Fill Out Your Cms 485 Form
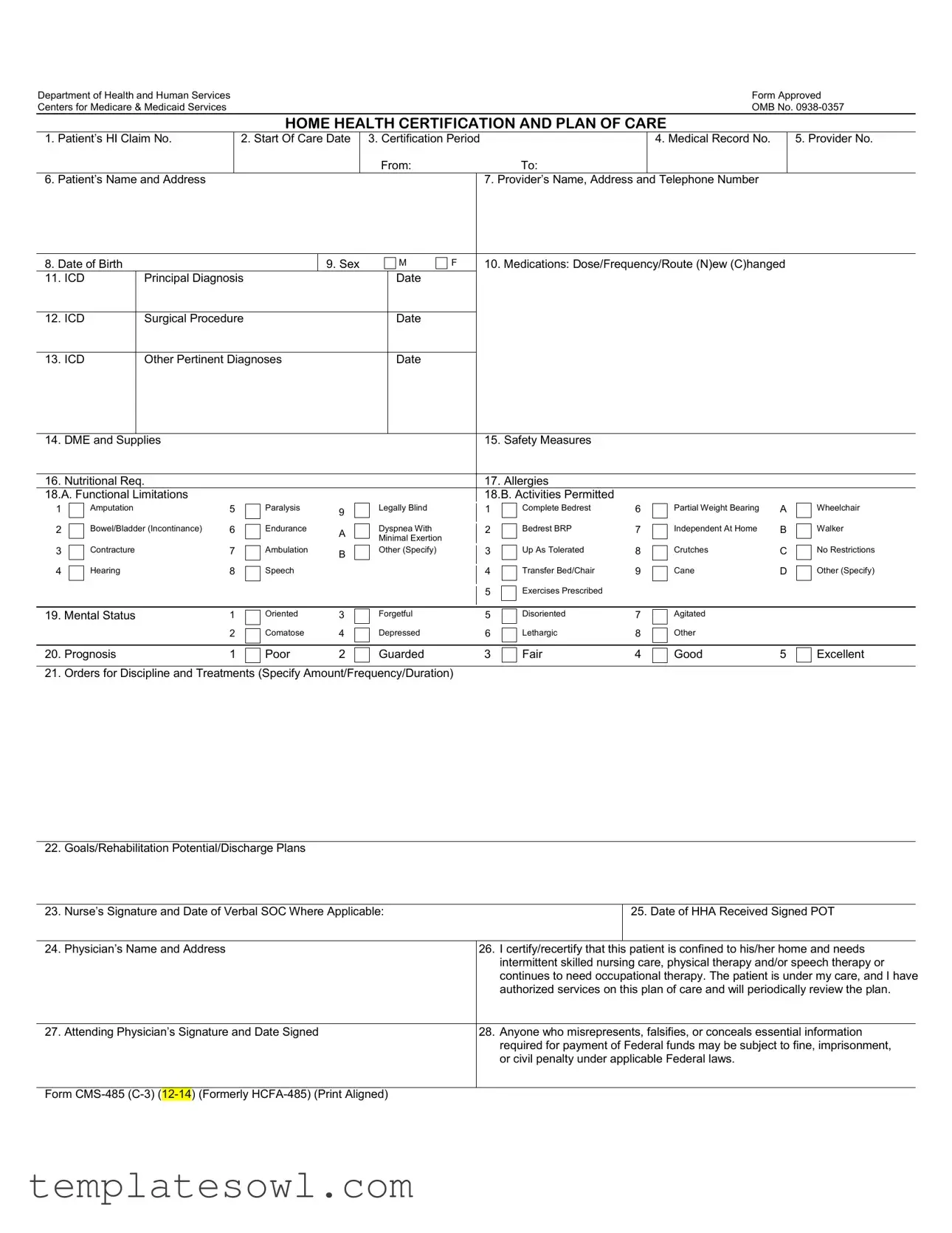
The CMS 485 form, also known as the Home Health Certification and Plan of Care, plays a crucial role in the Medicare system by documenting the medical necessity for home health services. This form is essential for healthcare providers to ensure that patients receive appropriate and necessary care in a home setting. Key components of the CMS 485 include a patient's identification details, such as name, date of birth, and medical record number, as well as information regarding the start of care date and certification period. It highlights the principal diagnosis using ICD codes, documents medications, and outlines any required durable medical equipment (DME) and supplies. Providers must assess and record the patient's functional limitations, mental status, and the prognosis to create a comprehensive treatment plan. Additionally, the form requires signatures and certifications from the attending physician, confirming ongoing need for skilled care. Understanding and accurately completing the CMS 485 form is vital, as any misrepresentation can result in serious legal repercussions and affect eligibility for Medicare benefits.
