Fill Out Your Complete Physical Examination Form
The Complete Physical Examination form is an essential tool used by healthcare providers to assess an individual's overall health. This comprehensive document collects vital signs, including temperature, heart rate, and blood pressure, which provide crucial data to evaluate a patient's current state. It includes a systematic review of various bodily systems, such as general appearance, head and neck, cardiovascular, respiratory, abdominal, extremities, neurological, psychiatric, and skin assessments. Each section of the form contains specific abbreviations and normal findings, enabling healthcare professionals to communicate efficiently. Detailed documentation on areas like the genitourinary and rectal examinations ensures thorough evaluations, leading to accurate diagnoses and treatment plans. Ultimately, the form not only serves as a critical record for medical professionals but also empowers patients by highlighting their health status and guiding potential interventions.
Complete Physical Examination Example

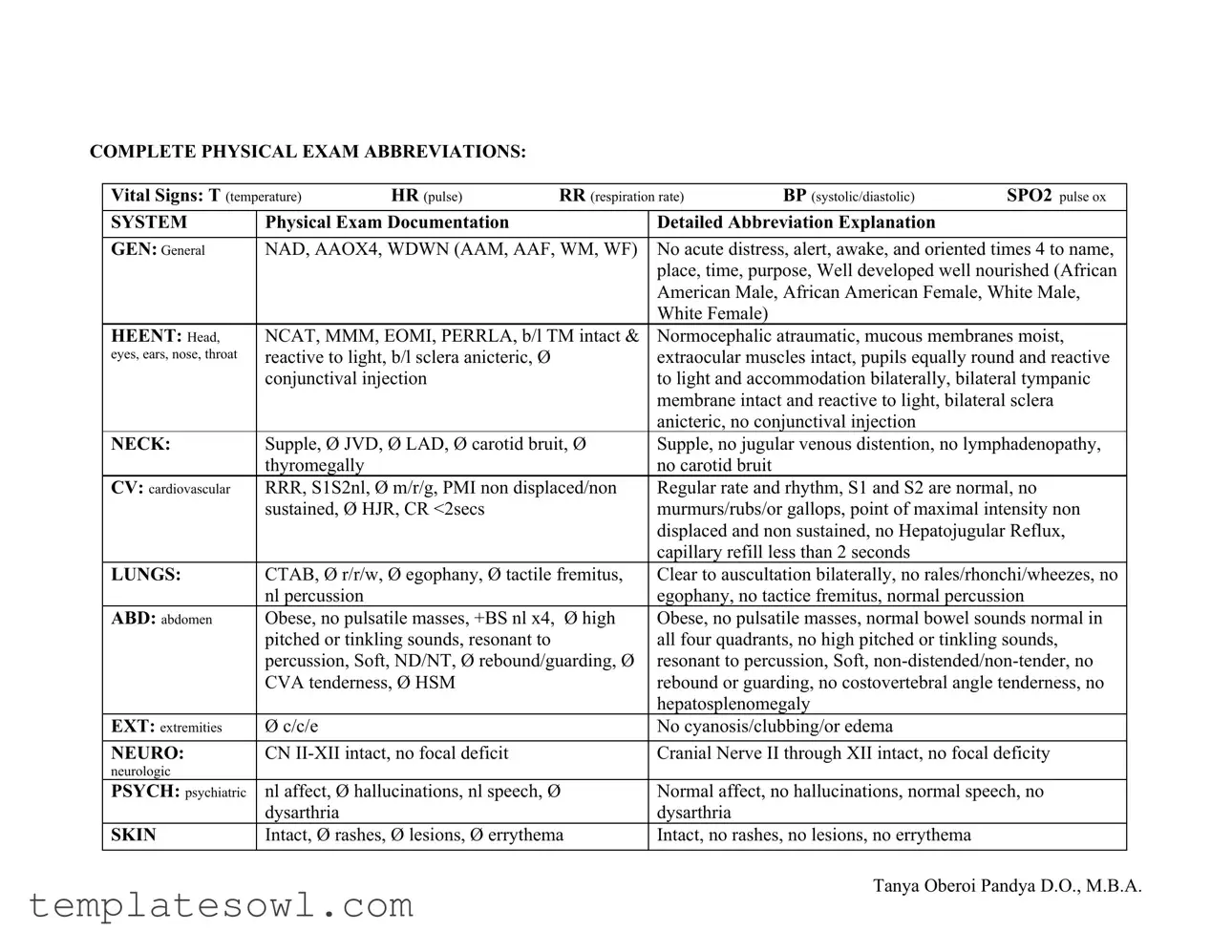
COMPLETE PHYSICAL EXAM ABBREVIATIONS:
Vital Signs: T (temperature) |
HR (pulse) |
RR (respiration rate) |
BP (systolic/diastolic) |
SPO2 pulse ox |
||
|
|
|
|
|
||
SYSTEM |
Physical Exam Documentation |
|
Detailed Abbreviation Explanation |
|
||
|
|
|
||||
GEN: General |
NAD, AAOX4, WDWN (AAM, AAF, WM, WF) |
No acute distress, alert, awake, and oriented times 4 to name, |
||||
|
|
|
|
place, time, purpose, Well developed well nourished (African |
||
|
|
|
|
American Male, African American Female, White Male, |
||
|
|
|
|
White Female) |
|
|
HEENT: Head, |
NCAT, MMM, EOMI, PERRLA, b/l TM intact & |
Normocephalic atraumatic, mucous membranes moist, |
||||
eyes, ears, nose, throat |
reactive to light, b/l sclera anicteric, Ø |
|
extraocular muscles intact, pupils equally round and reactive |
