Fill Out Your Cms 849 Form
The CMS-849 form, also known as the Certificate of Medical Necessity for Seat Lift Mechanisms, plays a crucial role in the Medicare system for individuals requiring specific assistive devices. This form is used to certify that a seat lift mechanism is medically necessary for a patient, particularly those with mobility challenges due to conditions such as severe arthritis or neuromuscular diseases. The form is divided into several sections, where detailed patient information, including diagnosis codes and medical history, is collected. It requires the input of both the supplier and the treating physician, establishing a collaborative effort to document the necessity of the equipment. Additionally, physicians must provide their attestation and signature, asserting the accuracy and completeness of the information submitted. The form also outlines the estimated length of need for the device, which can range from one month to a lifetime, ensuring that Medicare understands the ongoing requirements of the patient. Through this structured approach, the CMS-849 form not only assists in securing necessary medical equipment but also helps to uphold the standards of care for Medicare recipients.
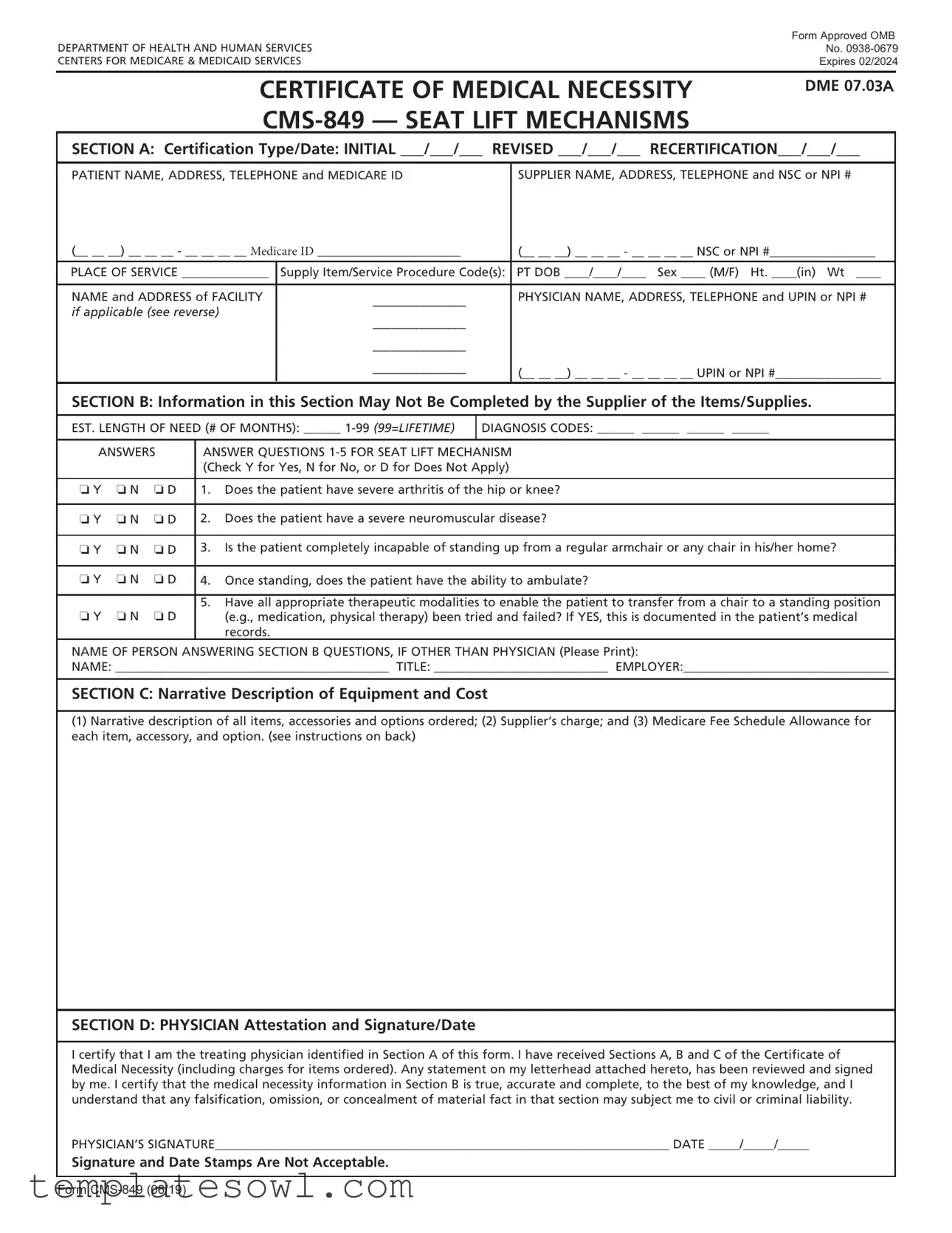
Cms 849 Example
|
Form Approved OMB |
|
DEPARTMENT OF HEALTH AND HUMAN SERVICES |
No. |
|
CENTERS FOR MEDICARE & MEDICAID SERVICES |
Expires 02/2024 |
|
|
|
|
CERTIFICATE OF MEDICAL NECESSITY
DME 07.03A
SECTION A: Certification Type/Date: INITIAL ___/___/___ REVISED ___/___/___ RECERTIFICATION___/___/___
PATIENT NAME, ADDRESS, TELEPHONE and MEDICARE ID |
SUPPLIER NAME, ADDRESS, TELEPHONE and NSC or NPI # |
(__ __ __) __ __ __ - __ __ __ __ Medicare ID _______________________ |
(__ __ __) __ __ __ - __ __ __ __ NSC or NPI #_________________ |
|
PLACE OF SERVICE ______________ |
Supply Item/Service Procedure Code(s): |
PT DOB ____/____/____ Sex ____ (M/F) Ht. ____(in) Wt ____ |
|
|
|
NAME and ADDRESS of FACILITY |
__________ |
PHYSICIAN NAME, ADDRESS, TELEPHONE and UPIN or NPI # |
if applicable (see reverse) |
__________ |
|
|
|
|
|
__________ |
|
