Fill Out Your Cms 855B Form
The CMS 855B form is a critical component for clinics, group practices, and other suppliers seeking to enroll in the Medicare program. This application not only allows organizations to obtain a Medicare billing number but also enables them to update their enrollment information when necessary. A variety of scenarios call for the completion of this form, whether it involves new enrollment, changes due to a new tax identification number, or revalidation of existing information. Importantly, the CMS 855B must be filled out accurately and thoroughly to prevent delays in the enrollment process. Applicants are required to submit supporting documentation alongside the form, ensuring compliance with Medicare regulations. Additionally, the form uniquely identifies the structure and ownership of healthcare organizations, making it vital for maintaining a seamless billing process with Medicare. Throughout this process, obtaining a National Provider Identifier (NPI) is paramount, as it is a prerequisite for submitting the application. Navigating the complexities of Medicare enrollment is essential for those in the healthcare sector, and understanding the CMS 855B form serves as a crucial first step in this journey.
Cms 855B Example
MEDICARE ENROLLMENT APPLICATION
Clinics/Group Practices and Other Suppliers
SEE PAGE
SEE SECTION 12 FOR A LIST OF SUPPORTING DOCUMENTATION TO BE SUBMITTED WITH THIS APPLICATION.
TO VIEW YOUR CURRENT MEDICARE ENROLLMENT RECORD GO TO: HTTPS://PECOS.CMS.HHS.GOV

|
Form Approved |
DEPARTMENT OF HEALTH AND HUMAN SERVICES |
OMB No. |
CENTERS FOR MEDICARE & MEDICAID SERVICES |
Expires: 03/2024 |
|
|
WHO SHOULD SUBMIT THIS APPLICATION
Clinics, group practices, and other suppliers must complete this application to enroll in the Medicare program and receive a Medicare billing number.
Clinics, group practices, and other suppliers can apply for enrollment in the Medicare program or make a change in their enrollment information using either:
•The
•The paper
For additional information regarding the Medicare enrollment process, including
NOTE: Applicants using this application require a Type 2 NPI. See below for more information.
NOTE: For the purposes of this application, the word “supplier” is used universally and includes any providers or suppliers who are required to complete the
Complete and submit this application if you are an organization/group or other supplier that plans to bill Medicare and you are:
•Enrolling in the Medicare program for the first time with this Medicare Administrative Contractor (MAC) under this tax identification number.
•Currently enrolled in Medicare but have a new tax identification number. If you are reporting a change to your current Medicare enrollment to your tax identification number, you must complete a new application.
•Currently enrolled in Medicare and need to enroll in another Medicare Administrative Contractor’s (MAC’s) jurisdiction (e.g., you have opened a practice location in a geographic territory serviced by another MAC).
•Revalidating your Medicare enrollment. CMS may require you to submit or update your enrollment information. The MAC will notify you when it is time for you to revalidate your enrollment information. Do not submit a revalidation application until you have been contacted by your MAC.
•Previously enrolled in Medicare and you need to reactivate your Medicare billing number to resume billing. Prior to being reactivated, you must meet all current requirements for your supplier type before reactivation may occur.
•Currently enrolled in Medicare and need to make changes to your enrollment information (e.g., you have added or changed a practice location). Changes must be reported in accordance with the timeframes established in 42 C.F.R. section 424.516. (IDTF changes of information must be reported in accordance with 42 C.F.R. section 410.33.)
•A hospital, hospital department, or other medical practice or clinic that may bill for Medicare Part A services but will also bill for Medicare Part B practitioner services or provide purchased laboratory tests to other entities that will bill Medicare Part B.
•A certified Medicare Part B provider (i.e. Ambulatory Surgery Center, Portable
•A medical practice, group/clinic or other supplier that will bill for Medicare Part B services (e.g., group practices, clinics, independent laboratories, portable
•Terminating a Physician Assistant (PA) employer relationship.
•Terminating an employer or individual relationship with an Independent Diagnostic Testing Facility (IDTF).
•Voluntary terminating your Medicare billing privileges. A supplier should voluntarily terminate its Medicare enrollment when it:
•Will no longer be rendering services to Medicare patients, or
•Is planning to cease (or has ceased) operations.
NOTE: For the purposes of this section of this application, an entity is defined as a group/clinic, other supplier, or any organization to which you will reassign your Medicare benefits.
1 |
BILLING NUMBER AND NATIONAL PROVIDER IDENTIFIER INFORMATION
The Provider Transaction Access Number (PTAN), often referred to as a Medicare Supplier Number or Medicare Billing Number, is a generic term for any number other than the National Provider Identifier (NPI) that is used by a supplier bill the Medicare program.
The NPI is the standard unique health identifier for health care providers and suppliers and is assigned by the National Plan and Provider Enumeration System (NPPES). To enroll in Medicare, you must obtain an NPI and furnish it on this application prior to enrolling in Medicare or when submitting a change to your existing Medicare enrollment information. Applying for the NPI is a process separate from Medicare enrollment.