|||
|
conjunctival injection |
|
to light and accommodation bilaterally, bilateral tympanic |
|||
|
|
|
|
membrane intact and reactive to light, bilateral sclera |
||
|
|
|
|
anicteric, no conjunctival injection |
|
|
NECK: |
Supple, Ø JVD, Ø LAD, Ø carotid bruit, Ø |
Supple, no jugular venous distention, no lymphadenopathy, |
||||
|
thyromegally |
|
|
no carotid bruit |
|
|
CV: cardiovascular |
RRR, S1S2nl, Ø m/r/g, PMI non displaced/non |
Regular rate and rhythm, S1 and S2 are normal, no |
||||
|
sustained, Ø HJR, CR <2secs |
|
murmurs/rubs/or gallops, point of maximal intensity non |
|||
|
|
|
|
displaced and non sustained, no Hepatojugular Reflux, |
||
|
|
|
|
capillary refill less than 2 seconds |
|
|
LUNGS: |
CTAB, Ø r/r/w, Ø egophany, Ø tactile fremitus, |
Clear to auscultation bilaterally, no rales/rhonchi/wheezes, no |
||||
|
nl percussion |
|
|
egophany, no tactice fremitus, normal percussion |
||
ABD: abdomen |
Obese, no pulsatile masses, +BS nl x4, |
Ø high |
Obese, no pulsatile masses, normal bowel sounds normal in |
|||
|
pitched or tinkling sounds, resonant to |
|
all four quadrants, no high pitched or tinkling sounds, |
|||
|
percussion, Soft, ND/NT, Ø rebound/guarding, Ø |
resonant to percussion, Soft, |
||||
|
CVA tenderness, Ø HSM |
|
rebound or guarding, no costovertebral angle tenderness, no |
|||
|
|
|
|
hepatosplenomegaly |
|
|
EXT: extremities |
Ø c/c/e |
|
|
No cyanosis/clubbing/or edema |
|
|
|
|
|
|
|||
NEURO: |
CN |
|
Cranial Nerve II through XII intact, no focal deficity |
|||
neurologic |
|
|
|
|
|
|
PSYCH: psychiatric |
nl affect, Ø hallucinations, nl speech, Ø |
Normal affect, no hallucinations, normal speech, no |
||||
|
dysarthria |
|
|
dysarthria |
|
|
SKIN |
Intact, Ø rashes, Ø lesions, Ø errythema |
Intact, no rashes, no lesions, no errythema |
|
|||
|
|
|
|
|
|
|
Tanya Oberoi Pandya D.O., M.B.A.