|
__________ |
(__ __ __) __ __ __ - __ __ __ __ UPIN or NPI #_________________ |
|
|
|
SECTION B: Information in this Section May Not Be Completed by the Supplier of the Items/Supplies.
EST. LENGTH OF NEED (# OF MONTHS): ______
DIAGNOSIS CODES: ______ ______ ______ ______
ANSWERS |
ANSWER QUESTIONS |
|||
|
|
|
(Check Y for Yes, N for No, or D for Does Not Apply) |
|
|
|
|
|
|
o Y |
o N |
o D |
1. |
Does the patient have severe arthritis of the hip or knee? |
|
|
|
|
|
o Y |
o N |
o D |
2. |
Does the patient have a severe neuromuscular disease? |
|
|
|
|
|
o Y |
o N |
o D |
3. |
Is the patient completely incapable of standing up from a regular armchair or any chair in his/her home? |
|
|
|
|
|
o Y |
o N |
o D |
4. |
Once standing, does the patient have the ability to ambulate? |
5.Have all appropriate therapeutic modalities to enable the patient to transfer from a chair to a standing position
o Y o N o D |
(e.g., medication, physical therapy) been tried and failed? If YES, this is documented in the patient’s medical |
|
records. |
NAME OF PERSON ANSWERING SECTION B QUESTIONS, IF OTHER THAN PHYSICIAN (Please Print):
NAME: ____________________________________________ TITLE: ____________________________ EMPLOYER:_________________________________
SECTION C: Narrative Description of Equipment and Cost
(1)Narrative description of all items, accessories and options ordered; (2) Supplier’s charge; and (3) Medicare Fee Schedule Allowance for each item, accessory, and option. (see instructions on back)
SECTION D: PHYSICIAN Attestation and Signature/Date
I certify that I am the treating physician identified in Section A of this form. I have received Sections A, B and C of the Certificate of Medical Necessity (including charges for items ordered). Any statement on my letterhead attached hereto, has been reviewed and signed by me. I certify that the medical necessity information in Section B is true, accurate and complete, to the best of my knowledge, and I understand that any falsification, omission, or concealment of material fact in that section may subject me to civil or criminal liability.
