Fill Out Your Clinical Incident Report Sample Form
The Clinical Incident Report Sample form serves as an essential document designed to ensure the safety and quality of patient care. It provides a structured approach for reporting unexpected incidents during patient treatment, encompassing a wide range of issues from equipment malfunctions to breaches in protocols. Each section of the form requests specific information, such as the identification of the affected person, the location of the incident, and the date and time it occurred. FASTAFF personnel fill out this form to complement the reporting obligations of healthcare facilities, ensuring a comprehensive account of the incident. Medical professionals are tasked with specifying the nature of the incident by checking relevant boxes, which helps categorize issues such as medication errors or safety hazards. Additionally, the form captures patient outcomes, allowing for the identification of potential impacts, ranging from near misses to severe complications. Contributory factors like poor communication or inadequate training are also recorded, helping organizations understand underlying problems. Importantly, the form requires a factual summary of the incident while emphasizing the necessity of taking appropriate actions to prevent future occurrences. Employee acknowledgment is solicited to affirm the accuracy of the information provided. This thorough documentation not only aids in immediate responses to incidents but also fosters an environment of continuous improvement and accountability in healthcare settings.
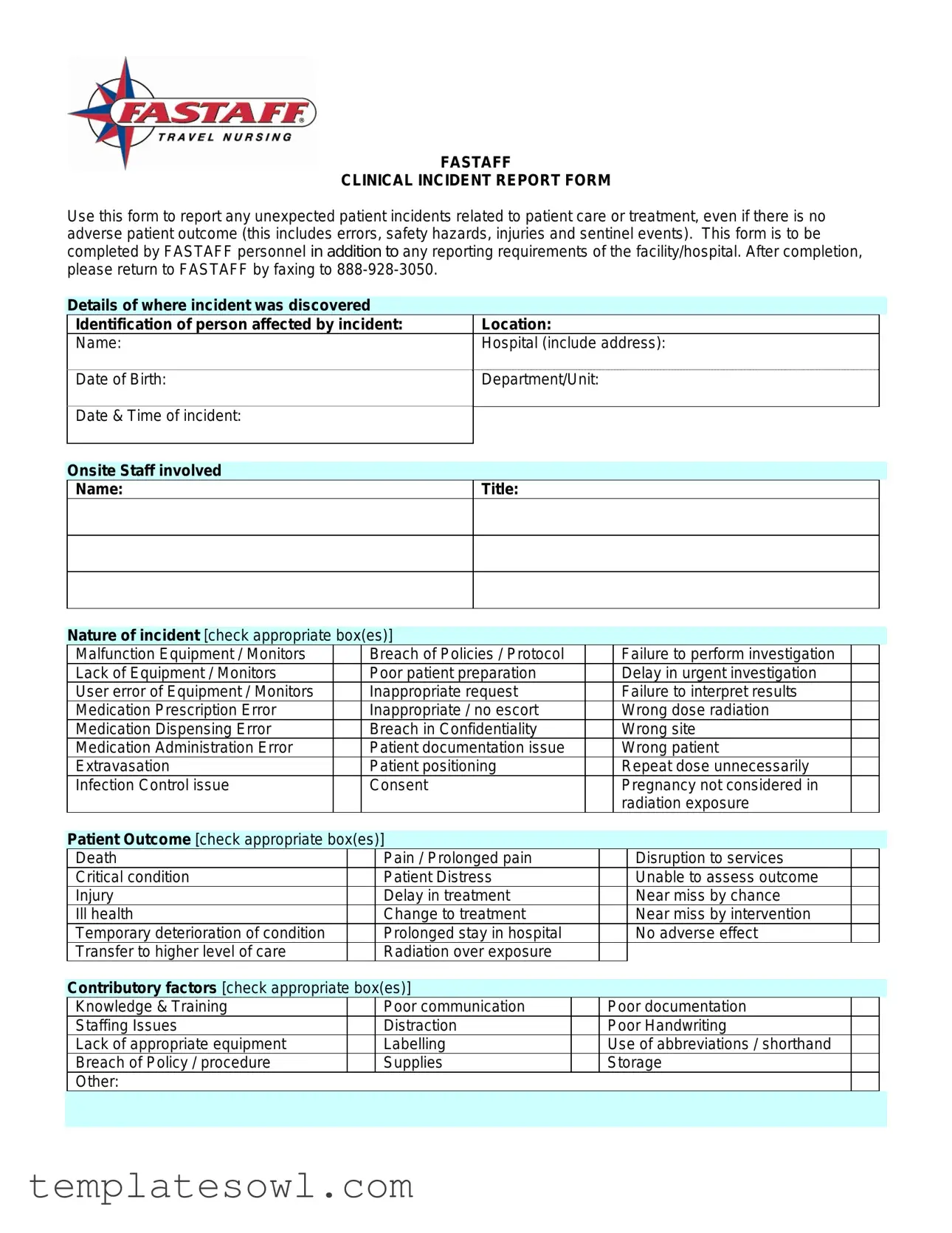
Clinical Incident Report Sample Example
FASTAFF
CLINICAL INCIDENT REPORT FORM
Use this form to report any unexpected patient incidents related to patient care or treatment, even if there is no adverse patient outcome (this includes errors, safety hazards, injuries and sentinel events). This form is to be completed by FASTAFF personnel in addition to any reporting requirements of the facility/hospital. After completion, please return to FASTAFF by faxing to
|
Details of where incident was discovered |
|
|
|
Identification of person affected by incident: |
Location: |
|
|
Name: |
Hospital (include address): |
|
|
Date of Birth: |
Department/Unit: |
|
|
|
||
|
Date & Time of incident: |
|
|
|
|