As a supplier, it is your responsibility to determine if you have “subparts.” A subpart is a component of an organization (supplier) that furnishes healthcare and is not itself a legal entity. If you do have subparts, you must determine if they should obtain their own unique NPIs. Before you complete this enrollment application, you need to make those determinations and obtain NPI(s) accordingly. To obtain an NPI, you may apply online at https://NPPES.cms.hhs.gov. For more information about NPI enumeration, visit
NOTE: The Legal Business Name (LBN) and Tax Identification Number (TIN) that you furnish in section 2A must be the same LBN and TIN you used to obtain your NPI. Once this information is entered into PECOS from this application, your LBN, TIN and NPI must match exactly in both PECOS and NPPES.
Organizational Health Care Providers (Entity Type 2): Organizational health care providers are eligible for an Entity Type 2 NPI (Organizations). Organizational health care providers may have a single employee or thousands of employees. Examples of organizational providers include hospitals, home health agencies, groups/clinics, nursing homes, ambulance companies, health care provider corporations formed by groups/ individuals, and single member LLCs with an EIN, not individual health care providers.
Important: For NPI purposes, sole proprietors and sole proprietorships are considered to be “Type 1” providers. Organizations (e.g., corporations, partnerships) are treated as “Type 2” entities. When reporting the NPI of a sole proprietor on this application, therefore, the individual’s Type 1 NPI should be reported; for organizations, the Type 2 NPI should be furnished.
To obtain an NPI, you may apply online at https://NPPES.cms.hhs.gov.
INSTRUCTIONS FOR COMPLETING AND SUBMITTING THIS APPLICATION
All information on this form is required with the exception of those fields specifically marked as “optional.” Any field marked as optional is not required to be completed nor does it need to be updated or reported as a “change of information” as required in 42 C.F.R. section 424.516. However, it is highly recommended that if reported, these fields be kept
•This form must be typed. It may not be handwritten. If portions of this form are handwritten, the application may be returned to you by your MAC.
•When necessary to report additional information, copy and complete the applicable section as needed.
•Attach all required supporting documentation.
•Keep a copy of your completed Medicare enrollment package for your own records.
2 |
TIPS TO AVOID DELAYS IN YOUR ENROLLMENT
To avoid delays in the enrollment process, you should:
•Complete all required sections, as shown in section 1.
•Ensure that the legal business name shown in section 2 matches the name on the tax documents.
•Ensure that the correspondence address shown in section 2 is the supplier’s address.
•Enter your NPI(s) in the applicable section(s).
•Include the Electronic Funds Transfer (EFT) Authorization Agreement (when applicable) with your enrollment application with a voided check or bank letter.
•Sign and date section 15.
•Ensure all supporting documents are sent to your designated MAC.
•The supplier pays the required application fee (via https://pecos.cms.hhs.gov/pecos/feePaymentWelcome.do) upon initial enrollment, the addition of a new business location, revalidation and, if requested, reactivation PRIOR to completing and submitting this application to the MAC.
ADDITIONAL INFORMATION
•You may visit our website to learn more about the enrollment process via the
•The MAC may request additional documentation to support and validate information reported on this application. You are responsible for providing this documentation within 30 days of the request per 42 C.F.R. section 424.525(a)(1).
•The information you provide on this form is protected under 5 U.S.C. section 552(b)(4) and/or (b)(6), respectively. For more information, see the last page of this application to read the Privacy Act Statement.
ACRONYMS COMMONLY USED IN THIS APPLICATION
C.F.R.: Code of Federal Regulations
EFT: Electronic Funds Transfer
EIN: Employer Identification Number
IHS: Indian Health Service
IRS: Internal Revenue Service
LBN: Legal Business Name
LLC: Limited Liability Corporation
MAC: Medicare Administrative Contractor
NPI: National Provider Identifier
NPPES: National Plan and Provider Enumeration System
OTP: Opioid Treatment Program
PTAN: Provider Transaction Access Number also referred to as the Medicare Identification Number
SSN: Social Security Number
TIN: Tax Identification Number
DEFINITIONS
NOTE: For the purposes of this
•Add: You are adding additional enrollment information to your existing information (e.g. practice locations).
•Change: You are replacing existing information with new information (e.g. billing agency, managing employee) or updating existing information (e.g. change in suite #, telephone #).
•Remove: You are removing existing enrollment information.
WHERE TO MAIL YOUR APPLICATION
Send this completed application with original signatures and all required documentation to your designated MAC. The MAC that services your State is responsible for processing your enrollment application. To locate the mailing address for your designated MAC, go to www.cms.gov/MedicareProviderSupEnroll.
