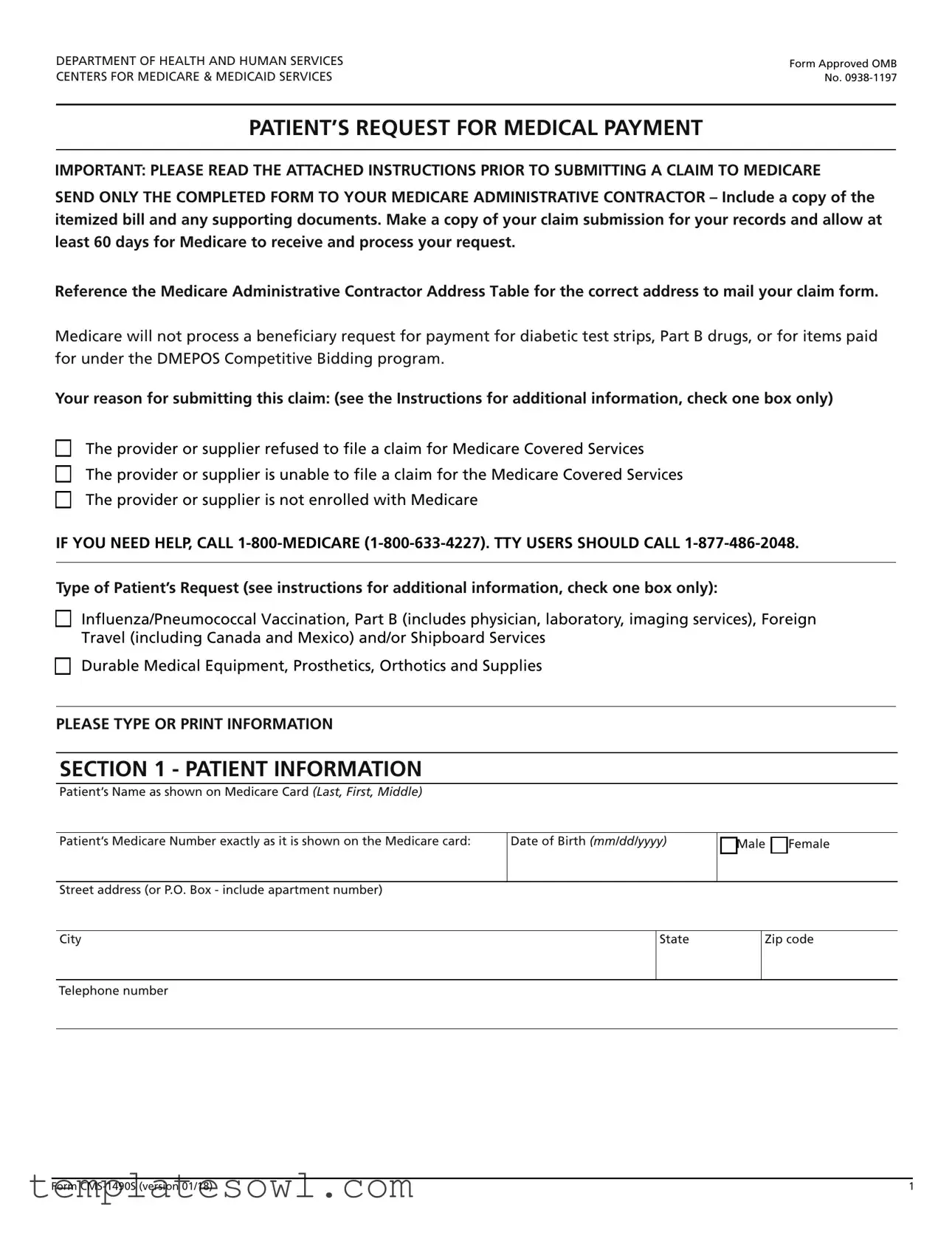
Fill Out Your Cms 1490S Form
The CMS 1490S form, officially titled "Patient's Request for Medical Payment," serves as a critical mechanism for Medicare beneficiaries to seek reimbursement for medical services received when their healthcare provider has not filed a claim on their behalf. This document facilitates the claim submission process, allowing individuals to detail their treatment, provide necessary documentation, and explain the reasons for their request. Key sections of the form include patient information, the nature of the services rendered, and additional health insurance details if applicable. Beneficiaries must submit an itemized bill alongside the form, including specific data such as the date of service, provider details, and a clear description of the illness or injury treated. Notably, the form outlines scenarios where Medicare payment may not be possible, such as for certain items like diabetic test strips or services covered under the DMEPOS Competitive Bidding program. Moreover, it highlights the importance of accurate and complete information to avoid claim denial, thereby emphasizing the need for meticulous attention to detail in its completion. The instructions also specify that the form, along with the attached documents, must be sent directly to one's Medicare Administrative Contractor, ensuring that the claim reaches the appropriate entity for processing. For those needing assistance, resources are made available, including a dedicated helpline to guide them through the submission process.