|
|
|
|
|
|
Onsite Staff involved Name:
Title:
|
Nature of incident [check appropriate box(es)] |
|
|
|
|
|
|
|||||
|
Malfunction Equipment / Monitors |
|
|
Breach of Policies / Protocol |
|
|
Failure to perform investigation |
|
|
|||
|
Lack of Equipment / Monitors |
|
|
Poor patient preparation |
|
|
Delay in urgent investigation |
|
|
|||
|
User error of Equipment / Monitors |
|
|
Inappropriate request |
|
|
Failure to interpret results |
|
|
|||
|
Medication Prescription Error |
|
|
Inappropriate / no escort |
|
|
Wrong dose radiation |
|
|
|||
|
Medication Dispensing Error |
|
|
Breach in Confidentiality |
|
|
Wrong site |
|
|
|||
|
Medication Administration Error |
|
|
Patient documentation issue |
|
|
Wrong patient |
|
|
|||
|
Extravasation |
|
|
Patient positioning |
|
|
Repeat dose unnecessarily |
|
|
|||
|
Infection Control issue |
|
|
Consent |
|
|
Pregnancy not considered in |
|
|
|||
|
|
|
|
|
|
|
|
|
radiation exposure |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Patient Outcome [check appropriate box(es)] |
|
|
|
|
|
|
|||||
|
Death |
|
|
|
Pain / Prolonged pain |
|
|
|
Disruption to services |
|
|
|
|
Critical condition |
|
|
|
Patient Distress |
|
|
|
Unable to assess outcome |
|
|
|
|
Injury |
|
|
|
Delay in treatment |
|
|
|
Near miss by chance |
|
|
|
|
Ill health |
|
|
|
Change to treatment |
|
|
|
Near miss by intervention |
|
|
|
|
Temporary deterioration of condition |
|
|
|
Prolonged stay in hospital |
|
|
|
No adverse effect |
|
|
|
|
Transfer to higher level of care |
|
|
|
Radiation over exposure |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
Contributory factors [check appropriate box(es)] |
|
|
|
|
|
|
|||||
|
Knowledge & Training |
|
|
|
Poor communication |
|
|
Poor documentation |
|
|
||
|
Staffing Issues |
|
|
|
Distraction |
|
|
Poor Handwriting |
|
|
||
|
Lack of appropriate equipment |
|
|
|
Labelling |
|
|
Use of abbreviations / shorthand |
|
|
||
|
Breach of Policy / procedure |
|
|
|
Supplies |
|
|
Storage |
|
|
||
|
Other: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Summary of what happened: (please state facts only and not opinion – attach separate sheet if necessary) Ensure that all necessary steps have been taken to support and treat anyone injured and prevent injury to others. Ensure medical records are factual and up to date.