3 |
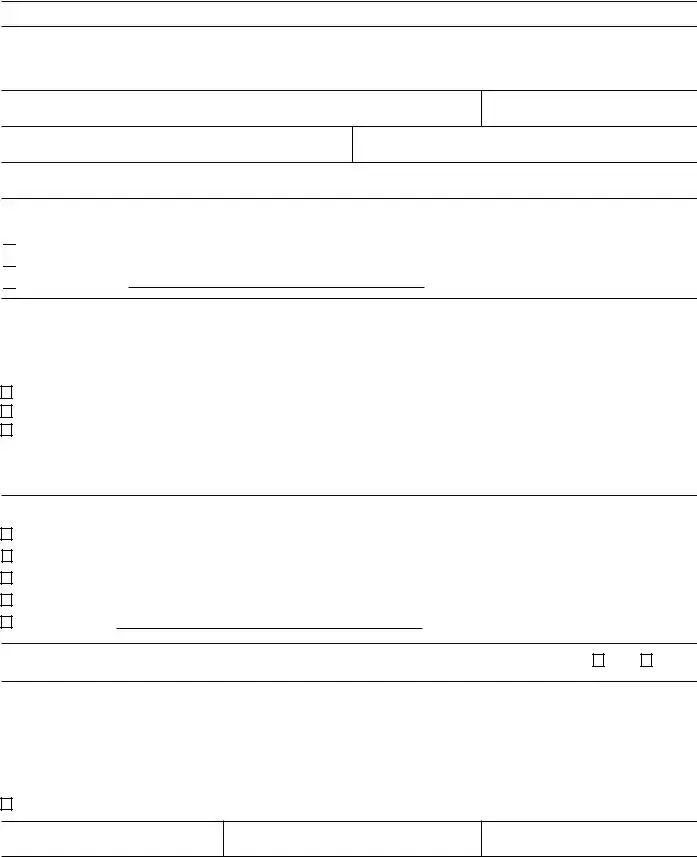
SECTION 1: BASIC INFORMATION
ALL APPLICANTS MUST COMPLETE THIS SECTION
A. REASON FOR SUBMITTING THIS APPLICATION
Check one box and complete the required sections of this application as indicated.
|
You are a new enrollee in Medicare |
Complete all applicable sections |
|
|
|
|
Ambulance suppliers must complete |
|
|
|
Attachment 1 |
|
|
|
IDTF suppliers must complete Attachment 2 |
|
|
|
OTPs must complete Attachment 3 |
|
|
|
|
|
You are enrolling with another Medicare Administrative |
Complete all applicable sections |
|
|
Contractor (MAC) |
Ambulance suppliers must complete |
|
|
|
|
|
|
|
|
Attachment 1 |
|
|
|
IDTF suppliers must complete Attachment 2 |
|
|
|
OTPs must complete Attachment 3 |
|
|
|
|
|
You are revalidating your Medicare enrollment |
Complete all applicable sections |
|
|
|
|
Ambulance suppliers must complete |
|
|
|
Attachment 1 |
|
|
|
IDTF suppliers must complete Attachment 2 |
|
|
|
OTPs must complete Attachment 3 |
|
|
|
|
|
You are reactivating your Medicare enrollment |
Complete all applicable sections |
|
|
|
|
Ambulance suppliers must complete |
|
|
|
Attachment 1 |
|
|
|
IDTF suppliers must complete Attachment 2 |
|
|
|
OTPs must complete Attachment 3 |
|
|
|
|
|
You are reporting a change to your Medicare enrollment |
Go to section 1B below |
|
|
information |
|
|
|
|
|
|
|
You are voluntarily terminating your Medicare enrollment |
Section 1, 2A1, 13 (optional), and 15 |
|
|
Effective date of termination (mm/dd/yyyy): |
Employers terminating Physician Assistants |
|
|
|
|
must complete sections 1, 2A1, 2F, 13 |
|
|
|
(optional), and 15 |
|
Medicare Identification Number: |
||
|
|
||
|
|
|
|
|
|
|
|
4 |
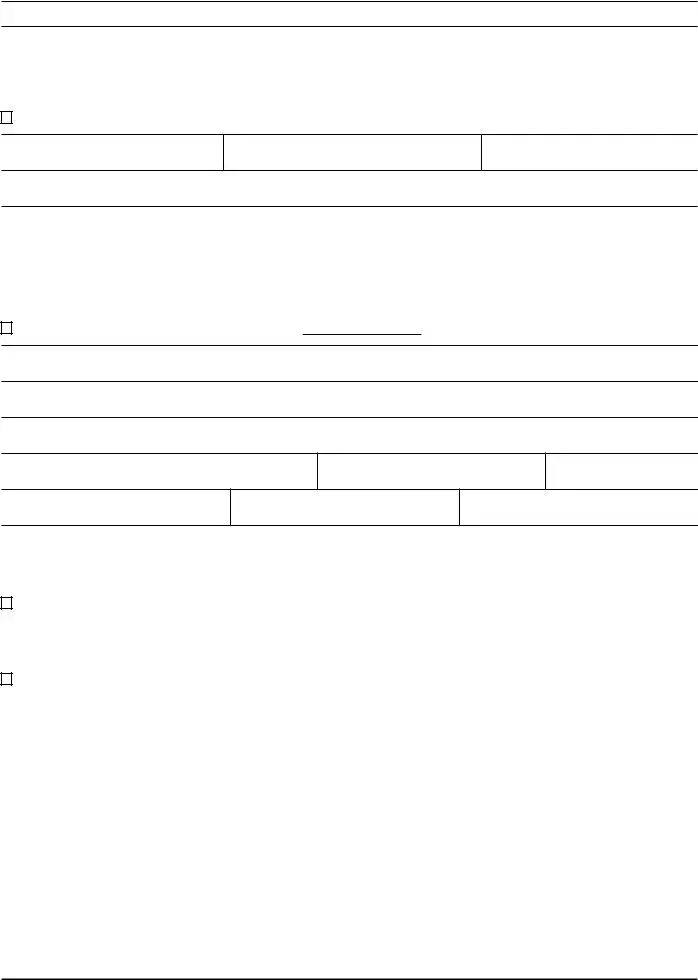
SECTION 1: BASIC INFORMATION (Continued)