Cms 1490S Example
DEPARTMENT OF HEALTH AND HUMAN SERVICES |
Form Approved OMB |
CENTERS FOR MEDICARE & MEDICAID SERVICES |
No. |
PATIENT’S REQUEST FOR MEDICAL PAYMENT
IMPORTANT: PLEASE READ THE ATTACHED INSTRUCTIONS PRIOR TO SUBMITTING A CLAIM TO MEDICARE
SEND ONLY THE COMPLETED FORM TO YOUR MEDICARE ADMINISTRATIVE CONTRACTOR – Include a copy of the itemized bill and any supporting documents. Make a copy of your claim submission for your records and allow at least 60 days for Medicare to receive and process your request.
Reference the Medicare Administrative Contractor Address Table for the correct address to mail your claim form.
Medicare will not process a beneficiary request for payment for diabetic test strips, Part B drugs, or for items paid for under the DMEPOS Competitive Bidding program.
Your reason for submitting this claim: (see the Instructions for additional information, check one box only)
The provider or supplier refused to file a claim for Medicare Covered Services
The provider or supplier is unable to file a claim for the Medicare Covered Services
The provider or supplier is not enrolled with Medicare
IF YOU NEED HELP, CALL
Type of Patient’s Request (see instructions for additional information, check one box only):
Influenza/Pneumococcal Vaccination, Part B (includes physician, laboratory, imaging services), Foreign Travel (including Canada and Mexico) and/or Shipboard Services
Durable Medical Equipment, Prosthetics, Orthotics and Supplies
PLEASE TYPE OR PRINT INFORMATION
SECTION 1 - PATIENT INFORMATION
Patient’s Name as shown on Medicare Card (Last, First, Middle)
Patient’s Medicare Number exactly as it is shown on the Medicare card: |
Date of Birth (mm/dd/yyyy) |
Male |
Female |
||
|
|
|
|||
|
|
|
|
|
|
Street address (or P.O. Box - include apartment number) |
|
|
|
|
|
|
|
|
|
|
|
City |
|
State |
|
Zip code |
|
|
|
|
|
|
|
Telephone number |
|
|
|
|
|
|
|
|
|
|
|
Form |
1 |
SECTION 2 - INFORMATION ABOUT SERVICES FURNISHED
FOR ALL CLAIMS including Influenza and Pneumococcal Vaccinations, describe the illness or injury for which you received treatment.
Attach all supporting documentation to the form including an itemized bill with the following information:
•Date of service
•Place of service
•Description of illness or injury
•Description of each surgical or medical service or supply furnished
•Charge for each service
•The doctor’s or supplier’s name and address
•The provider or supplier’s National Provider Identifier (NPI) If known
IMPORTANT: If the itemized bill is from:
•A Clinical laboratory for ordered tests
•An independent diagnostic imaging center for ordered imaging procedures
•A supplier of Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) for ordered DMEPOS
The ordering & referring providers legal name MUST be included on the itemized bill.
Please also include the ordering & referring providers National Provider Identifier (NPI) if known.
Was the condition related to:

 Yes
Yes
 No Employment
No Employment
Yes
 No Auto Accident
No Auto Accident
Yes
 No Treatment for chronic dialysis or kidney transplant
No Treatment for chronic dialysis or kidney transplant
Yes
 No Other Accident
No Other Accident
SECTION 3 - INFORMATION ABOUT HEALTH INSURANCE OTHER THAN MEDICARE
Complete this section if you are age 65 or older and enrolled in a health insurance plan where you or your spouse are currently working and covered by any medical coverage other than Medicare.
Yes |
No |
Are you employed and covered under an employee health plan? |
|
|
|
Yes |
No |
Is your spouse employed and are you covered under your spouse’s employee health plan? |
|
|
|
Yes |
No |
Do you have any medical coverage other than Medicare, such as private insurance, MEDIGAP, employment related insurance, |
|
|
Medicaid,or the Veterans Administration (VA)? |
Name of other Medical Insurance
Policy Number including Medicaid ID Number
Policyholder’s Name (Last, First, Middle)
Street Address (or P.O. Box) of other Medical Insurance
City
State
Zip code
Please attach a copy of your primary insurer’s Explanation of Benefits if Medicare is secondary.
Form |
2 |
SECTION 4 - SIGNATURE
I declare under penalty of perjury that I have examined all the information on this form, and on any accompanying statements or forms, and it is true and correct to the best of my knowledge. Anyone who misrepresents or falsifies essential information requested by this form may upon conviction be subject to fine and imprisonment under Federal law.
I authorize any holder of medical or other information about me to release it to the Centers for Medicare & Medicaid Services or its designated contractor or the Social Security Administration for this Medicare claim. I permit a copy of this authorization to be used in place of the original, and request payment of medical insurance benefits to me.
Signature of Patient |
Date Signed (mm/dd/yyyy) |
|
|
If you cannot sign your name, mark an (X) on the signature line. Have a witness sign his/her name next to the “X” and complete the section below.
If signing this form on behalf of a Medicare patient, on the ‘Signature of Patient’ line above, indicate the patient’s name followed by “By” and sign your name. Provide your name, address, and relationship to the patient with a brief explanation why the patient cannot sign.