Action Taken as a Result of Incident: (please give brief
Employee Acknowledgment |
|
Employee Name: |
Title/Position: |
Acknowledgment - I acknowledge that the facts and circumstances reported above are true and accurate to the best of my knowledge:
______________________________________________________
Employee Signature |
Date |
INTERNAL USE ONLY – COMPLETED BY FASTAFF DIRECTOR OF CREDENTIALING
Action Taken as a Result of Incident: (please give brief
____________________________________________________________________
Director of Credentialing |
Date |
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The Clinical Incident Report Form is used to document unexpected patient incidents that arise during patient care or treatment, regardless of whether there is an adverse outcome. |
| Who Completes the Form | This form must be filled out by FASTAFF personnel. It is essential to follow any additional reporting requirements set by the facility or hospital where the incident occurred. |
| Submission Method | Once completed, the form should be returned to FASTAFF via fax at 888-928-3050. |
| Types of Incidents | The form allows the reporting of various incidents, including equipment malfunctions, medication errors, breaches of policy, and patient safety issues. |
| Patient Outcome | The form includes options to select the impact on the patient, such as pain, injury, or critical condition, enabling a comprehensive overview of the situation. |
| Legal Compliance | Using this form helps ensure compliance with state laws that govern patient care and safety reporting, providing a clear record of events and actions taken. |
Guidelines on Utilizing Clinical Incident Report Sample
Filling out the Clinical Incident Report form requires careful attention to detail and factual accuracy. This process captures critical information about unexpected incidents related to patient care to ensure safety and compliance. Follow these steps to properly complete the form.
- Identify the Incident: Begin by stating the details where the incident was discovered. Include specific information such as the location and the hospital address.
- Document Personal Information: Record the name and date of birth of the person affected by the incident, as well as their department or unit.
- Date and Time: Indicate when the incident occurred, providing both the date and exact time.
- Onsite Staff Involved: List the names and titles of any staff members involved in the incident.
- Nature of Incident: Check all appropriate boxes to categorize the incident. Possible issues may include equipment malfunction, user error, or medication dispensing errors.
- Patient Outcome: Check the relevant boxes to describe the patient's condition following the incident. This could range from no adverse effect to critical condition.
- Contributory Factors: Identify any factors that may have contributed to the incident. This includes poor communication, distractions, or lack of training.
- Summary of What Happened: Write a factual summary of the incident without including opinions. Use an additional sheet if necessary to provide complete details.
- Action Taken: Briefly describe any immediate actions taken in response to the incident. Attach more information if needed.
- Employee Acknowledgment: Have the employee involved sign and date the report to acknowledge that the information is accurate to the best of their knowledge.
- Internal Use: This section should be completed by the Fastaff Director of Credentialing. Include any actions taken as a result of the incident and the date.
After filling out the form, make sure to fax it to 888-928-3050 as instructed. Keeping accurate and thorough records ensures that the healthcare environment continues to prioritize patient safety and quality care.
What You Should Know About This Form
What is the purpose of the Clinical Incident Report Sample form?
The Clinical Incident Report Sample form serves as a structured tool for reporting unexpected incidents related to patient care and treatment. This can include a wide range of occurrences, such as errors, safety hazards, or other unsettling events, regardless of whether or not these incidents result in patient harm. The form assists FASTAFF personnel in documenting events thoroughly and systematically, ensuring compliance with both internal protocols and external reporting requirements. By using this form, facilities can improve patient safety, identify trends, and promote better care practices.
Who is responsible for completing the form?
The responsibility for completing the Clinical Incident Report form lies primarily with FASTAFF personnel. This includes any staff members who are directly involved in or witness the incident. It is essential that the individual filling out the form provides accurate and factual information regarding the incident. Additionally, any necessary actions taken to address the situation, as well as relevant details about involved staff or patients, must be correctly documented to ensure a comprehensive report.
What information is required on the form?
The form requires several critical pieces of information. First, it asks for basic details such as the name of the patient affected, their date of birth, and the department where the incident occurred. Then, it details the nature of the incident, allowing the reporter to check appropriate boxes, thus categorizing the type. Further, it includes a section for describing the patient’s outcome and any contributory factors that may have played a role in the incident. Finally, there is space for summarizing the incident and any actions taken as a result, ensuring thorough visibility into the event.