Cms 485 Example

Department of Health and Human Services |
Form Approved |
Centers for Medicare & Medicaid Services |
OMB No. |
HOME HEALTH CERTIFICATION AND PLAN OF CARE
1. |
Patient’s HI Claim No. |
2. Start Of Care Date |
3. Certification Period |
|
4. Medical Record No. |
5. Provider No. |
|
|
|
From: |
To: |
|
|
6. |
Patient’s Name and Address |
|
|
7. Provider’s Name, Address and Telephone Number |
|
|
8. Date of Birth |
|
9. Sex |
M |
F |
10. Medications: Dose/Frequency/Route (N)ew (C)hanged |
11. ICD |
Principal Diagnosis |
|
Date |
|
|
|
|
|
|
|
|
12. ICD |
Surgical Procedure |
|
Date |
|
|
|
|
|
|
|
|
13. ICD |
Other Pertinent Diagnoses |
|
Date |
|
|
|
|
|
|
|
|
14. |
DME and Supplies |
15. |
Safety Measures |
|
|
|
|
16. |
Nutritional Req. |
17. |
Allergies |
18.A. Functional Limitations |
18.B. Activities Permitted |
||
1
2
3
4
Amputation |
5 |
|
Paralysis |
9 |
|
|
|
|
|
Bowel/Bladder (Incontinance) |
6 |
|
Endurance |
A |
|
||||
|
|
|
|
|
Contracture |
7 |
|
Ambulation |
B |
|
||||
|
|
|
|
|
Hearing |
8 |
|
Speech |
|
|
|
|||
|
|
|
|
|
Legally Blind
Dyspnea With
Minimal Exertion
Other (Specify)
1
2
3
4
5
Complete Bedrest |
6 |
Bedrest BRP |
7 |
Up As Tolerated |
8 |
Transfer Bed/Chair |
9 |
Exercises Prescribed |
|
Partial Weight Bearing |
A |
Independent At Home |
B |
Crutches |
C |
Cane |
D |
Wheelchair
Walker
No Restrictions
Other (Specify)
19. Mental Status |
1 |
Oriented |
3 |
Forgetful |
5 |
Disoriented |
7 |
Agitated |
|
|
|
2 |
Comatose |
4 |
Depressed |
6 |
Lethargic |
8 |
Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
20. Prognosis |
1 |
Poor |
2 |
Guarded |
3 |
Fair |
4 |
Good |
5 |
Excellent |
21. Orders for Discipline and Treatments (Specify Amount/Frequency/Duration)
22. Goals/Rehabilitation Potential/Discharge Plans
23. Nurse’s Signature and Date of Verbal SOC Where Applicable:
25. Date of HHA Received Signed POT
24. |
Physician’s Name and Address |
26. |
I certify/recertify that this patient is confined to his/her home and needs |
|
|
|
|
intermittent skilled nursing care, physical therapy and/or speech therapy or |
|
|
|
|
continues to need occupational therapy. The patient is under my care, and I have |
|
|
|
|
authorized services on this plan of care and will periodically review the plan. |
|
|
|
|
|
|
27. |
Attending Physician’s Signature and Date Signed |
28. |
Anyone who misrepresents, falsifies, or conceals essential information |
|
|
|
|
required for payment of Federal funds may be subject to fine, imprisonment, |
|
|
|
|
or civil penalty under applicable Federal laws. |
|
|
|
|
|
|
Form
Privacy Act Statement
Sections 1812, 1814, 1815, 1816, 1861 and 1862 of the Social Security Act authorize collection of this information. The primary use of this information is to process and pay Medicare benefits to or on behalf of eligible individuals. Disclosure of this information may be made to: Peer Review Organizations and Quality Review Organizations in connection with their review of claims, or in connection with studies or other review activities, conducted pursuant to Part B of Title XI of the Social Security Act; State Licensing Boards for review of unethical practices or nonprofessional conduct; A congressional office from the record of an individual in response to an inquiry from the congressional office at the request of that individual.
Where the individual’s identification number is his/her Social Security Number (SSN), collection of this information is authorized by Executive Order 9397. Furnishing the information on this form, including the SSN, is voluntary, but failure to do so may result in disapproval of the request for payment of Medicare benefits.