B. WHAT INFORMATION IS CHANGING?
Check all that apply and complete the required sections.
Please note: When reporting ANY information, sections 1, 2A1, 3, and 15 MUST always be completed in addition to the information that is changing within the required section.
Changing Information |
Required Sections |
|
|
Business Identifying Information |
1, 2A1, 3, 12, 13 (optional) and 15 and 6 for |
|
the signer if that authorized or delegated |
|
official has not been established for this |
|
supplier |
|
|
Final Adverse Legal Actions |
1, 2A1, 3, 12, 13 (optional) and 15 and 6 for |
|
the signer if that authorized or delegated |
|
official has not been established for this |
|
supplier |
|
|
Medical Specialty Information |
1, 2A, 2B, 3, 4, 12, 13 (optional), and 15 and 6 |
|
for the signer if that authorized or delegated |
|
official has not been established for this |
|
supplier |
|
|
Supplier Specific Information |
1, 2A1, |
|
12,13 (optional), and 15 and 6 for the signer if |
|
that authorized or delegated official has not |
|
been established for this supplier |
|
|
Physician Assistant Employment Terminations |
1, 2A1, 2F, 3, 13 (optional) and 15 and 6 for |
|
the signer if that authorized or delegated |
|
official has not been established for this |
|
supplier |
|
|
Private Practice Business Information |
1, 2A, 3, 4A, 12, 13 (optional) and 15 and 6 |
|
for the signer if that authorized or delegated |
|
official has not been established for this |
|
supplier |
|
|
Change of Ownership (Hospitals, Hospital Departments, |
Complete all sections and provide a copy of |
Portable |
the sales agreement |
Only) |
|
|
|
Ownership Interest and/or Managing Control Information |
1, 2A1, 3, 5, 13, and 15, and 6 for the signer if |
(Organizations) |
that authorized or delegated official has not |
|
been established for this supplier |
|
|
Ownership Interest and/or Managing Control Information |
1, 2A1, 3, 6, 13, and 15, and another 6 for the |
(Individuals) |
signer if that authorized or delegated official |
|
has not been established for this supplier |
|
|
Managing Employee Information |
1, 2A1, 3, 6, 12, 13 (optional), and 15 and 6 |
|
for the signer if that authorized or delegated |
|
official has not been established for this |
|
supplier |
|
|
5 |
SECTION 1: BASIC INFORMATION (Continued)
Changing Information |
Required Sections |
|
|
|
|
Address Information |
1, 2A, 3, 12, 13 (optional) and 15 AND sections |
|
Correspondence Mailing Address |
2A3, 2A4, 4A, 4B, 4C, and/or 4E as applicable |
|
for the address that is being changed and 6 |
||
Medicare Beneficiary Medical Records Storage Address |
||
for the signer if that authorized or delegated |
||
Practice Location Address |
||
official has not been established for this |
||
|
||
Remittance Notices/Special Payment Mailing Address |
supplier |
|
Base of Operations Address for Mobile or Portable |
|
|
Suppliers (location of Business Office or Dispatcher/ |
|
|
Scheduler) |
|
|
|
|
|
Billing Agency Information |
1, 2A1, 3, 8, 13 (optional) and 15 and 6 for the |
|
|
signer if that authorized or delegated official |
|
|
has not been established for this supplier |
|
|
|
|
Authorized Official(s) and/or Delegated Official(s) |
1, 2A1, 3, 13, 15A1 (if you are an Authorized |
|
|
Official) or 15B1 (if you are a delegated |
|
|
official), and another 6 for the signer if that |
|
|
authorized or delegated official has not been |
|
|
established for this supplier |
|
|
|
|
Any other information not specified above |
1, 2A1, 3, 12 (if applicable), 13 (optional) and |
|
|
15 and the applicable section or |
|
|
that is changing and 6 for the signer if that |
|
|
authorized or delegated official has not been |
|
|
established for this supplier |
|
|
|
|
ATTACHMENT 1: AMBULANCE SERVICE SUPPLIERS (ONLY) |
|
|
|
|
|
Changing Information |
Required Sections |
|
|
|
|
Ambulance Supplier Transport Type |
1, 2A, 3, 12, 13 (optional) and 15 and 6 for the |
|
|
signer if that authorized or delegated official |
|
|
has not been established for this supplier |
|
|
Attachment 1(A) |
|
|
|
|
Geographic Area |