PHYSICIAN’S SIGNATURE_________________________________________________________________________ DATE _____/_____/_____
Signature and Date Stamps Are Not Acceptable.
Form

INSTRUCTIONS FOR COMPLETING THE CERTIFICATE OF MEDICAL NECESSITY
FOR SEAT LIFT MECHANISMS
SECTION A: |
(May be completed by the supplier) |
CERTIFICATION |
If this is an initial certification for this patient, indicate this by placing date (MM/DD/YY) needed initially in the space TYPE/ |
DATE: |
marked “INITIAL.” If this is a revised certification (to be completed when the physician changes the order, based on the |
|
patient’s changing clinical needs), indicate the initial date needed in the space marked “INITIAL,” and indicate the |
|
recertification date in the space marked “REVISED.” If this is a recertification, indicate the initial date needed in the |
|
space marked “INITIAL,” and indicate the recertification date in the space marked “RECERTIFICATION.” Whether |
|
submitting a REVISED or a RECERTIFIED CMN, be sure to always furnish the INITIAL date as well as the REVISED or |
|
RECERTIFICATION date. |
PATIENT |
Indicate the patient’s name, permanent legal address, telephone number and his/her Medicare ID as it appears on his/her |
INFORMATION: |
Medicare card and on the claim form. |
SUPPLIER |
Indicate the name of your company (supplier name), address and telephone number along with the Medicare Supplier |
INFORMATION: |
Number assigned to you by the National Supplier Clearinghouse (NSC) or applicable National Provider Identifier (NPI). If |
|
using the NPI Number, indicate this by using the qualifier XX followed by the |
|
e.g. NSC number, use the qualifier 1C followed by the |
PLACE OF SERVICE: |
Indicate the place in which the item is being used, i.e., patient’s home is 12, skilled nursing facility (SNF) is 31, End |
|
Stage Renal Disease (ESRD) facility is 65, etc. Refer to the DMERC supplier manual for a complete list. |
FACILITY NAME: |
If the place of service is a facility, indicate the name and complete address of the facility. |
SUPPLY ITEM/SERVICE |
List all procedure codes for items ordered. Procedure codes that do not require certification should not be listed |
PROCEDURE CODE(S): |
on the CMN. |
PATIENT DOB, HEIGHT, |
Indicate patient’s date of birth (MM/DD/YY) and sex (male or female); height in inches and weight in pounds, if requested. |
WEIGHT AND SEX: |
|
PHYSICIAN NAME, |
Indicate the PHYSICIAN’S name and complete mailing address. |
ADDRESS: |
|
PHYSICIAN |
Accurately indicate the treating physician’s Unique Physician Identification Number (UPIN) or applicable National |
INFORMATION: |
Provider Identifier (NPI). If using the NPI Number, indicate this by using the qualifier XX followed by the |
|
If using UPIN number, use the qualifier 1G followed by the |
PHYSICIAN’S |
Indicate the telephone number where the physician can be contacted (preferably where records would be accessible |
TELEPHONE NO: |
pertaining to this patient) if more information is needed. |
SECTION B: |
(May not be completed by the supplier. While this section may be completed by a |
|
Physician employee, it must be reviewed, and the CMN signed (in Section D) by the treating practitioner.) |
EST. LENGTH OF NEED: |
Indicate the estimated length of need (the length of time the physician expects the patient to require use of the ordered |
|
item) by filling in the appropriate number of months. If the patient will require the item for the duration of his/her life, |
|
then enter “99”. |
DIAGNOSIS CODES: |
In the first space, list the diagnosis code that represents the primary reason for ordering this item. List any additional |
|
diagnosis codes that would further describe the medical need for the item (up to 4 codes). |
QUESTION SECTION: |
This section is used to gather clinical information to help Medicare determine the medical necessity for the item(s) |
|
being ordered. Answer each question which applies to the items ordered, checking “Y” for yes, “N” for no, or “D” for |
|
does not apply. |
NAME OF PERSON |
If a clinical professional other than the treating physician (e.g., home health nurse, physical therapist, dietician) or a |