What should be done after completing the Clinical Incident Report form?
Once the Clinical Incident Report form is completed, it must be returned to FASTAFF promptly. This is typically done by faxing the form to 888-928-3050. It is crucial that the report is filled out accurately and succinctly, as it serves not only as documentation of the incident but also as a potential catalyst for improving safety practices. After submission, the report will be reviewed internally to identify trends or areas needing improvement, ensuring that all necessary follow-up actions are taken for the continued safety and care of patients.
Common mistakes
When filling out the Clinical Incident Report Sample form, accuracy is critical. One common mistake is failing to provide complete information about the person affected by the incident. This includes not only the name and department but also the date of birth and other identifying details. Incomplete information can hinder a proper investigation and complicate follow-up actions.
Another frequent error is neglecting to specify the location where the incident occurred. Without a precise location, it might be challenging to understand the context of the incident. It's essential to indicate where exactly the incident took place, whether in a specific hospital wing or a particular department.
Additionally, many people check off multiple boxes under the "Nature of Incident" section without thoroughly considering each option. This can lead to ambiguity about what occurred. It is better to select only the most relevant categories that truly describe the incident instead of overwhelming the form with too many unchecked boxes.
Providing a detailed summary of what happened is often overlooked. Some individuals may skip writing a summary or include vague language. A concise, factual account helps everyone understand the situation clearly. If necessary, include an attachment for more thorough details.
Moreover, people sometimes forget to document the action taken in response to the incident. This section is crucial for understanding how the issue was addressed and ensuring that necessary steps are in place to prevent recurrence. Omitting this information can lead to repeated mistakes.
Lastly, signatures and dates can often be overlooked. The acknowledgment section requires a signature to confirm that the report is accurate. Failing to sign or date the report may delay the review process or cause the report to be considered incomplete, impacting accountability and follow-up actions.
Documents used along the form
When a clinical incident occurs, several important forms and documents are typically utilized alongside the Clinical Incident Report Form. These documents ensure that all relevant details are recorded and that appropriate follow-up actions are taken. Below are some common forms that accompany the Clinical Incident Report.
- Patient Complaint Form: This form allows patients or their families to formally document complaints regarding their care. It captures specific grievances and provides a structured way for the facility to address concerns.
- Incident Follow-Up Report: Following the initial report, this document outlines the results of any investigations conducted after the incident. It helps in tracking progress on how issues will be resolved or mitigated.
- Root Cause Analysis Template: This form is used to identify the underlying factors contributing to the incident. It helps teams analyze what went wrong to improve processes and prevent similar occurrences in the future.
- Corrective Action Plan: This document lays out specific measures that will be taken to address the issues highlighted in the Clinical Incident Report. It includes timelines and responsible parties for each action.
- Staff Training Evaluation Form: This evaluation assesses whether staff training is adequate and identifies any areas needing improvement to prevent future incidents, ensuring that staff members stay competent in their roles.
- Equipment Maintenance Log: This log tracks the maintenance and inspections of medical equipment used in the incident, providing accountability and safety checks for equipment performance.
- Patient Safety Report: Compiled periodically, this report summarizes all safety incidents over a specific timeframe, offering insights into trends and areas in need of improvement across the facility.
Each of these documents serves a critical role in maintaining patient safety and improving healthcare practices. Together with the Clinical Incident Report, they help ensure a thorough response to incidents, engage staff in continuous improvement, and enhance overall care quality.
Similar forms
-
Accident Report Form: Like the Clinical Incident Report, this form captures details about unexpected incidents, focusing on the who, what, and where of an accident. Both documents aim to document facts only, minimizing personal opinions to maintain objectivity.
-
Patient Safety Event Report: This document is similar in that it aims to enhance patient safety by reporting events that could lead to harm. Both forms emphasize identifying contributing factors and documenting actions taken to prevent recurrence.
-
Incident Investigation Report: This report serves as a thorough examination of incidents, similar to the Clinical Incident Report. Both documents require a summary of what happened and the steps taken following the incident, ensuring accountability and corrective measures are documented.