1, 2A, 3, 12, 13 (optional) and 15 and 6 for the |
|
|
signer if that authorized or delegated official |
|
|
has not been established for this supplier |
|
|
Attachment 1(B) |
|
|
|
|
State License Information |
1, 2A, 3, 12, 13 (optional) and 15 and 6 for the |
|
|
signer if that authorized or delegated official |
|
|
has not been established for this supplier |
|
|
Attachment 1(C) |
|
|
|
|
Vehicle Information |
1, 2A, 3, 12, 13 (optional) and 15 and 6 for the |
|
|
signer if that authorized or delegated official |
|
|
has not been established for this supplier |
|
|
Attachment 1(D) |
|
|
|
6 |
SECTION 1: BASIC INFORMATION (Continued)
ATTACHMENT 2: INDEPENDENT DIAGNOSTIC TESTING FACILITIES (ONLY)
Changing Information |
Required Sections |
|
|
1, 2A, 3, 12, 13 (optional) and 15 and 6 for the |
|
|
signer if that authorized or delegated official |
|
has not been established for this supplier |
|
Attachment 2(B) |
|
|
Interpreting Physician Information |
1, 2A, 3, 12, 13 (optional) and 15 and 6 for the |
|
signer if that authorized or delegated official |
|
has not been established for this supplier |
|
Attachment 2(C) |
|
|
Personnel (Technicians) Who Perform Tests |
1, 2A, 3, 12, 13 (optional) and 15 and 6 for the |
|
signer if that authorized or delegated official |
|
has not been established for this supplier |
|
Attachment 2(D) |
|
|
Supervising Physicians |
1, 2A, 3, 12, 13 (optional) and 15 and 6 for the |
|
signer if that authorized or delegated official |
|
has not been established for this supplier |
|
Attachment 2(E) |
|
|
ATTACHMENT 3: OPIOID TREATMENT PROGRAMS (ONLY) |
|
|
|
Changing Information |
Required Sections |
|
|
Opioid Treatment Program Personnel – Ordering Personnel |
1, 2A1, 3, 12, 13 (optional) and 15 and 6 for |
Identification |
the signer if that authorized or delegated |
|
official has not been established for this |
|
supplier |
|
Attachment 3A |
|
|
Opioid Treatment Program Personnel – Dispensing |
1, 2A1, 3, 12, 13 (optional) and 15 and 6 for |
Personnel Identification |
the signer if that authorized or delegated |
|
official has not been established for this |
|
supplier |
|
Attachment 3B |
|
|
7 |
SECTION 2: IDENTIFYING INFORMATION
A. SUPPLIER IDENTIFICATION INFORMATION
1. BUSINESS INFORMATION
Legal Business Name as Reported to the Internal Revenue Service
Tax Identification Number (TIN)
Medicare Identification Number (PTAN) (if issued)
National Provider Identifier (NPI)
Other Name (if applicable)
Type of Other Name (if applicable). Check box indicating Type of Other Name:

 Former Legal Business Name
Former Legal Business Name

 Doing Business As Name
Doing Business As Name

 Other (Describe):
Other (Describe):
Business Structure information
Identify how your business is registered with the IRS. (NOTE: If your business is a Federal and/or State government supplier, indicate
Proprietary
Disregarded Entity (Submit IRS Form 8832)
NOTE: If a checkbox identifying how the business is registered with the IRS is not completed, the supplier will be defaulted to “Proprietary.”
Identify the type of organizational structure of this supplier: (Check one)
Corporation
Limited Liability Company
Partnership
Sole Proprietor
Other (Specify):
Is this supplier an Indian Health Service (IHS) Facility? .....................................................................
Yes
No
2. LICENSE/CERTIFICATION/REGISTRATION INFORMATION
Complete the appropriate subsection(s) below for your supplier type as you will report in section 2B. If no subsection is associated with your supplier type, check the box stating the information is not applicable.
a. Active License Information
License Not Applicable
License Number
Effective Date (mm/dd/yyyy)
State Where Issued
8 |
SECTION 2: IDENTIFYING INFORMATION (Continued)
b. Active Certification Information
Complete the appropriate subsection(s) below for your supplier type as you will report in section 2B. If no subsection is associated with your supplier type, check the box stating the information is not applicable. *If
you are certified by a national entity, put the word “all” in the “State Where Issued” data field.