Paper Work Burden Statement
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Purpose | The CMS 485 form is used for home health certification and plan of care for patients needing intermittent skilled nursing care or therapy services. |
| Governing Law | This form is governed under the Social Security Act, specifically sections 1812, 1814, 1815, 1816, 1861, and 1862. |
| OMB Control Number | The OMB control number for the CMS 485 form is 0938-0357. |
| Information Collection | Completing the CMS 485 generally takes about 15 minutes, according to the Paperwork Reduction Act of 1995. |
| Patient Information | The form requires essential patient information, including the patient's name, address, date of birth, and medical record number. |
| Provider Details | Healthcare providers must include their name, address, and telephone number on the form. |
| Medications Section | The medications section allows for the documentation of medication doses, frequency, and route, distinguishing new and changed medications. |
| Certification Requirement | Physicians must certify that the patient is homebound and needs intermittent skilled services, and they must periodically review the care plan. |
| Consequences of Misrepresentation | Misrepresentation or falsification of information on this form could lead to fines, imprisonment, or civil penalties under federal laws. |
Guidelines on Utilizing Cms 485
Filling out the CMS 485 form involves several key steps. This is essential for ensuring that the necessary medical information is collected properly for home health services. Accuracy and completeness are crucial throughout the process. Follow the steps below to efficiently complete the form.
- Begin by entering the patient’s HI Claim Number at the top of the form.
- Indicate the Start of Care Date.
- Fill in the Certification Period by recording the From and To dates.
- Enter the Medical Record Number.
- Input the Provider Number.
- Complete the Patient’s Name and Address section.
- Provide the Provider’s Name, Address, and Telephone Number.
- Fill in the Patient’s Date of Birth.
- Select the Patient’s Sex by marking ‘M’ for male or ‘F’ for female.
- List the patient's medications, including Dose/Frequency/Route, and indicate if they are new (N) or changed (C).
- Record the ICD Principal Diagnosis and the date.
- Provide the ICD Surgical Procedure date.
- List other pertinent ICD diagnoses and their respective dates.
- Indicate any DME and supplies needed.
- Detail safety measures to be taken for the patient.
- Specify the patient’s nutritional requirements.
- Document any known allergies.
- Under the functional limitations section, check applicable items that pertain to the patient’s condition.
- In the activities permitted section, select the appropriate options that indicate what the patient can do.
- Assess and mark the patient’s mental status based on the provided scale.
- Provide a prognosis rating from poor to excellent.
- List orders for discipline and treatments, specifying amount, frequency, and duration.
- Outline the goals, rehabilitation potential, and discharge plans.
- Have the nurse sign and date the form where applicable.
- Record the date the Home Health Agency (HHA) received the signed Plan of Treatment (POT).
- Fill in the Physician’s Name and Address.
- Have the attending physician certify/recertify the patient’s eligibility for home care and sign and date the section provided.
- Read the fine print regarding misrepresentation and the consequences associated with it.
What You Should Know About This Form
What is the CMS 485 form?
The CMS 485 form, also known as the Home Health Certification and Plan of Care, is a document used by healthcare providers to certify that a patient requires home health services. It outlines the necessary skilled nursing care, physical therapy, or other treatments required for the patient, and serves as a plan of action for the patient's home healthcare team.
Who needs to complete the CMS 485 form?
The form must be completed by a qualified healthcare provider, typically a physician. They are responsible for assessing the patient's needs and certifying that the individual meets the criteria for receiving home health care services.
What information is required on the CMS 485 form?
The form requires detailed information such as the patient's medical record number, diagnosis, medications, and the type of care required. It also includes personal details, functional limitations, mental status, and discharge plans, which all help to create a comprehensive care plan.
How does the CMS 485 form affect Medicare coverage?
The completion of this form is essential for Medicare coverage of home health services. It certifies that the patient is confined to their home and needs intermittent skilled care. Without this documentation, the request for payment may be denied.
What are the consequences of providing false information on the CMS 485 form?
Providing false or misleading information can lead to serious legal consequences, including fines or imprisonment. It is crucial to ensure that all information is accurate and complete to avoid complications in the payment process.
How often must the CMS 485 form be updated?
The CMS 485 form must be reviewed and updated at least every 60 days. This ensures that the patient's care plan remains relevant and aligned with their current health needs. If there are significant changes in the patient’s condition, an updated form is necessary sooner.
Can patients or their families fill out the CMS 485 form?
No, patients or their families cannot fill out the CMS 485 form. It must be completed by an authorized healthcare provider who can assess the patient’s medical needs and certify the necessity of home health services.
What happens if a patient does not provide their Social Security Number on the CMS 485 form?