Name of Witness (Last, First, Middle)
Street Address
City
State
Zip code
Relationship to the Patient
Signature of Witness
Date Signed (mm/dd/yyyy)
Briefly explain why the Patient cannot sign:
Send the completed form and supporting documentation to your Medicare contractor. Reference the Medicare Administrative Contractor Address table for the correct address to mail your claim form. If you still
do not know the address of your Medicare contractor, call
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information
resources, gather the data needed, and complete and review the information collection. If you have any comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Baltimore, Maryland
Form |
3 |

COLLECTION AND USE OF MEDICARE INFORMATION
We are authorized by the Centers for Medicare & Medicaid Services to ask you for information needed in the administration of the Medicare program. Authority to collect information is in section 205(a), 1872 and 1875 of the Social Security Act, as amended.
The information we obtain to complete your Medicare claim is used to identify you and to determine your eligibility. It is also used to decide if the services and supplies you received are covered by Medicare and to insure that proper payment is made.
The information may also be given to other providers of services, Medicare Administrative Contractor (MAC), medical review boards, and other organizations as necessary to administer the Medicare program. For example, it may be necessary to disclose information to a hospital or doctor about the Medicare benefits you have used.
With one exception, which is discussed below, there are no penalties under Social Security law for refusing to supply information. However, failure to furnish information regarding the medical services rendered or the amount charged would prevent payment of the claim. Failure to furnish any other information, such as name or Medicare number, would delay payment of the claim.
It is mandatory that you tell us if you are being treated for a work related injury so we can determine whether worker’s compensation will pay for the treatment. Section 1877(a)(3) of the Social Security Act provides criminal penalties for withholding this information. If you are being treated for a work related injury be sure to check the appropriate box in Section 2 titled ‘Condition Related to’.
Physicians and other suppliers, such as clinical laboratories, imaging service suppliers, and durable medical equipment suppliers are required by law to submit a claim for Medicare covered services furnished to you, the Medicare beneficiary, within one year of the date of service.
To reduce your
For a list of participating Medicare enrolled physicians in your area, please go to www.medicare.gov/physiciancompare or call
If a physician or supplier furnishes Medicare covered services to you and refuses to submit a claim on your behalf for those services, please call
When you submit your own claim to Medicare, complete the entire form. If the claim form has incomplete or invalid information, the Medicare contractor will return the claim along with a letter to you clearly stating what information is missing or invalid.
If the Patient is deceased, please contact your Social Security office for instructions on how to file a claim.
NOTICE: Anyone who misrepresents or falsifies essential information requested by this form may upon conviction be subject to fine and imprisonment under Federal law. No Part B Medicare benefits may be paid unless this form is received as required by existing law and regulations (20 CFR 422.510).
Form |
4 |

INSTRUCTIONS
READ BEFORE SUBMITTING A CLAIM TO MEDICARE
(PLEASE RETURN ONLY THE FORM AND NOT THE INSTRUCTION)
Patient’s Request for Medical Payment for the Influenza/Pneumococcal Vaccinations, Part B Services, (includes physician, laboratory, imaging services), Durable Medical Equipment, Prosthetics, Orthotics and Supplies, Foreign Travel (including Canada and Mexico) and Shipboard Services
Influenza and Pneumococcal Vaccination:
Medicare may pay for seasonal influenza and pneumococcal vaccinations. Annual Part B deductible and coinsurance amounts do not apply. Medicare does not pay for the hepatitis B vaccines. All physicians,
Part B Services:
In most situations, your physician, other practitioner or supplier will submit your claim to Medicare, if they do not, you can submit a claim.
Durable Medical Equipment, Prosthetics, Orthotics and Supplies:
In most situations, your supplier of DMEPOS will submit your claim to Medicare, if they do not, you can submit a claim for an item or services furnished by this supplier.
Foreign Travel (including Canada and Mexico):
Medicare law prohibits payment for health care services furnished outside the United States (U.S.) except in certain limited circumstances. The term “outside the U.S.” means anywhere other than the 50 states of the U.S., the District of Columbia, Puerto Rico, the U.S. Virgin Islands, Guam, American Samoa, and the Northern Mariana Islands.
Services furnished on a ship in a U.S. port or within 6 hours of when the ship arrived at or departed from a U.S. port are furnished inside the U.S.
There are three situations when Medicare may pay for certain types of health care services rendered in a foreign hospital (a hospital outside the U.S.):
1.You’re in the U.S. when you have a medical emergency and the foreign hospital is closer than the nearest U.S. hospital that can treat your illness or injury.
2.You’re traveling through Canada without unreasonable delay by the most direct route between Alaska and another state when a medical emergency occurs, and the Canadian hospital is closer than the nearest U.S. hospital that can treat your illness or injury. Medicare determines what qualifies as “without unreasonable delay” on a
3.You live in the U.S. and the foreign hospital is closer to your home than the nearest U.S. hospital that can treat your medical condition, regardless of whether it’s an emergency.
In these situations, Medicare will pay for the
Shipboard Services:
Medicare may pay for medically necessary services furnished on a ship in a U.S. port or within 6 hours of when the ship arrived at or departed from a U.S. port only if all of the following requirements are met:
•You have Part B benefits
•The physician is legally authorized to practice in the U.S.
If the ship is more than 6 hours away from a U.S. port, Medicare can pay for medically necessary services only if all of the following requirements are met:
1.You have a medical emergency within 6 hours of departing or arriving at a U.S. port that requires inpatient hospital services.
2.The nearest or most accessible hospital that can treat you is a foreign hospital rather than a U.S. hospital.