-
Quality Assurance Report: This type of report overlaps with the Clinical Incident Report by assessing incidents that could affect the quality of care. Both forms focus on incident analysis and require a breakdown of factors leading to the event and the actions taken in response.
Dos and Don'ts
When filling out the Clinical Incident Report Sample form, it's important to follow some best practices to ensure clarity and accuracy. Here are five things you should do, along with five things you should avoid:
- DO: Write clearly and legibly to ensure your information is easily readable.
- DO: Include all relevant details, such as names, dates, and specific incidents.
- DO: Stick to the facts. Focus on what happened without including opinions.
- DO: Follow the reporting requirements set by your facility or hospital.
- DO: Ensure that any necessary medical assistance has been provided to affected individuals.
- DON'T: Use abbreviations that might confuse the reader.
- DON'T: Omit any vital information that could help in understanding the incident.
- DON'T: Include personal opinions or assumptions about what may have caused the incident.
- DON'T: Forget to check for typos or errors in the report.
- DON'T: Submit the report without reviewing it for completeness.
Misconceptions
Understanding the Clinical Incident Report Sample form is crucial for maintaining high standards in patient care. However, several misconceptions frequently arise regarding how this form operates. Here are ten of the most common misunderstandings:
- Only serious incidents need to be reported. Many people believe that only incidents resulting in harm to the patient require reporting. In reality, any unexpected occurrence, regardless of the outcome, should be documented.
- This form is only for fast-affiliated incidents. While it is a form provided by FASTAFF, it applies to any incident related to patient care within various healthcare facilities, not just those associated with FASTAFF.
- Completing the form is optional. Some may assume that filling out the form is merely a suggestion. It is, in fact, a critical part of reporting protocols that helps improve patient safety.
- The form must be filled out immediately. While urgent reporting is essential, the form can be completed as soon as accurate information is gathered. Promptness is encouraged but not always feasible.
- The report impacts my employment status negatively. Many individuals fear repercussions from reporting incidents. The goal of the form is to enhance safety and quality of care, not to punish staff.
- All sections of the form must be filled out completely. While providing as much detail as possible is important, it is understood that not every field may apply to every incident. Only fill out what is relevant.
- You cannot seek help when completing the form. Some believe that they must fill out the form independently. It is encouraged to collaborate with supervisors or designated personnel for assistance if needed.
- Lack of a negative outcome means no need for a report. A common myth is that if a patient was not harmed, there is no obligation to report. Incidents may still indicate systemic issues that require attention.
- This form is for internal use only. Some assume the form stays within the organization. In fact, proper reporting may require sharing relevant information with external bodies for compliance and safety improvement.
- The process is solely about blame. There’s a misconception that this form focuses on assigning blame to individuals. In truth, it’s designed as a tool for learning and prevention to enhance patient safety and care.
Being aware of these misconceptions can help staff use the Clinical Incident Report Sample form effectively, ultimately benefiting patient care protocols and safety outcomes.
Key takeaways
When filling out and using the Clinical Incident Report Sample form, keep the following key takeaways in mind to ensure proper reporting and compliance:
- The form is designed for reporting any unexpected incidents related to patient care, even without adverse outcomes.
- Ensure accuracy by providing complete identification details of the person affected, including their name, date of birth, and hospital details.
- Clearly document the nature of the incident by checking all applicable boxes, which helps categorize the event effectively.
- Include a factual summary of the incident without personal opinions to maintain objectivity and integrity in your report.
- After completing the form, return it to FASTAFF via fax at 888-928-3050 as required.
- It is crucial to document any actions taken as a result of the incident, regardless of whether additional sheets are needed.
- Lastly, ensure the employee acknowledges the accuracy of the report by signing and dating the acknowledgment section.
Browse Other Templates
Mv3617 Order for Ignition Interlock Exemptions - Defendants may need to attend court hearings to discuss their situation further.
Child Support Direct Deposit Authorization,Electronic Child Support Payment Form,Child Support EFT Enrollment,Custodial Parent Payment Setup,Child Support Payment Electronic Authorization,Direct Deposit Request for Child Support,Authorization for Ele - All custodial parents are encouraged to consider electronic deposits for convenience and reliability.