe hallucinations; |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
6 – extremely severe hallucinations; 7 - continuous hallucinations |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
Auditory Disturbances (0 - 7) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
0 |
- not present; 1 - very mild harshness/ ability to startle; 2 - mild |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
harshness, ability to startle; 3 - moderate harshness, ability to |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
startle; 4 - moderate hallucinations; 5 severe hallucinations; |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
6 |
- extremely severe hallucinations; 7 - continuous.hallucinations |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
Visual Disturbances (0 - 7) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
0 |
- not present; |
1 - very mild sensitivity; |
2 - mild sensitivity; |
|
|
|
|
|
|
|
|
|
|
|
|
||||
3 |
- moderate sensitivity; 4 - moderate hallucinations; 5 - severe |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
hallucinations; |
6 - extremely severe hallucinations; |
7 - |
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
continuous hallucinations |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
Headache (0 - 7) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
0 |
- not present; 1 - very mild; 2 - mild; 3 - moderate; 4 - moderately |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
severe; 5 - severe; 6 - very severe; 7 - extremely severe |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Total |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
PRN Med: (circle one) |
|
Dose given (mg): |
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
Diazepam |
Lorazepam |
|
|
|
Route: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Time of PRN medication administration: |
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
Assessment of response |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
minutes after medication administered) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
RN Initials |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Scale for Scoring:
Total Score =
0 – 9: absent or minimal withdrawal
10 – 19: mild to moderate withdrawal
more than 20: severe withdrawal
Indications for PRN medication:
a.Total
b.Total
Patient Identification (Addressograph)
Signature/ Title
Initials
Signature / Title
Initials
Alcohol Withdrawal Assessment Flowsheet (revised Nov 2003)
Form Characteristics
| Fact Name | Description |
|---|---|
| Assessment Tool | The CIWA-Ar (Clinical Institute Withdrawal Assessment for Alcohol-Revised) is a standardized tool to assess the severity of alcohol withdrawal symptoms. |
| Scoring Range | Each of the ten assessed criteria is rated on a scale of 0 to 7, except for "Orientation and clouding of sensorium," which is rated from 0 to 4. |
| Significance of Scores | A total CIWA-Ar score of 8 or greater indicates a need for prophylactic medication, marking a significant threshold for intervention. |
| Monitoring Frequency | If the initial score is 8 or more, assessments are repeated every hour for up to 8 hours; thereafter, they become less frequent if stable. |
| Categories of Symptoms | Symptoms assessed include anxiety, tremors, sweating, hallucinations, and headaches among others, each contributing to the total score. |
| Decision-Making Criteria | Patients showing a score of 15 or higher on the CIWA-Ar while on scheduled medication require an additional dose of PRN medication. |
| Intervention Guidelines | The CIWA-Ar is most effective when administered by nursing professionals who can provide early intervention to prevent severe withdrawal. |
| Clinical Application | The CIWA-Ar is widely used in clinical settings across the U.S. for managing patients undergoing alcohol withdrawal, aiding in evidence-based treatment strategies. |
Guidelines on Utilizing Ciwa Ar
Once you have the CIWA-Ar form in front of you, the next steps will involve rating the patient's symptoms based on specific criteria. Accurate assessment is key in providing the right care during withdrawal. Below are the steps you need to follow to complete the form correctly.
- Begin with entering the patient’s identification details at the top of the form.
- Document the date and time of the assessment.
- Assess and rate each of the 10 criteria on the CIWA-Ar scale. Use the following guidelines for scoring:
- Nausea/Vomiting: Rate from 0 to 7.
- Anxiety: Rate from 0 to 7.
- Paroxysmal Sweats: Rate from 0 to 7.
- Tactile Disturbances: Rate from 0 to 7.
- Visual Disturbances: Rate from 0 to 7.
- Tremors: Rate from 0 to 7.
- Agitation: Rate from 0 to 7.
- Orientation and Clouding of Sensorium: Rate from 0 to 4.