3.The services are to treat the emergency illness or injury.
4.You have Part B benefits.
5.The physician is legally authorized to practice where he or she furnished the services
For shipboard services please include a copy of the ship’s itinerary.
Form |
5 |
THI |
E WITH YOUR CLAIM |

HOW TO FILL OUT THIS MEDICARE FORM
Medicare may pay you directly when you complete this form and attach an itemized bill from your doctor or supplier. Mail your completed claim form to the Medicare contractor responsible for processing your claim. If you need additional assistance, call
You have the right to get Medicare information in an accessible format, like large print, Braille, or audio. You also have the right to file a complaint if you believe you’ve been discriminated against. Visit https://www.medicare.gov/
FOLLOW THESE INSTRUCTIONS CAREFULLY:
A. Your Reason for submitting this Claim
Check the box that applies to this claim
B. Type of Patient’s Request
Check only one box that applies to this claim
Section 1 – PATIENT INFORMATION
•Print your name as shown on your Medicare card (Last Name, First Name, Middle Name).
•Print your Medicare Number exactly as it is shown on the Medicare card.
•Print your date of birth (mm/dd/yyyy)
•Check the appropriate box for the patient’s sex.
•Furnish your mailing address and include your telephone number
Section 2 – INFORMATION ABOUT SERVICES FURNISHED
•Describe the illness or injury for which you received treatment
•Patient’s Condition related to: Check the appropriate boxes
NOTE: You must attach an itemized bill in order for Medicare to process this claim.
Attach all supporting documentation to the form including an itemized bill with the following information:
•Date of service
•Place of service
•Description of illness or injury
•Description of each surgical or medical service or supply furnished
•Charge for each service
•The doctor’s or supplier’s name and address
•The provider or supplier’s National Provider Identifier (NPI) If known
•The ordering & referring Providers Full Legal Name and address if required as indicated in Section 2
•It is helpful if the diagnosis is shown on the physician’s itemized bill. If not, be sure you have completed Section 2 of this form.
•Many times a bill will show the names of several doctors or suppliers. It is very important the provider who treated you be identified. Simply circle his/her name on the bill.
•Mark out any services on the itemized bill(s) you are attaching for which you have already filed a Medicare claim.
•Attach a copy of your primary insurer’s Explanation of Benefits notice if you are requesting Medicare Secondary payment.
•Shipboard services please include a copy of the ship’s itinerary.
Section 3 – INFORMATION ABOUT HEALTH INSURANCE OTHER THAN MEDICARE
•Complete this Section if you are age 65 or older and enrolled in a health insurance plan where you or your spouse are currently working and if you have any medical coverage other than Medicare.
•Check all boxes that apply
Section 4 – SIGNATURE
Sign your name and date the form
•Name of other Medical Insurance
•Policy Number including Medicaid ID Number
•Policyholder’s Name
•Street Address of other Medical Insurance
If the Medicare beneficiary is not able to sign his/her name, follow the instructions on the form.
Form |
6 |

MEDICARE ADMINISTRATIVE CONTRACTOR ADDRESS TABLE
FOR INFLUENZA/PNEUMOCOCCAL VACCINATION, PART B (INCLUDES PHYSICIAN, LABORATORY, IMAGING SERVICES)
If you received a |
Mail your claim form, itemized bill and supporting documents to: |
|
service in: |
|
|
|
|
|
Alabama |
Palmetto GBA, LLC |
|
|
Mail Code: |
|
|
P.O. Box 100306 |
|
|
Columbia, SC |
|
|
|
|
Alaska |
Noridian Healthcare Solutions, LLC |
|
|
P.O. Box 6703 |
|
|
Fargo, ND |
|
|
|
|
American Samoa |
Noridian Healthcare Solutions, LLC |
|
|
P.O. Box 6777 |
|
|
Fargo, ND |
|
|
|
|
Arkansas |
Novitas Solutions, Inc. |
|
|
P.O. Box 3098 |
|
|
Mechanicsburg, PA |
|
|
(Address to send Medicare 1490 claims via Priority mail or through a commercial courier |
|
|
(UPS, FedEx) for which a PO Box cannot be used, please use the following street address: |
|
|
Novitas Solutions, Inc. |
|
|
Attention: Claims Department |
|
|
2020 Technology Parkway, Suite 100 |
|
|
Mechanicsburg, PA 17050 |
|
|
|
|
Arizona |
Noridian Healthcare Solutions , LLC |
|
|
P.O. Box 6704 |
|
|
Fargo, ND |
|
|
|
|
California Northern |
Noridian Healthcare Solutions |
|
(For Part B) |
P.O. Box 6774 |
|
|
SEND |
|
|
Fargo, |
|
California Southern |
Noridian Healthcare Solutions, LLC |