GU: (genitourinary) |
Male: Ø rashes, Ø penile discharge, penile shaft s |
Male: no rashes, no penile discharge, penile shaft without |
|
masses or lesions, Ø inguinal hernia, Ø inguinal |
masses or lesions, no inguinal hernia, no inguinal |
|
LAD, b/l testicles nl in consistency s hydrocele or |
lymphadenopathy, bilateral testicles normal in consistency |
|
varicocele, Ø hypospadias/epispadias |
without hydrocele or varicocele, no hypospadias or |
|
|
epispadias |
Pelvic: |
Ø rashes, nl bartholin gland, vaginal mucosa nl |
No rashes, normal bartholin gland, vaginal mucosa of normal |
|
consistency s atrophy or discharge, cervical os s |
consistency without atrophy or discharge, cervical os without |
|
discharge |
discharge |
|
Bimanual: Ø CMT Ø VB Ø discharge Ømasses |
Bimanual: No cervical motion tenderness, no vaginal |
|
|
bleeding, no discharge, no masses |
RECTAL |
Ø BRBPR, Ø melena, Ø masses, nl sphincter |
No bright red blood per rectum, no melena, no masses, |
|
tone, Ø ext/int hemorrhoids, prostate walnut size |
normal sphincter tone, no external or internal hemorrhoids, |
|
s nodularity or hypertrophy, Ø prostate tenderness |
prostate walnut size without nodularity or hypertrophy, no |
|
|
prostate tenderness |
LYMPH: |
Ø LAD |
No lymphadenopathy |
(lymphatic) |
|
|
Mmsk: |
nl ROM, Ø joint swelling or errythema |
Normal range of motion, no joint swelling or errythema |
(musculoskeletal) |
|
|
Tanya Oberoi Pandya D.O., M.B.A.
COMMON ABREVIATIONS ENCOUNTERED IN PRACTICE:
CC |
Chief complaint |
HPI |
History of Present Illness |
ROS |
Review of System |
PMH |
Past Medical History |
NKDA |
No known Drug Allergies |
CP |
Chest Pain |
|
|
SOB |
Shortness of Breath |
DOE |
Dyspnea on exertion |
PND |
If talking cardiac: Paroxysmal Nocturnal Dyspnea |
|
If talking Upper respiratory: Post Nasal Drip |
JVD |
Jugular Venous Distention |
HJR |
|
LE edema |
Lower Extremity edema |
No c/c/e |
No cyanosis/clubbing/edema |
No r/r/w |
No Rales/rhonchi/wheezes |
No m/r/g |
No murmurs/rubs/gallops |
CTAB |
Clear To Auscultation Bilaterally |
RRR |
Regular Rate and Rhythm |
S1S2 nl |
S1 (first heart sound) and S2 (second heart sound) |
|
are normal in auscultation |
EKG: |
|
LAD |
Left Axis Deviation |
RAD |
Right Axis Deviation |
RAE |
Right Atrial Enlargement |
LAE |
Left Atrial Enlargement |
LVH |
Left Ventricular Hypertrophy |
NSR |
Normal Sinus Rhythm |
LAD |
Lymphadenopathy |
EOMI |
|
PERRL |
Pupils Equally Round and Reactive to light |
Cranial Nerves two through twelve intact |
|
MMSE |
Mini Mental Status Exam |
No T/A/D |
No Tobacco/Alcohol/IV drug use |
Ctx |
Contractions |
Fx |
Fracture or function (depending on context) |
P.V. |
Per Vagina |
P.R. |
Per Rectum |
SBP |
Systolic Blood Pressure |
DBP |
Diastolic Blood Pressure |
HR |
Heart Rate |
RR |
Respiratory Rate |
SPO2 |
Pulse Oximetry |
BRBPR |
Bright Red Blood Per Rectum |
DTR |
Deep Tendon Reflexes |
ARF |
Acute Renal Failure |
CRI |