ANSWERING SECTION B |
physician employee answers the questions of Section B, he/she must print his/her name, give his/her professional title |
QUESTIONS: |
and the name of his/her employer where indicated. If the physician is answering the questions, this space may be |
|
left blank. |
SECTION C: |
(To be completed by the supplier) |
NARRATIVE |
Supplier gives (1) a narrative description of the item(s) ordered, as well as all options, accessories, supplies and drugs; |
DESCRIPTION OF |
(2) the supplier’s charge for each item(s), options, accessories, supplies and drugs; and (3) the Medicare fee schedule |
EQUIPMENT & COST: |
allowance for each item(s), options, accessories, supplies and drugs, if applicable. |
SECTION D: |
(To be completed by the physician) |
PHYSICIAN |
The physician’s signature certifies (1) the CMN which he/she is reviewing includes Sections A, B, C and D; (2) the |
ATTESTATION: |
answers in Section B are correct; and (3) the |
PHYSICIAN SIGNATURE |
After completion and/or review by the physician of Sections A, B and C, the physician’s must sign and date the CMN in |
AND DATE: |
Section D, verifying the Attestation appearing in this Section. The physician’s signature also certifies the items ordered |
|
are medically necessary for this patient. |
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is
DO NOT SUBMIT CLAIMS TO THIS ADDRESS. Please see http://www.medicare.gov/ for information on claim filing.
Form
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Purpose | The CMS-849 form is used to certify the medical necessity of seat lift mechanisms for Medicare beneficiaries. |
| Governing Authority | This form is governed under the regulations set forth by the Centers for Medicare & Medicaid Services (CMS). |
| Expiration Date | The current approval for the CMS-849 form expires in February 2024. |
| Sections Overview | The form includes several sections: A for certification details, B for medical necessity questions, C for item description, and D for physician's attestation. |
| Estimation of Need | Users must indicate the estimated length of need, which can range from 1 to 99 months, with 99 representing lifetime need. |
| Signature Requirement | The form must be signed and dated by the treating physician, confirming the accuracy of the information provided. |
Guidelines on Utilizing Cms 849
Filling out the CMS 849 form involves several detailed steps to ensure all necessary information is accurately provided. It’s essential to have all relevant patient and medical information on hand to facilitate the completion of this form.
- Start by identifying the certification type in Section A. Choose whether it is an INITIAL, REVISED, or RECERTIFICATION certification and fill in the appropriate date.
- Enter the patient’s details. Fill in their name, address, telephone number, and Medicare ID.
- Provide your details as the supplier. This includes the supplier name, address, telephone number, and either the NSC or NPI number.
- Specify the place of service where the seat lift mechanism will be used. Use the appropriate code to indicate this location.
- List any supply items or service procedure codes associated with the equipment.
- Record the patient’s date of birth, height (in inches), weight, and sex (M/F).
- Fill in the physician's information. Write down their name, address, telephone number, and UPIN or NPI number.
- In Section B, provide information regarding the estimated length of need for the item, filling in the number of months required (1-99). Indicate the diagnosis codes relevant to the medical need.
- Answer the questions regarding the patient’s condition in Section B. Use “Y” for yes, “N” for no, or “D” for does not apply for each question about the patient’s health.
- If someone other than the physician answers the questions in Section B, they must print their name, title, and employer’s information.
- In Section C, the supplier must provide a narrative description of the equipment, detailing all items, accessories, and their costs, along with the Medicare Fee Schedule Allowance.