Certification Not Applicable
Certification Number
Effective Date (mm/dd/yyyy)
State Where Issued*
Certifying Entity (Specialty Board, State, Other)
3. CORRESPONDENCE MAILING ADDRESS
This is the address where correspondence will be sent to the supplier listed in section 2A1 by your designated MAC. This address cannot be a billing agent or agency’s address or a medical management company address.
If you are reporting a change to your Correspondence Mailing Address, check the box below. This will replace any current Correspondence Mailing Address on file.
Change |
Effective Date (mm/dd/yyyy): |
Attention (optional)
Correspondence Mailing Address Line 1 (P.O. Box or Street Name and Number)
Correspondence Mailing Address Line 2 (Suite, Room, Apt. #, etc.)
City/Town
State
ZIP Code + 4
Telephone Number (if applicable)
Fax Number (if applicable)
4. MEDICAL RECORD CORRESPONDENCE ADDRESS
This is the address where the medical record correspondence will be sent to the supplier listed in section 2A1 by your designated MAC. This information would be used for any medical record review requests.
Check here if your Medical Record Correspondence Address should be mailed to your Correspondence Address in section 2A3 (above) and skip this section.
If you are reporting a change to your Medical Record Correspondence Address, check the box below. This will replace any current Medical Record Correspondence Address on file.
Change |
Effective Date (mm/dd/yyyy): |
|
|
|
||||
|
|
|
|
|
|
|
|
|
Attention (optional) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Medical Record Correspondence Mailing Address Line 1 |
(P.O. Box or Street Name and Number) |
|||||||
|
|
|
|
|
|
|
||
Medical Record Correspondence Mailing Address Line 2 |
(Suite, Room, Apt. #, etc.) |
|
|
|
||||
|
|
|
|
|
|
|
|
|
City/Town |
|
|
|
|
State |
|
|
ZIP Code + 4 |
|
|
|
|
|
|
|||
Telephone Number (if applicable) |
Fax Number (if applicable) |
|
||||||
|
|
|
|
|
|
|
|
|
9 |
Form Characteristics
| Fact Name | Fact Description |
|---|---|
| Purpose | The CMS-855B form is used for clinics, group practices, and other suppliers to enroll in the Medicare program and obtain a Medicare billing number. |
| Eligibility | Only clinics, group practices, and certain suppliers can submit this form to enroll or make changes to their Medicare enrollment information. |
| Submission Methods | The form can be submitted online via the PECOS system or through traditional mail as a paper application. |
| Type 2 NPI Requirement | Applicants must have a Type 2 National Provider Identifier (NPI) before completing the CMS-855B form. |
| Supporting Documentation | Section 12 of the application outlines required supporting documentation that must accompany the form upon submission. |
| Revalidation | Current Medicare providers may need to revalidate their enrollment periodically, as mandated by CMS. This process requires resubmission of the application. |
| Termination Process | Providers wishing to voluntarily terminate their Medicare billing privileges must complete specific sections of the CMS-855B and submit it to the designated Medicare Administrative Contractor (MAC). |
| Submission Details | Completed forms must be mailed to the designated MAC, which serves the provider’s state, along with original signatures and all required documentation. |
| Application Fee | An application fee may be required upon initial enrollment or revalidation. This fee must be paid online before submitting the CMS-855B. |
| Relevant Regulations | The application process and requirements can be found in the Code of Federal Regulations (CFR), specifically in sections 424.516 and 489.18. |
Guidelines on Utilizing Cms 855B
Completing the CMS 855B form is an essential step for clinics, group practices, and other suppliers looking to enroll in the Medicare program. This process ensures a smooth submission, allowing you to receive a Medicare billing number and comply with necessary regulations. Follow these steps carefully to fill out the form accurately.
- Start with Section 1 to provide basic information.
- Indicate your reason for submitting the application by checking the appropriate box.
- In Section 2, enter the Legal Business Name (LBN) and Tax Identification Number (TIN). Ensure these match the details used to obtain your NPI.
- Provide your National Provider Identifier (NPI) in the designated sections.
- Complete all applicable sections as indicated, including additional attachments if required (e.g., Attachment 1 for ambulance suppliers).
- Fill out the contact information for your business, confirming the correspondence address is correct.
- If applicable, include the Electronic Funds Transfer (EFT) Authorization Agreement along with a voided check or bank letter.
- Review all entries to ensure completeness and accuracy. Double-check that all required sections are filled out.
- Sign and date Section 15 of the form.
- Attach all required supporting documentation as specified in Section 12.
- Keep a copy of the completed application for your records.
- Mail the signed application and supporting documents to your designated Medicare Administrative Contractor (MAC) according to the information provided on the form.
By following these steps, you will help prevent delays in the enrollment process. Ensure all information is accurate and up-to-date to facilitate timely processing of your application.