- Auditory Disturbances: Rate from 0 to 7.
- Headache: Rate from 0 to 7.
- Add up the scores for all ten criteria to obtain the total CIWA-Ar score.
- If the total score is 8 or greater, consider starting prophylactic medication for the patient.
- Document vital signs and the CIWA-Ar assessment details on the Withdrawal Assessment Sheet.
- Track and document any PRN medications administered, including the dosage and response after 30-60 minutes.
Filling out the CIWA-Ar form accurately ensures that vital information is conveyed. This assessment helps healthcare providers determine the appropriate level of intervention for managing alcohol withdrawal symptoms effectively.
What You Should Know About This Form
What is the CIWA-Ar form used for?
The CIWA-Ar form is a tool used by healthcare providers to assess the severity of alcohol withdrawal symptoms in patients. It helps in monitoring symptoms such as nausea, anxiety, tremors, and disturbances in perception. By evaluating these symptoms, providers can make informed decisions about the necessary interventions, ensuring the patient receives appropriate care to minimize withdrawal complications.
How does scoring on the CIWA-Ar scale work?
Each symptom is assessed on a scale that usually ranges from 0 to 7, with 0 indicating no symptoms and higher scores indicating increasing severity. For the "Orientation and clouding of sensorium" criteria, there is a different scale from 0 to 4. After scoring each of the ten criteria, the scores are totaled to determine the overall CIWA-Ar score. This score helps guide treatment decisions for the patient.
When should prophylactic medication be initiated based on the CIWA-Ar score?
If the total CIWA-Ar score reaches 8 or greater, prophylactic medication should be started. This early intervention is crucial in managing potential withdrawal complications effectively. For those on scheduled medication, additional PRN medication is advised if the score hits 15 or higher.
What symptoms are evaluated in the CIWA-Ar assessment?
The CIWA-Ar assessment evaluates the following symptoms: nausea/vomiting, anxiety, paroxysmal sweats, tactile disturbances, visual disturbances, tremors, agitation, orientation and clouding of sensorium, auditory disturbances, and headache. Each of these symptoms is crucial for determining the severity of alcohol withdrawal the patient is experiencing.
What should be documented after completing the CIWA-Ar assessment?
It's essential to document the patient's vital signs, the CIWA-Ar assessment scores, and any medications administered. This information should be recorded on the Withdrawal Assessment Sheet to maintain an accurate and comprehensive medical record, facilitating effective ongoing care and monitoring.
How often should the CIWA-Ar assessment be repeated?
If the initial CIWA-Ar score is 8 or higher, assessments should be repeated every hour for a total of eight hours. If the patient's condition stabilizes, the frequency can decrease to every two hours for another eight hours, and then every four hours. For initial scores under 8, assessment should occur every four hours for up to 72 hours. This regular monitoring is key to adjusting treatment as necessary.
What actions should be taken if a patient’s CIWA-Ar score exceeds critical thresholds?
If the total CIWA-Ar score exceeds 35, or if a patient requires extensive medication or experiences respiratory distress, transfer to an intensive care unit may be necessary. Continuous assessment is essential in these cases to ensure the patient's safety and effective management of severe withdrawal symptoms.
Common mistakes
Filling out the CIWA-Ar form accurately is crucial for effective patient assessment during alcohol withdrawal. However, several common mistakes can diminish its effectiveness. First, many people fail to consider the specific scaling for each criterion. Each section of the CIWA-Ar form requires a score between 0 and 7, except for "Orientation and clouding of sensorium," which is rated from 0 to 4. Misinterpreting the scales can lead to inaccurate scores that may compromise patient care.
Another frequent error is not seeking clarification before scoring. It is essential to ask patients specific questions about their symptoms. For example, instead of assuming a general state of agitation, a detailed inquiry into their feelings regarding anxiety or agitation can provide a clearer picture of their condition. Skipping this essential step results in incomplete evaluations.