- Finally, in Section D, the physician should review and then sign and date the form, certifying the accuracy of the information provided in Sections A, B, and C.
After completing the CMS 849 form, ensure that it is submitted to the appropriate Medicare office. This document is crucial for verifying the medical necessity of the equipment being requested. Make sure all signatures and information are correct to avoid any delays or issues with processing.
What You Should Know About This Form
What is the CMS 849 form?
The CMS 849 form, also known as the Certificate of Medical Necessity for Seat Lift Mechanisms, is a document used to certify that a patient requires a seat lift mechanism based on medical necessity. This form is essential for Medicare providers to obtain reimbursement for the device, ensuring that the patient's needs are properly addressed.
Who needs to fill out the CMS 849 form?
The CMS 849 form requires input from multiple parties. Typically, the treating physician completes Section D to certify medical necessity. Sections A and C can be filled out by the supplier, while Section B may be answered by non-physician clinicians or a physician’s employee, but it must be signed by the physician.
What information is required in Section A?
In Section A, you will need to provide the patient’s name, contact information, Medicare ID, and details about the supplier including name and NSC or NPI number. It also asks for certification type—initial, revised, or recertification—and the date. Accurate information is crucial for processing.
What is Section B about?
Section B gathers clinical information to establish the medical necessity of a seat lift mechanism. It contains specific questions that must be answered to support the claims. Anyone completing this section must ensure their answers are accurate, as they will form the basis of the medical necessity determination.
How do I determine the estimated length of need?
The estimated length of need should reflect the period the physician expects the patient will require the seat lift mechanism. You can indicate a specific number of months or use '99' for a lifetime need. This is critical for the approval process and affects reimbursement eligibility.
What happens if the form is filled out incorrectly?
Filling out the CMS 849 form incorrectly can lead to delays in processing, denials of claims, or audits. It is vital to double-check all details, including patient information, diagnosis codes, and responses in Section B. Keeping accurate records will significantly help in these situations.
What kind of equipment details are needed in Section C?
In Section C, it is essential to provide a clear narrative description of the seat lift mechanism and any accessories. You must also include the supplier’s charge and the Medicare Fee Schedule allowance for each item. Transparency and detail in this section ensure that everything can be reviewed accurately.
What is the physician's role in completing this form?
The physician plays a crucial role by verifying the accuracy and completeness of all information on the CMS 849 form. They must review Sections A, B, and C before signing in Section D, attesting that the items ordered are medically necessary for the patient. Without the physician's signature, the form will not be valid.
How can I submit the CMS 849 form?
Once completed, you should submit the CMS 849 form to Medicare as part of your claims process. It is important not to send the form to the address listed for comments or improvements. Ensure you follow the guidelines for submission according to Medicare's instructions to avoid any issues.
When does the CMS 849 form expire?
The CMS 849 form is currently set to expire in February 2024. It’s crucial to stay updated on any changes or new versions of the form to ensure compliance and facilitate timely reimbursement for the necessary equipment. Regular checks on CMS guidelines are recommended.
Common mistakes
Filling out the CMS 849 form can be straightforward, but mistakes are common and can delay necessary medical equipment for patients. One frequent mistake is failing to indicate the correct certification type. Many people either overlook marking whether the request is for an initial certification, revision, or recertification or do not provide the required dates in the appropriate sections. This confusion can lead to unnecessary back-and-forth with Medicare.
Another common error involves patient information. It is vital to provide the full and accurate Medicare ID, permanent address, and phone number. When this information is incorrect or incomplete, claims may be denied. Always double-check the Medicare card for the correct ID and ensure it matches the form.
In the section dedicated to answers regarding the patient's condition, individuals often misunderstand the answer format. They might answer questions incorrectly by choosing "Y," "N," or "D" without ensuring that they've understood the questions properly. Each question directly impacts the determination of medical necessity. Thus, if the answers are unclear, this may hinder the approval process.