What You Should Know About This Form
What is the CMS-855B form?
The CMS-855B form is an application used by clinics, group practices, and other suppliers to enroll in the Medicare program. By completing this form, these entities can obtain a Medicare billing number, allowing them to submit claims for Medicare services provided to their patients.
Who needs to submit the CMS-855B application?
This form is necessary for any clinic, group practice, or other supplier that plans to bill Medicare. It is required for those enrolling for the first time, changing their tax identification number, revalidating their enrollment, or reactivating their Medicare billing privileges. Essentially, if you intend to provide services billed to Medicare, you will need to complete this application.
How do I apply for an NPI in conjunction with the CMS-855B?
To enroll in Medicare, you must have a National Provider Identifier (NPI). You can apply for your NPI online at the National Plan and Provider Enumeration System (NPPES) website. It's important to complete this step prior to filling out the CMS-855B form, as you will need your NPI to be included on the application.
What happens if my application is incomplete?
Incompletely filled applications may delay your enrollment process. The Medicare Administrative Contractor (MAC) may return your application if fields are missing or if the application is handwritten. Always ensure that all required fields are completed before submission.
How should I submit the completed CMS-855B form?
The completed form and any required supporting documents should be mailed to your designated Medicare Administrative Contractor (MAC). You can find the appropriate mailing address by visiting the CMS website and checking the state-specific MAC information.
What is the legal business name and tax identification number requirement?
Your Legal Business Name (LBN) and Tax Identification Number (TIN) must match exactly with the information used to obtain your NPI. Ensuring this consistency is vital to avoid issues during the enrollment process.
Are there any fees associated with submitting the CMS-855B form?
Yes, there are application fees that must be paid when you initially enroll, add a new business location, or revalidate your enrollment. You should pay the fee prior to submitting your application to avoid processing delays.
What supporting documentation do I need to include with my application?
The application will require various supporting documents, depending on your specific situation. A list of required documentation can be found in Section 12 of the application. Make sure to review this list carefully and include all necessary documents to support your application.
What is the importance of electronic funds transfer authorization?
If applicable, including an Electronic Funds Transfer (EFT) Authorization Agreement alongside your CMS-855B form is crucial. This agreement allows Medicare to directly deposit payments into your bank account, streamlining the payment process for services rendered.
How can I avoid delays in my enrollment process?
To help ensure your application moves smoothly through the process, double-check that all fields are completed accurately, the correct legal business name and TIN are provided, and all supporting documents are included. Additionally, remember to sign and date your application!
Common mistakes
Filling out the CMS 855B form can seem daunting, but careful attention to detail can make the process smoother. Unfortunately, many applicants make common mistakes that can lead to delays or even denials. One of the most frequent errors occurs when providers fail to use the most current version of the form. The Medicare program updates its forms periodically, and using an outdated version can result in automatic rejection. Always check for the latest version on the CMS website before beginning the application.
Another prevalent mistake is not providing accurate and matching information. Specifically, the Legal Business Name (LBN) and Tax Identification Number (TIN) must match exactly with what is on the tax documents and what was used to obtain the National Provider Identifier (NPI). Discrepancies here can lead to complications during the enrollment process, so double-check these details carefully.
Additionally, many applicants overlook the importance of providing a correspondence address that is up-to-date and accurate. This address is where the Medicare Administrative Contractor (MAC) will send important communication regarding your enrollment. If this information is incorrect, you may miss critical updates or requests, which can further delay the process.
A significant error occurs when applicants assume that optional sections can be filled out flexibly. While optional fields may not need to be completed, they should not be ignored if relevant information can be provided. Keeping this information updated can be crucial in maintaining a smooth relationship with Medicare.
Failure to include supporting documentation is another common pitfall. All required documents must accompany the application; without them, the application may be returned or rejected. A comprehensive checklist can help ensure that everything necessary is included before submission.
Signing and dating the application is mandatory, yet many people forget to do this. An unsigned application may be considered incomplete and can be returned, causing further delays. Make sure to read through the form and confirm that all required sections have been signed where necessary.
Finally, one major oversight occurs when applicants forget to pay the required application fee upfront. The process requires payment upon initial enrollment, which should be completed prior to submission of the application. Skipping this step can lead to immediate delays; thus, it’s critical to keep this in mind as you prepare to submit your form.
Documents used along the form
The CMS-855B form is essential for clinics, group practices, and other suppliers enrolling in the Medicare program. However, several other documents are often needed to support the application and ensure a successful enrollment process. Below is a list of essential forms and documents typically used alongside the CMS-855B.
- National Provider Identifier (NPI) Application: Required to obtain a unique identification number for healthcare providers. This number is crucial for billing Medicare.
- Electronic Funds Transfer (EFT) Authorization Agreement: Optional but recommended for suppliers who want Medicare payments directly deposited into their bank accounts. Accompanied by a voided check or bank letter.