Many assessors also overlook the importance of documentation. Failing to document vital signs and assessments can interfere with continuity of care. The form not only tracks withdrawal symptoms but also guides medical responses. It's vital to ensure that everything is documented accurately, including any medications administered.
People often rush through the assessment process. Moving too quickly can lead to misjudgments. It's crucial to take the time needed to assess each criterion thoroughly. Making hasty decisions could result in a missed severe withdrawal state that requires immediate intervention.
Another common mistake is inadequate communication among healthcare providers. Not sharing a completed CIWA-Ar assessment with the healthcare team can create gaps in treatment. Consistent communication is essential for patient safety and effective care.
Some individuals might incorrectly assume that symptoms do not require continual reassessment. Failing to re-evaluate patients regularly can cause missed opportunities for timely medical intervention. For patients with a CIWA-Ar score of 8 or higher, regular re-assessment can prevent their condition from worsening.
Lastly, patients may provide inaccurate information due to misunderstanding questions or the assessment's purpose. Not tailoring questions to the individual can lead to unreliable responses. Understanding a patient's background and their language barriers, if any, can make a significant difference in obtaining accurate assessments.
Documents used along the form
The CIWA-Ar form is a critical tool used for assessing withdrawal symptoms in individuals experiencing alcohol withdrawal. Several other documents are often utilized in conjunction with the CIWA-Ar form to ensure comprehensive patient monitoring and treatment. Below is a list of these forms and a brief description of each.
- Withdrawal Assessment Sheet: This document records the CIWA-Ar assessment scores along with patients' vitals and medication administration. It allows healthcare providers to track changes over time and make timely interventions.
- MAR (Medication Administration Record): This record tracks the medications given to the patient, including dosages and times of administration. It's essential for maintaining accurate medication history.
- Patient Identification Form: This form ensures that patient details are correctly documented for identification purposes. It often includes reliance on an addressograph or patient ID number to prevent mix-ups.
- Nursing Assessment Notes: Nurses document their observations, treatments, and any significant changes in the patient's condition on these notes. This provides vital insights and ensures continuity of care among staff.
- Physician’s Order Sheet: This document outlines the orders given by physicians concerning the patient’s treatment plan, medication, and any specific interventions needed based on the CIWA-Ar assessment.
- Vital Signs Chart: Recording vital signs is critical to monitoring the patient's physical state. This chart assists in tracking trends over time, aiding in making informed decisions about ongoing treatment.
- Transfer Documentation: In cases where a patient may need to be transferred to a higher level of care, such as an intensive care unit (ICU), this documentation includes detailed information about the patient's status and treatment received to ensure proper continuity of care.
Utilizing these forms alongside the CIWA-Ar form helps healthcare providers effectively monitor and manage patients going through alcohol withdrawal. Such comprehensive documentation supports better clinical decisions and enhances patient safety and care quality.
Similar forms
- Clinical Assessment Tools: Similar to CIWA-Ar, such tools like the Beck Depression Inventory help assess subclinical symptoms. They both provide structured methods for scoring specific criteria based on observed or self-reported symptoms.
- Withdrawal Severity Scale: Like the CIWA-Ar, the Withdrawal Severity Scale (WSS) quantifies withdrawal symptoms through rating scales. Both allow healthcare professionals to evaluate the severity of symptoms and determine a course of action.
- Alcohol Use Disorders Identification Test (AUDIT): The AUDIT screen functions similarly by identifying potential alcohol use disorder. It assesses various behaviors and their consequences related to alcohol, helping inform the clinical approach.
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5): The DSM-5 outlines criteria for alcohol use disorder, similar to CIWA-Ar, which guides treatment decisions based on symptom presence and severity.
- Patient Health Questionnaire (PHQ-9): The PHQ-9 assesses depression symptoms similarly to how CIWA-Ar does for withdrawal. Both employ a self-report format with scored responses to gauge severity and need for intervention.