|
(For Part B) |
P.O. Box 6775 |
|
|
Fargo, ND |
|
|
|
|
Colorado |
Novitas Solutions |
|
|
P. . Box 3107 |
|
|
Mechanicsburg, PA |
|
|
(Address to send Medicare 1490 claims via Priority mail or through a |
|
|
commercial courier (UPS, FedEx) for which a PO Box cannot be used, please use the |
|
|
following street address: |
|
|
Novitas Solutions, Inc. |
|
|
Attention: Claims Department |
|
|
2020 Technology Parkway, Suite 100 |
|
|
Mechanicsburg, PA 17050 |
|
|
|
|
Connecticut |
National Government Services, Inc. |
|
|
P.O. Box 6178 |
|
|
Indianapolis, IN |
|
|
|
|
Delaware |
Novitas Solutions |
|
|
P.O. Box 3397 |
|
|
Mechanicsburg, PA |
|
|
|
|
District of Columbia |
Novitas Solutions |
|
|
P.O. Box 3396 |
|
|
Mechanicsburg, PA |
|
|
|
|
Form |
7 |
MEDICARE ADMINISTRATIVE CONTRACTOR ADDRESS TABLE
FOR INFLUENZA/PNEUMOCOCCAL VACCINATION, PART B (INCLUDES PHYSICIAN, LABORATORY, IMAGING SERVICES)
If you received a |
Mail your claim form, itemized bill and supporting documents to: |
service in: |
|
|
|
Florida |
First Coast Service Options, Inc. |
|
P.O. Box 2525 |
|
Jacksonville, FL |
|
|
Georgia |
Palmetto GBA, LLC |
|
Mail Code: |
|
P.O. Box 100306 |
|
Columbia, SC |
|
|
Guam |
Noridian Healthcare Solutions, LLC |
|
P.O. Box 6777 |
|
Fargo, ND |
|
|
Hawaii |
Noridian Healthcare Solutions, LLC |
|
P.O. Box 6777 |
|
Fargo, ND |
|
|
Idaho |
Noridian Healthcare Solutions, LLC |
|
P.O. Box 6701 |
|
Fargo, ND |
|
|
Illinois |
National Government Services, Inc. |
|
P.O. Box 6475 |
|
Indianapolis, IN |
|
|
Indiana |
Wisconsin Physicians Service |
|
P.O. Box 8940 |
|
Madison, WI |
|
|
Iowa |
Wisconsin Physicians Service |
|
P.O. Box 8550 |
|
Madison, WI |
|
|
Kansas |
Wisconsin Physicians Service |
|
P.O. Box 7238 |
|
NOT |
|
Madison, WI |
Kentucky |
CGS Administrators, LLC |
|
P. . Box 20019 |
|
Nashville, TN 37202 |
|
|
Louisiana |
Novitas Solutions, Inc. |
|
P.O. Box 3097 |
|
Mechanicsburg, PA |
|
(Address to send Medicare 1490 claims via Priority mail or through a commercial courier |
|
(UPS, FedEx) for which a PO Box cannot be used, please use the following street address: |
|
Novitas Solutions, Inc. |
|
Attention: Claims Department |
|
2020 Technology Parkway, Suite 100 |
|
Mechanicsburg, PA 17050 |
|
|
Maine |
National Government Services, Inc. |
|
P.O. Box 6178 |
|
Indianapolis, IN |
|
|
Form |
8 |

MEDICARE ADMINISTRATIVE CONTRACTOR ADDRESS TABLE
FOR INFLUENZA/PNEUMOCOCCAL VACCINATION, PART B (INCLUDES PHYSICIAN, LABORATORY, IMAGING SERVICES)
If you received a |
Mail your claim form, itemized bill and supporting documents to: |
service in: |
|
|
|
Maryland |
Novitas Solutions, Inc. |
|
P.O. Box 3398 |
|
Mechanicsburg, PA |
|
(Address to send Medicare 1490 claims via Priority mail or through a commercial courier |
|
(UPS, FedEx) for which a PO Box cannot be used, please use the following street address: |
|
Novitas Solutions, Inc. |
|
Attention: Claims Department |
|
2020 Technology Parkway, Suite 100 |
|
Mechanicsburg, PA 17050 |
|
|
Massachusetts |
National Government Services, Inc. |
|
P.O. Box 6178 |
|
Indianapolis, IN |
|
|
Michigan |
Wisconsin Physicians Service |
|
P.O. Box 8987 |
|
Madison, WI |
|
|
Minnesota |
National Government Services, Inc. |
|
P.O. Box 6475 |
|
Indianapolis, IN |
|
|
Mississippi |
Novitas Solutions |
|
P.O. Box 3129 |
|
Mechanicsburg, PA |
|
(Address to send Medicare 1490 claims via Priority mail or through a commercial courier |
|
(UPS, FedEx) for which a PO Box cannot be used, please use the following street address: |
|
Novitas Solutions, Inc. |
|
Attention: Claims Department |
|
2020 Technology Parkway, Suite 100 |
|
Mechanicsburg, PA 17050 |
|
|
Missouri |
Wisconsin Physicians Service |
|
P. . Box 14260 |
|
Madison, WI |
|
|
Montana |
Noridian Healthcare Solutions, LLC |
|
P.O. Box 6735 |
|
Fargo, ND |
|
|
Nebraska |
Wisconsin Physicians Service |
|
P.O. Box 8667 |
|
Madison, WI |
|
|
Nevada |
Noridian Healthcare Solutions, LLC |
|
P.O. Box 6776 |
|
Fargo, ND |
|
|
New Hampshire |
National Government Services, Inc. |
|
P.O. Box 6178 |
|
Indianapolis, IN |
|
|
Form |
9 |
MEDICARE ADMINISTRATIVE CONTRACTOR ADDRESS TABLE
FOR INFLUENZA/PNEUMOCOCCAL VACCINATION, PART B (INCLUDES PHYSICIAN, LABORATORY, IMAGING SERVICES)
If you received a |
|
Mail your claim form, itemized bill and supporting documents to: |
service in: |
|
|
|
|
|
New Jersey |
|
Novitas Solutions |
|
|
P.O. Box 3030 |
|
|
Mechanicsburg, PA |
|
|
(Address to send Medicare 1490 claims via Priority mail or through a commercial courier |