People frequently neglect to assign diagnosis codes. Listing appropriate codes is critical, as these codes communicate to Medicare why the lift mechanism is medically necessary. Many fail to include all four possible codes or choose codes that don't accurately reflect the patient's condition, which can lead to denial of the request.
A common blunder happens in the narrative description section. Some submitters provide vague or insufficient descriptions of the items requested. This section needs clarity and detail about the seat lift mechanism, accessories, and costs associated with each component. Lack of specificity can slow down the review process.
Finally, the physician's signature and date must not only be present but also properly formatted. Using a signature stamp or failing to date the signature can lead to automatic rejection of the form. The physician must certify that they have reviewed all sections and confirm the information provided is correct. Ensuring these details are complete is essential for finalizing the claim.
Documents used along the form
The CMS-849 form, also known as the Certificate of Medical Necessity for Seat Lift Mechanisms, is an important document in the Medicare system. This form helps to establish the medical need for a seat lift mechanism for a patient, and it is often accompanied by several other documents that provide additional information or support for the claim. Below are related forms and documents commonly associated with the CMS-849.
- CMN Guidelines: This document outlines the specific requirements and instructions for completing the CMS-849 form, including the necessary information healthcare providers must include to demonstrate medical necessity.
- Medicare Supplier Agreement: This contract grants the supplier the authority to provide durable medical equipment (DME) to Medicare beneficiaries and outlines the terms of service and reimbursement procedures.
- Physician's Order: An additional document signed by the treating physician, stating their order for the seat lift mechanism. It often includes specific details about the patient's diagnosis and need for the equipment.
- Patient Medical Record: This record contains comprehensive medical history and treatment notes, providing evidence of the patient's condition and the necessity for the lift mechanism.
- Diagnosis Codes Documentation: A detailed list of diagnosis codes related to the patient's medical condition. This supports the medical necessity claimed in the CMS-849.
- Medical Necessity Statement: This statement elaborates on the clinical justification for the seat lift mechanism, often prepared by healthcare providers to reinforce the need for the equipment.
- Insurance Claim Form: This form is used to submit a request for payment for the seat lift mechanism through Medicare, which will reference the information provided in the CMS-849.
- Durable Medical Equipment (DME) Receipt: The receipt from the DME supplier indicates the purchase of the seat lift mechanism, often required for claims processing and reimbursement.
- Letter of Medical Necessity: A customizable letter from the physician or healthcare provider that specifies why the seat lift mechanism is essential for the patient’s care and well-being.
These documents collectively support the CMS-849 form in establishing a patient's eligibility for Medicare reimbursement for a seat lift mechanism. Ensuring each document is accurately completed and submitted can facilitate a smoother claims process and improve the chances of reimbursement approval.
Similar forms
- CMS-486 - This form is used to certify medical necessity for durable medical equipment (DME) prescribed by a physician. Like the CMS-849, it requires detailed patient information and a physician's signature to affirm the necessity of the device.
- CMS-1500 - A standard claim form for healthcare professionals to bill Medicare and other insurers. It includes patient details, service codes, and requires a signature, paralleling the CMS-849's comprehensive patient and provider information requirements.
- CMS-381 - Used for the Certification of Medical Necessity for Orthotics and Prosthetics. Similar to the CMS-849, it verifies the medical need specifically for orthotic and prosthetic devices.
- DA Form 7880 - This Department of Defense form certifies medical necessity for certain items within military healthcare. It serves a similar purpose, confirming that a specific item is essential for the patient’s care.
- Form 3372 - Utilized by the Veterans Affairs for Durable Medical Equipment. This form assesses the need for medical equipment in the veteran population, akin to the evaluation done in the CMS-849.
- CMS-855 - This provider enrollment application form gathers extensive information about healthcare providers, much like the CMS-849 gathers details about suppliers and practitioners involved in patient care.
- Medicaid Provider Enrollment Application - Similar to the CMS-849, it collects information to affirm a provider’s services to be covered under Medicaid, ensuring the necessary medical documentation is provided.