- Generalized Anxiety Disorder 7-item scale (GAD-7): This scale, like the CIWA-Ar, helps evaluate anxiety symptoms through a structured questionnaire. Both scales assist providers in understanding a patient's mental health and determining necessary interventions.
Dos and Don'ts
When filling out the CIWA-Ar form, it's crucial to approach the task with care. This ensures accurate assessment and effective treatment for patients undergoing alcohol withdrawal. Here are nine guidelines to follow:
- Do ensure clarity in responses: When rating symptoms, provide clear and concise answers to reflect the patient's condition accurately.
- Do utilize the complete scale: Rate each criterion on the provided scale, ensuring every aspect is assessed.
- Don’t provide subjective opinions: Stick to the facts of what the patient expresses and experiences.
- Do document medications properly: Record any prophylactic or PRN medication given along with the CIWA-Ar assessment.
- Don’t skip critical assessment questions: Ensure all questions are asked and documented to create a full picture of the patient’s state.
- Do monitor the patient frequently: For those scoring 8 or higher, repeat assessments must be timely and consistent.
- Don’t ignore abnormal findings: Any score indicating severe withdrawal should prompt immediate action.
- Do rotate who conducts assessments: Allow different nurses to evaluate and document observations to prevent bias.
- Don’t rush the assessment process: Take the necessary time to ensure thorough evaluations and accurate ratings.
By following these guidelines, healthcare professionals can offer better care and potentially improve outcomes for those at risk of severe alcohol withdrawal.
Misconceptions
- Misconception 1: The CIWA-Ar scale is only useful for severe withdrawal cases.
- Misconception 2: CIWA-Ar scoring can be conducted without patient interaction.
- Misconception 3: A total score of 8 or greater automatically means medication must be administered.
- Misconception 4: The CIWA-Ar scale only focuses on physical symptoms of alcohol withdrawal.
- Misconception 5: Only nurses can perform CIWA-Ar assessments.
In reality, the CIWA-Ar scale is designed to assess withdrawal symptoms across a spectrum of severity. It can effectively identify mild cases, allowing for early intervention before symptoms escalate. Regular assessment is crucial for all patients at risk of withdrawal.
It's essential to engage with the patient during the assessment. The scale includes questions about symptoms like tactile or auditory disturbances, which require the patient's input for accurate scoring. Understanding the patient’s experience helps in tailoring effective treatment.
While a score of 8 or higher indicates potential withdrawal, clinical judgment should guide the decision to administer medication. Not every patient with a high score will require immediate intervention; monitoring and evaluating each individual's condition is essential.
This misconception overlooks the cognitive and emotional aspects of withdrawal. The CIWA-Ar scale assesses symptoms like anxiety, orientation, and sensorium, which are crucial for understanding the full impact of withdrawal on a patient's mental state.
While nurses play a critical role in using the CIWA-Ar scale, any trained healthcare provider can conduct the assessment. It’s vital for all team members involved in the care of patients experiencing withdrawal to be familiar with the scale and its application to ensure comprehensive patient care.
Key takeaways
When filling out and using the CIWA-Ar (Clinical Institute Withdrawal Assessment for Alcohol), keep these key takeaways in mind:
- Thorough Assessment is Crucial: Carefully assess each of the ten criteria separately. Each item helps gauge the severity of withdrawal symptoms.
- Scoring Matters: Scores from 0 to 7 are assigned for most symptoms, while orientation is rated from 0 to 4. A higher score indicates more severe symptoms.
- Document Everything: Always document vitals and CIWA-Ar assessments on the Withdrawal Assessment Sheet. Track the administration of any PRN medications, as this can provide essential information for ongoing care.
- Timely Intervention is Key: If the total CIWA-Ar score is 8 or greater, it’s time to start prophylactic medication. Addressing withdrawal symptoms early can help prevent serious complications.
Browse Other Templates
What Is Conduent - Submission of the W2 is an annual requirement that contributes to the greater financial ecosystem of society.
Maintenance Bond Form - Defective workmanship must be repaired within the bond period.