While providing a Social Security Number (SSN) is voluntary, not including it may result in disapproval of Medicare benefits. This number is used to accurately process claims and verify patient identity.
How long does it take to complete the CMS 485 form?
The estimated time to complete the CMS 485 form is about 15 minutes. This includes reviewing instructions and gathering necessary information. Overall, it should not take significantly longer if the required data is readily available.
Where can I obtain the CMS 485 form?
The CMS 485 form can be obtained from the Centers for Medicare & Medicaid Services (CMS) website or directly from a healthcare provider’s office that offers home health services. Make sure to use the most up-to-date version of the form.
Common mistakes
Filling out the CMS 485 form correctly is crucial for ensuring that patients receive the home health care they need and that providers are fairly compensated. Yet, many people make common mistakes when completing this important document. Here are ten errors to watch out for.
One frequent mistake is incomplete patient information. A missing patient name, birth date, or address can delay processing and lead to complications. It’s essential to double-check that all fields related to the patient’s identity are filled out accurately.
Another common pitfall is failing to accurately enter the certification period. This section indicates how long the services are needed. If this information is incorrect or missing, it can lead to payment issues and disrupt patient care.
Inaccurate listing of medications is another significant error. It’s vital to note the correct dose, frequency, and route for all medications. Any discrepancies can affect a patient’s treatment plan and put their health at risk.
The use of outdated or incorrect diagnosis codes (ICD codes) often leads to problems. Each diagnosis must be relevant and up-to-date for proper reimbursement. It’s crucial to review the principal and additional diagnoses before submitting the form.
Likewise, neglecting to include required self-care limitations, such as function impairments and permitted activities, is a serious mistake. This information helps tailor the care plan and ensures that all necessary support is provided to the patient.
Another issue arises from omitting allergies and nutritional requirements. This information is vital for clinicians to prescribe appropriate treatments and avoid potential complications related to allergies and dietary restrictions.
Providing insufficient details in the section for orders and goals can also lead to confusion. Specificity is key here to ensure that care providers understand the treatments needed and the objectives for patient recovery.
Some people forget to include the date of the physician's signature. This date is essential in validating the plan of care, and lacking it means the document may not be considered officially complete.
Moreover, failing to retain a copy of the completed CMS 485 form is a mistake that can have consequences later on. Keeping a copy is crucial for tracking patient care and serving as a point of reference for future treatments.
Lastly, not thoroughly reviewing the form for errors before submission can lead to overlooked mistakes that affect payment and patient care continuity. Taking the time to carefully check all sections can prevent headaches down the road.
By steering clear of these common errors, individuals can help ensure that home health care services are delivered smoothly and effectively, benefiting both patients and providers.
Documents used along the form
The CMS 485 form, known as the Home Health Certification and Plan of Care, is a crucial document for patients receiving home health services. It outlines the medical and care requirements specific to each patient. Alongside this form, several other documents are often necessary for comprehensive care planning and billing. Below is a list of these important forms.
- CMS 486 (Home Health Agency/Provider Notification): This form serves as a notification to the Medicare Administrative Contractor (MAC) that home health services are initiated. It informs them of the patient's eligibility and care needs.
- CMS 1500 (Health Insurance Claim Form): This form is used by healthcare providers to bill Medicare and other payers for medical services provided. It captures information about the patient, the provider, and the services rendered.
- Plan of Care (POC): A detailed document outlining the specific treatment and services the patient will receive. It includes goals, interventions, and benchmarks to measure progress towards recovery.
- CMS 845 (Home Health Agency Certification and Receipt of Services): This form confirms the enrollment and receipt of services by the home health agency. It ensures that the agency complies with Medicare regulations.
- Patient Assessment/Outcome Measure (OASIS): A comprehensive assessment tool that evaluates a patient's condition and outcomes over time. This form is required for Medicare certification and recertification.
- Physician Orders (for Home Health services): A document where the physician specifies the care needed by the patient, including treatments and medications. It is essential for guiding home health providers in delivering appropriate care.
Each of these documents plays a vital role in ensuring that patients receive the necessary care and that providers maintain compliance with Medicare regulations. Proper completion and management of these forms facilitate efficient communication between patients, providers, and insurers, ultimately leading to better health outcomes.
Similar forms
- CMS 486 Form: This form is also related to home health services and outlines the plan of care initiated by a healthcare provider. It details the patient's needs and the agreed-upon treatments, similar to the CMS 485 which includes a certification for home health care.