|
|
(UPS, FedEx) for which a PO Box cannot be used, please use the following street address: |
|
|
Novitas Solutions, Inc. |
|
|
Attention: Claims Department |
|
|
2020 Technology Parkway, Suite 100 |
|
|
Mechanicsburg, PA 17050 |
|
|
|
New Mexico |
|
Novitas Solutions |
|
|
P.O. Box 3107 |
|
|
Mechanicsburg, PA |
|
|
(Address to send Medicare 1490 claims via Priority mail or through a commercial courier |
|
|
UPS, FedEx) for which a PO Box cannot be used,please use the following street address: |
|
|
Novitas Solutions, Inc. |
|
|
Attention: Claims Department |
|
|
2020 Technology Parkway, Suite 100 |
|
|
Mechanicsburg, PA 17050 |
|
|
|
New York |
|
National Government ervices, Inc. |
|
|
P.O. Box 6178 |
|
|
Indianapolis, IN |
|
|
|
North Carolina |
|
Palmetto GBA, LLC |
|
|
Mail Code: |
|
|
P.O. Box 100190 |
|
|
Columbia, SC |
|
|
|
North Dakota |
|
Noridian Healthcare Solutions, LLC |
|
|
P.O. Box 6706 |
|
|
Fargo, ND |
|
|
|
Northern Mariana |
Noridian Healthcare Solutions |
|
Islands |
NOTP. . Box 6777 |
|
|
|
Fargo, ND |
|
|
|
Ohio |
|
CGS Administrators, LLC |
|
|
P.O. Box 20019 |
|
|
Nashville, TN 37202 |
|
|
|
Oklahoma |
|
Novitas Solution |
|
|
P.O. Box 3107 |
|
|
Mechanicsburg, PA |
|
|
(Address to send Medicare 1490 claims via Priority mail or through a commercial courier |
|
|
(UPS, FedEx) for which a PO Box cannot be used, please use the following street address: |
|
|
Novitas Solutions, Inc. |
|
|
Attention: Claims Department |
|
|
2020 Technology Parkway, Suite 100 |
|
|
Mechanicsburg, PA 17050 |
|
|
|
Oregon |
|
Noridian Healthcare Solutions |
|
|
P.O. Box 6702 |
|
|
Fargo, ND |
|
|
|
Form |
10 |
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The CMS 1490S form is used by patients to request medical payment from Medicare for services that were not directly submitted by their medical provider. |
| Submission Guidelines | To process the claim, the form must be completed in full and submitted alongside an itemized bill and any supporting documents. It's crucial to send these to the appropriate Medicare Administrative Contractor address. |
| Item Restrictions | Medicare will not process claims for certain items, including diabetic test strips and services covered under the DMEPOS Competitive Bidding program. |
| Governing Law | This form is governed by the regulations set forth in the Social Security Act, specifically sections 205(a), 1872, and 1875. |
Guidelines on Utilizing Cms 1490S
Completing the CMS-1490S form accurately is essential for receiving medical payment from Medicare. Ensure that you gather all necessary documentation before you start filling out the form. This will help streamline the process and avoid any delays in processing your claim.
- Section 1 – Patient Information: Fill in your name as it appears on your Medicare card. Include your Medicare number, date of birth, sex, address, city, state, zip code, and phone number.
- Section 2 – Information About Services Furnished: Describe the illness or injury for which you received treatment. Attach an itemized bill that includes:
- Date of service
- Place of service
- Description of illness or injury
- Details of each surgical or medical service provided
- Charge for each service
- Provider’s or supplier’s name and address
- Provider’s National Provider Identifier (NPI), if known
- Indicate if the condition was related to employment, auto accidents, chronic dialysis or kidney transplant, or other accidents.
- Section 3 – Information About Health Insurance: If applicable, answer whether you or your spouse are covered under an employee health plan or have any other medical coverage. Provide the required information for the other insurance policy.
- Section 4 – Signature: Sign and date the form. If you cannot sign, mark an 'X'. Have a witness sign next to the 'X', and provide their information and your explanation for not signing.
- Documentation: Ensure that you include all supporting documents, such as the itemized bill and any explanations from other insurers if Medicare is secondary.
- Submission: Send the completed form along with the supporting documents to the correct Medicare Administrative Contractor address as referenced in the instructions. Retain a copy for your records.
Once submitted, allow at least 60 days for Medicare to process your claim. If you have questions or need assistance during the process, contacting Medicare directly can provide valuable support.
What You Should Know About This Form
What is the CMS 1490S form?