- Tax Identification Number (TIN) Documentation: Proof of the TIN used for the business, which must match the one provided in the CMS-855B to avoid discrepancies.
- Proof of Business Structure: Documents like Articles of Incorporation or a partnership agreement to verify the legal business structure of the organization.
- Ownership and Control Disclosure Information: Required to disclose the individuals and entities with controlling interests in the practice. Helps ensure transparency.
- Licensure Documents: Copies of state licenses or certifications for all healthcare providers involved, ensuring they are qualified to offer services.
- Compliance Plan: A written plan that outlines the organization’s policies for adhering to federal regulations and standards in healthcare.
- Additional Attachments as Needed: Any further documentation specific to the type of supplier or unique circumstances of the organization may be required to complete the application.
Submitting the necessary forms and documentation with the CMS-855B is crucial for expedient processing of the Medicare enrollment application. Being thorough and organized will greatly reduce the risk of delays and increase the chance of a successful outcome.
Similar forms
-
CMS-855A Form: This application is intended for individual physicians and non-physician practitioners to enroll in the Medicare program. Similar to the CMS-855B, it collects essential information to verify the provider’s eligibility for billing Medicare and requires supporting documentation. Both forms ensure that providers meet Medicare standards before accepting patients.
-
CMS-855S Form: Used for suppliers of Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS), this form assists suppliers in enrolling in the Medicare program. Like the CMS-855B, the CMS-855S Form requires comprehensive details about the organization or supplier and specific documentation to satisfy the Medicare requirements.
-
CMS-587 Form: This form is for the Electronic Funds Transfer (EFT) authorization, enabling providers to receive Medicare payments directly into their bank accounts. While the CMS-855B collects enrollment information, the CMS-587 focuses on payment processing. However, both forms are crucial for managing gains from Medicare billing.
-
CMS-855R Form: This application is for reassigning Medicare benefits, allowing providers to assign their payments to another entity. As with the CMS-855B, the CMS-855R mandates that comprehensive information is reported regarding the provider relationships and contractual agreements necessary for proper billing.
Dos and Don'ts
- Ensure that you are using the most current version of the CMS-855B form.
- Type all information on the form; handwritten applications may be returned.
- Complete all required sections without skipping any.
- Provide your NPI in all applicable sections of the form.
- Attach all necessary supporting documentation as specified.
- Keep a copy of your completed application for your records.
- Submit the form to your designated Medicare Administrative Contractor (MAC) in a timely manner.
- Sign and date the application in section 15 prior to submission.
- Make sure the legal business name on the application matches tax documents.
- Include the required application fee with your submission if applicable.
Don't:
- Use a handwritten form; it could result in delays.
- Skip any required fields even if you think they are unimportant.
- Submit your application without verifying that your NPI matches exactly.
- Fail to include all supporting documents as requested.
- Neglect to report changes within the required timeframe.
- Attempt to revalidate without being instructed by your MAC.
- Detach the application fee from your submission.
- Ignore the specific instructions applicable to your supplier type.
- Forget to check that the correspondence address is accurate.
- Submit your application to the incorrect MAC; ensure it’s correct for your state.
Misconceptions
Here are four common misconceptions about the CMS 855B form that often create confusion for applicants:
- Only new suppliers need to fill out the CMS 855B. Many believe this form is only for new applicants. In reality, current suppliers must also use it to update their information or revalidate their enrollment.
- Handwritten applications are acceptable. Some may think that it’s fine to submit a handwritten CMS 855B. However, all information must be typed for the application to be considered.
- The CMS 855B can be submitted without supporting documents. An assumption exists that applicants can send the form alone. Supporting documentation is a crucial part of the application process and must be included.
- Submitting the CMS 855B guarantees automatic enrollment. Many believe that simply filling out and sending in the CMS 855B means they’ll automatically be enrolled. However, the application must be processed and approved by the Medicare Administrative Contractor (MAC) before enrollment is official.
Key takeaways
The CMS-855B form is essential for clinics, group practices, and suppliers to enroll in the Medicare program.
Accuracy is crucial. Ensure that all entries match your tax documents, especially the Legal Business Name (LBN) and Tax Identification Number (TIN).
Lorem ipsum dolor
Individuals must possess a Type 2 National Provider Identifier (NPI) before submitting the application.
Required information must be provided in the form; any optional fields should be completed if relevant.
Handwritten parts can result in application delays. Always type the form.
CMS may require additional documentation. Respond promptly to requests to avoid delays.
Keep a copy of the completed application for your records.
To ensure a smooth enrollment process, submit the Electronic Funds Transfer (EFT) Authorization Agreement, if applicable.
Mail the application to your designated Medicare Administrative Contractor (MAC) using the correct address from the CMS website.
Browse Other Templates
Dmv Forms Florida - A certification statement must be completed by an authorized official.
How Much Does It Cost to Make a Llc - Details about previous owners may be necessary for some filings.
Member Register Format - Failure to provide accurate information may delay the registration process.