- HCFA-460 - A form that documents clinical care and treatment, confirming aspects like medical necessity, similar to the way the CMS-849 collects and certifies patient information specifically for seat lift mechanisms.
Dos and Don'ts
When completing the CMS 849 form, it’s important to follow guidelines to ensure accuracy and avoid delays. Here are six things to keep in mind:
- Do: Fill in the patient’s information accurately, including name, address, phone number, and Medicare ID.
- Don't: Skip any required fields. Missing information can lead to rejection of the form.
- Do: Clearly label whether you are submitting an initial or revised certification.
- Don't: Provide false or exaggerated medical necessity information. This can have legal repercussions.
- Do: Ensure the treating physician signs Section D of the form, providing their attestation.
- Don't: Use signature stamps. The physician must sign personally for the form to be valid.
Misconceptions
Misconceptions about the CMS 849 form can lead to confusion and errors in its completion. The following list clarifies nine common misunderstandings regarding the form:
- This form is only for establishing initial medical necessity. Many believe that the CMS 849 form is exclusively for initial certifications. In reality, it is also applicable for revisions and recertifications to reflect changing patient needs.
- Anyone can complete all sections of the CMS 849 form. While suppliers can fill out Section A, Sections B and D must be completed by a physician or a qualified clinician under their supervision.
- The CMS 849 form can be submitted without a physician's signature. A physician's signature in Section D is mandatory, confirming the information and medical necessity for the ordered items.
- All equipment listed on the form is guaranteed coverage by Medicare. Listing an item does not ensure coverage. It must meet Medicare's criteria for medical necessity, as documented in the patient’s medical records.
- Only one diagnosis code is required for the form. The CMS 849 allows for multiple diagnosis codes to provide a complete picture of the patient's medical condition, up to four codes can be listed.
- The estimated length of need can be based on guesswork. The estimated length of need must be based on the physician’s clinical judgment and expectations for how long the patient will require the equipment.
- The questions in Section B are optional. Responses to the questions in Section B are essential for evaluating medical necessity. Each must be answered accurately to avoid process delays.
- The CMS 849 form does not require any documentation. Documentation must support the answers provided, especially if certain therapies or modalities have been attempted prior to the equipment's request.
- Completing this form is a straightforward task with no detailed guidelines. Proper completion of the CMS 849 requires attention to specific instructions and guidelines, which must be thoroughly understood to ensure accuracy.
Understanding these misconceptions can enhance the efficiency and accuracy of completing the CMS 849 form, ensuring that patients get the medical equipment they need in a timely manner.
Key takeaways
When filling out and using the CMS-849 form, a Certificate of Medical Necessity for seat lift mechanisms, there are important considerations to keep in mind. Here are five key takeaways:
- Correct Certification Type: Always indicate the appropriate certification type—initial, revised, or recertification—by providing specific dates in the designated spaces. This ensures clarity about the patient's ongoing medical needs.
- Accurate Patient Information: Include comprehensive patient details, such as the patient's full name, address, telephone number, and Medicare ID. These specifics are crucial for processing the claim effectively.
- Physician’s Role: The physician must not only complete Section D but also assure that Sections A, B, and C are accurate. This ensures the form reflects the true medical necessity and compliance with Medicare requirements.
- Complete Diagnosis Codes: Provide all relevant diagnosis codes in Section B. Indicate up to four codes that support why the equipment is necessary. This documentation is essential for Medicare to assess eligibility.
- Narrative Description: In Section C, the supplier should offer a detailed narrative description of the equipment along with its cost and associated Medicare fee schedule allowances. This complete information assists in determining the appropriate coverage.
Filling out the CMS-849 form accurately is vital for ensuring patients receive necessary equipment under Medicare coverage. Proper attention to each section can help avoid potential claim denials.
Browse Other Templates
Pennsylvania Llc Filing Requirements - This form represents a formal request to conduct business within Pennsylvania.
New York Sales Tax Rate - The form cannot be used for seeking legal advice or professional tax return preparation services.