The CMS 1490S form is a document used by Medicare beneficiaries to request medical payment for services covered under Medicare. This includes treatments such as influenza and pneumococcal vaccinations, certain medical services, and supplies. The form needs to be completed and sent to the Medicare Administrative Contractor along with an itemized bill and supporting documents.
Who needs to fill out the CMS 1490S form?
Any Medicare beneficiary who has received covered medical services but whose provider or supplier has refused or is unable to submit the claim on their behalf needs to fill out the CMS 1490S form. This may also apply if the provider is not enrolled in Medicare.
What should be included with the CMS 1490S form when submitting a claim?
When submitting a claim using the CMS 1490S form, you must include the completed form, a copy of your itemized bill, and any relevant supporting documents. The itemized bill should include details like the date of service, place of service, description of the illness or injury, services rendered, charges for each service, and the provider’s name and National Provider Identifier (NPI), if known.
How long does it take for Medicare to process a claim submitted via the CMS 1490S form?
Once you submit your claim, allow at least 60 days for Medicare to receive and process it. Processing times may vary, so it's important to keep a record of your submission.
What happens if the CMS 1490S form is incomplete or invalid?
If the form is submitted with incomplete or invalid information, the Medicare contractor will return the claim to you. Along with the returned claim, you will receive a letter stating what information is missing or why the claim is invalid. Make sure to double-check everything before sending it in to avoid delays.
Is there any specific information required on the itemized bill?
Yes, the itemized bill must include specific details. It should have the date of service, place of service, a description of the illness or injury, each medical service or supply furnished, the charge for each service, and the provider or supplier's name and NPI. If from certain types of providers, such as labs or DMEPOS suppliers, the ordering and referring providers’ names and NPIs must also be included.
Can I submit a claim for services received outside the United States?
Submitting a claim for services received outside the United States is possible under certain conditions. If you received emergency care in a foreign hospital when a U.S. hospital was not accessible, or if you are traveling through Canada en route to Alaska, Medicare may cover some of those services. Specific documentation must be provided, so it's essential to review the requirements carefully.
What should I do if I am unable to sign the form?
If you are unable to sign the form, you can mark an ‘X’ on the signature line. A witness must then sign their name next to the ‘X’. Additionally, you must provide the witness's name, address, and relationship to you, along with a brief explanation of why you cannot sign.
What should I do if the provider does not file a claim on my behalf?
If your provider refuses to file a claim for Medicare-covered services, you have the right to submit your own claim using the CMS 1490S form. It’s encouraged to reach out to Medicare at 1-800-MEDICARE (1-800-633-4227) for assistance, especially if the provider continues to deny your request for them to file on your behalf.
Where do I send the completed CMS 1490S form?
The completed CMS 1490S form should be sent to your designated Medicare Administrative Contractor. The specific address to send your claim can be found in the Medicare Administrative Contractor Address Table. If you are uncertain about the correct address, you can call 1-800-MEDICARE for assistance.
Common mistakes
Filling out the CMS 1490S form can be challenging, and several common mistakes may lead to delays or denials in processing claims. One frequent error occurs when individuals fail to provide complete patient information. This includes not listing the patient's name exactly as it appears on their Medicare card or omitting vital details like the patient's Medicare number and date of birth. Incomplete information can cause the claim to be returned, resulting in frustrating delays.
Another mistake is related to missing documentation. Claimants often forget to include the required itemized bills and supporting documents. Every claim must be backed with accurate details, such as the date of service, description of the illness or injury, and charges for services provided. Without these documents, Medicare may be unable to verify the claim, leading to a denial.
Additionally, selecting the wrong type of request can significantly impact the claim's outcome. The form requires claimants to check only one box regarding the reason for submission and the type of request. Confusion over which category to select can lead to inappropriate processing, particularly for non-covered services like diabetic test strips.
Many also overlook the importance of disclosing other health insurance coverage. If a person is age 65 or older and has medical coverage from an employer or other sources, this must be reported on the form. Failure to do so can result in Medicare not paying for the claim, as they may not cover services that should be billed to another insurer first.
Lastly, individuals frequently neglect the signature section. The form must be signed by the patient or their representative. If the patient is unable to sign, it's crucial to have a witness sign next to the "X" and provide an explanation. An unsigned or improperly signed form will cause the claim to be returned, further delaying the process.
Documents used along the form
When submitting a claim using the CMS 1490S form, it's important to understand the additional forms and documents that may be required. These documents help provide further context and necessary information for the claim, ensuring a smoother review process by Medicare. The following is a list of important documents to consider when filing your claim.
- Itemized Bill: This document provides a detailed account of the medical services rendered. Include specific information such as the date of service, place of service, and description of each service. This is essential for Medicare to validate your claim.
- Explanation of Benefits (EOB): If you have other insurance coverage besides Medicare, the EOB from that insurer outlines what was covered and what amounts are owed. This is critical for processing as it shows Medicare how to coordinate benefits.
- Doctor's National Provider Identifier (NPI): This unique identification number is tied to healthcare providers. If known, including the NPI on your claim helps to streamline the approval process.
- Medical Records: In some cases, Medicare may request additional medical documentation. Records that establish the treatment you received, such as physicians' notes or lab results, can support your claim.
- Proof of Payment: Receipts or other documentation showing that payment has been made for the service can be required. This helps confirm that you have incurred an expense that needs to be reimbursed by Medicare.