- CMS 422A Form: Like the CMS 485, this document certifies Medicare eligibility for home health services. It establishes medical necessity based on the patient's condition, ensuring that the services provided align with Medicare's requirements.
- CMS 487 Form: This form focuses on the establishment of a home health plan of care following a patient’s assessment. It works in tandem with the CMS 485 by confirming the specifics of care, much like how the 485 certifies the need for that care.
- CMS 500 Form: Similar to the 485, this document is a request for home health services that highlights the patient's condition and required treatments. It emphasizes the necessity for intermittent skilled care, providing similar information for processing claims.
- Medicare Plan of Care Template: This is an informal document used by healthcare providers to outline treatment plans for patients. It shares the same purpose as the CMS 485 by delineating patient needs, treatment goals, and monitoring strategies that ensure continuity of care.
Dos and Don'ts
When filling out the CMS 485 form, it's crucial to ensure accuracy and completeness. Here are some tips to help you navigate the process smoothly:
- Do: Carefully read all instructions provided with the form to understand what information is required.
- Do: Double-check that you have entered the correct patient details, including their name, address, and date of birth.
- Do: Provide detailed information about medications, including dose and frequency, to ensure proper care planning.
- Do: Clearly note any functional limitations and permitted activities to aid in recovery.
- Don't: Rely on memory alone; always reference the patient’s medical records for accurate data.
- Don't: Leave any required fields blank; incomplete information may delay processing.
- Don't: Use medical jargon or vague language; clarity is essential in describing the patient's condition and needs.
- Don't: Forget to sign and date the form; missing signatures can result in further complications.
Misconceptions
Misconception 1: The CMS 485 form is only necessary for patients receiving home health care with Medicare.
This is not entirely accurate. While the CMS 485 form is commonly associated with Medicare, it is also utilized by other payers and healthcare systems to ensure proper documentation and care planning for patients receiving home health services.
Misconception 2: Completing the CMS 485 form guarantees approval for home health services.
Filling out the form correctly is essential, but it does not guarantee service approval. The form is part of the process, and insurance providers will review it along with other documentation before making their final decision.
Misconception 3: The form only has to be filled out once for ongoing care.
In reality, the CMS 485 form must be updated regularly, especially if there are changes in the patient's condition or the care plan. Regular updates ensure the plan reflects the current needs of the patient and meets the requirements of the payer.
Misconception 4: Only doctors can fill out the CMS 485 form.
This is another common misunderstanding. While a physician's signature is required, other qualified healthcare professionals can assist in completing sections of the form, as long as they provide relevant information about the patient's care.
Misconception 5: The CMS 485 form is purely administrative and does not impact patient care.
Actually, the information compiled in the CMS 485 form plays a critical role in shaping the patient's care plan. It helps ensure that all healthcare providers are on the same page regarding the services a patient requires, which directly influences the quality of care.
Misconception 6: The data on the CMS 485 form is kept confidential and is not shared with third parties.
While there are privacy protections, some information may be shared with third parties responsible for reviewing or processing claims, such as peer review organizations or state licensing boards, under specific circumstances.
Key takeaways
Filling out and utilizing the CMS 485 form is crucial for home health agencies to ensure proper certification and care planning. Below are key takeaways regarding this important document.
- Patient Information: Gather accurate details such as the patient’s name, address, date of birth, and Medicare claim number to ensure the form is completed correctly.
- Medical Necessity: The form must clearly outline the patient's needs for skilled nursing care, therapy services, and the rationale for home-bound status to justify Medicare coverage.
- ICD Codes: Include appropriate ICD codes for principal, surgical, and other pertinent diagnoses. These codes are essential for proper billing and documentation of the patient's medical condition.
- Functional Limitations: Clearly define any functional limitations and activities permitted for the patient. This helps establish a tailored care plan that meets individual needs.
- Orders for Treatments: Specify detailed orders for all disciplines, including amount, frequency, and duration of services to provide clarity and direction for healthcare providers.
- Signatures Required: Ensure that the physician’s signature is obtained to validate the plan of care. The signature indicates ongoing responsibility for the patient's care.
- Legal Implications: Be aware that misrepresentation or concealment of information on this form can lead to severe penalties, including fines or imprisonment.
Careful attention to these aspects can enhance compliance and ensure that patients receive the necessary services while protecting the involved parties from potential legal issues.
Browse Other Templates
Ca Llc Formation,700 - Ensuring clarity in all obligations defines the operational capacities of both parties post-settlement.
Cash Vault Services - The signature ensures that you authorize the requested changes.
Trupanion Claim Form Canada - Provide the name of the hospital where your pet received treatment.