- Power of Attorney (if applicable): If someone else is submitting the claim on your behalf, a Power of Attorney document is needed to show their authority to act in your name, ensuring all procedures align with legal protocols.
Being prepared with these documents can significantly improve the chances of your claim being processed efficiently. Ensure each document is filled out correctly and submitted alongside your CMS 1490S form to avoid delays in reimbursement.
Similar forms
- CMS-1500 Form: This form is used by healthcare providers to bill Medicare and other insurers for services provided. Like the CMS-1490S, it requires detailed information about the patient and the services rendered.
- UB-04 Form: Similar to the CMS-1500, this form is used for hospital billing. It captures detailed information about inpatient and outpatient services, making it equivalent to CMS-1490S in terms of final claims submission.
- CMS-855I Form: This application form is used for enrolling as a Medicare provider. While it serves a different purpose than CMS-1490S, both documents involve verifying information to facilitate Medicare claims.
- CMS-27 Form: This form is used specifically for requesting Medicare coverage for specific items or services. It parallels the CMS-1490S in its intent to seek payment from Medicare.
- 86210 Form: This document is utilized for submitting claims for durable medical equipment (DME). Similar to the CMS-1490S, it focuses on reimbursement for necessary medical supplies.
- HCFA 1491 Form: This form is a request for payment for outpatient hospital services. Like CMS-1490S, it is focused on submitting claims to Medicare for reimbursement.
- CMS-421 Form: It is used for assigning and verifying patient information related to Medicare enrollment, sharing a common goal with the CMS-1490S in ensuring accurate records for claims.
- Medicaid Claim Form: This form is used to request payment for health services provided to Medicaid beneficiaries. It serves a similar role in claims submission, akin to the CMS-1490S.
- Patient Financial Assistance Application: While not a direct Medicare claim, this form is used to seek financial help based on patient needs, paralleling the CMS-1490S in supporting patient healthcare access.
Dos and Don'ts
Here are some essential tips for filling out the CMS 1490S form:
- Do: Read the attached instructions thoroughly before submitting your claim.
- Don't: Forget to include an itemized bill with detailed information about your services.
- Do: Ensure all patient information, such as name and Medicare number, exactly matches what is on the Medicare card.
- Don't: Leave any sections of the form incomplete. Every section is important for processing your claim.
- Do: Make a copy of the completed form and supporting documents for your records.
- Don't: Submit claims for items that are not covered by Medicare, such as diabetic test strips.
- Do: Allow at least 60 days for Medicare to process your claim before following up.
Misconceptions
Many individuals may hold misconceptions about the CMS 1490S form, which is crucial for submitting claims to Medicare. Understanding these misconceptions can help ensure a smoother claims process.
- The CMS 1490S form is only for a specific type of service. Many believe that this form applies exclusively to particular services such as vaccinations. In fact, it is used for a variety of medical services, including physician visits, laboratory tests, and durable medical equipment claims.
- Only healthcare providers can submit this form. While it is common for providers to submit claims, beneficiaries can also self-submit the form when providers refuse or are unable to file on their behalf.
- Medicare automatically processes all claims submitted on the CMS 1490S. This is not true. The form must be completed accurately and fully, or the claim may be returned for missing or invalid information, causing delays in processing.
- It is unnecessary to include supporting documents. In reality, the claim will require an itemized bill and additional supporting documentation to process properly. Without these, the claim might be rejected.
- Diabetic test strips are covered by this form. Many believe that they can claim diabetic test strips through CMS 1490S. However, this is not permitted as Medicare does not process beneficiary requests for certain items such as these under this form.
- The form can be submitted without checking the required boxes. Claimants must check one box for their reason for submission and for the type of services requested. Omitting this step can lead to denial or delay of the claim.
- It is acceptable to send in the form without reviewing the instructions. Failing to read the attached instructions can lead to mistakes in filling out the form, which may result in a denial of the claim due to improper completion.
- Only older beneficiaries need to use the CMS 1490S form. While it is often utilized by older adults, any individual covered by Medicare can use this form regardless of age, especially when their provider does not file the claim on their behalf.
Awareness of these misconceptions can empower Medicare beneficiaries to navigate the claims process more effectively. Proper understanding can lead to faster resolution of claims and ultimately better access to necessary medical services.
Key takeaways
1. Complete the Form Accurately: When filling out the CMS-1490S form, ensure all sections are complete and accurate. Incomplete or incorrect information may lead to delays or denials in processing your claim.
2. Include Supporting Documentation: Attach an itemized bill and any necessary supporting documents to your claim submission. This documentation should include the date of service, place of service, description of the illness or injury, and the charges for each service.
3. Know What Medicare Covers: Be aware that Medicare does not cover certain items and services, such as diabetic test strips or items included under the DMEPOS Competitive Bidding program. Understanding what is covered can prevent unnecessary claims.
4. Allow Sufficient Processing Time: After submitting your claim, allow at least 60 days for Medicare to process your request. Keep a copy of your submission for your records in case of future inquiries or issues.
Browse Other Templates
Capital One Bank Wire Transfer - Keep a copy of your completed form for your records after submission.
Consent to Release - Consent to Release only permits information access, while Proof of Representation allows action.