Chronic Renal Insufficiency |
CRF |
Chronic Renal Failure |
FEN/GI |
Fluids, Electrolytes, and |
|
Nutrition/Gastroenterology |
AAOX3 |
Alert, awake, and Oriented times 3 (to person, |
|
time, place) |
NAD |
No Acute Distress |
MMM |
Mucus Membranes Moist |
ND/NT |
Non Distended/Non Tender |
BSx4 |
Bowel Sounds present in all 4 quadrants |
N, V |
Nausea, Vomiting |
S.Q. |
Subcutaneous |
PTCA |
Percutaneous Transluminal Coronary Angioplasty |
PCI |
Percutaneous Intervention (cardiac) |
CAD |
Coronary Artery Disease |
ICD |
Implantable Cardioverter Defibrillator |
CABG |
Coronary Artery Bypass Graft |
VB |
Vaginal Bleeding |
FM |
Fetal Movement |
CMT |
Cervical motion tenderness |
LMP |
Last menstrual period |
NSVD |
Normal Spontaneous Vaginal Delivery |
PPROM |
Preterm Premature Rupture of Membranes |
PROM |
Premature Rupture of Membranes |
LTCS |
Low Transverse Cesarean Section |
VBAC |
Vaginal Birth After Cesarean Section |
EBL |
Estimated Blood Loss |
EGA |
Expected Gestational Age |
EDC |
Expected Date of Confinement (baby’s due date) |
Tanya Oberoi Pandya D.O., M.B.A.
IUP |
|
FHT |
Fetal Heart Tones |
TAH/BSO |
Total Abdominal Hysterectomy with Bilateral |
|
Salpigoopherectomy (i.e. no uterus/ tubes, no |
|
ovaries) |
TAH |
Total abdominal hysterectomy |
BTL |
Bilateral Tubal Ligation |
PTL |
Preterm Labor |
CVA |
Cerebrovascular accident |
TIA |
Transient Ischemic Attack |
No T/A/D |
No tobacco/alcohol/drugs |
Supp. |
Suppository |
Wt |
Weight |
HA |
Headache |
Palp |
Palpitations |
Sptm |
Sputum |
AGE |
Acute gastroenteritis |
URI |
Upper respiratory infection |
FH or FHx |
Family History |
SH or SHx |
Social history |
PVD |
Peripheral vascular disease |
DJD |
Degenerative joint disease |
OA |
Osteoarthritis |
POD |
Post Op Day |
Lap. chole. |
Laparoscopic Cholecystectomy |
Lap. Appy |
Laparoscopic appendectomy |
AKA |
Above the Knee Amputation |
BKA |
Below the Knee Amputation |
NKDA |
No Known Drug Allergies |
Hb |
Hemoglobin |
Hct |
Hematocrit |
H/H |
Hemoglobin and hematocrit |
CXR |
Chest |
BAL |
|
s/p |
Status post… |
h/o |
History of… |
wnl |
Within normal limits |
NC |
Non contributory (if written under family history) |
OA |
Osteoarthritis |
RCT |
Rotator cuff tear |
RTC |
Return to Clinic |
FOB |
Fecal Occult Blood |
AAAAbdominal Aortic Aneurysm
MURMURS:
AI |
Aortic Insufficiency |
AS |
Aortic Stenosis |
MR |
Mitral Regurgitation |
MS |
Mitral Stenosis |
TI |
Tricuspid Insufficiency |
PS |
Pulmonic Stenosis |
PI |
Pulmonic Insufficiency |
AVR |
Aortic Valve Replacement |
MVR |
Mitral Valve Replacement |
MVP |
Mitral Valve Prolapse |
AV |
Atrioventricular |
AVM |
|
UA c C&S |
Urinalysis with Culture and Sensitivity |
VSS |
Vital Signs Stable |
TURP |
Trans Uretheral Prostatectomy |
TAB |
Therapeutic Abortion |
VIP |
Voluntary Interruption of Pregnancy |
PNA |
Pneumonia |
ddx |
Differential Diagnosis |
abx |
Antibiotics |
bx |
Biopsy |
cx |
Culture |
Ad lib |
As much as needed |
c/o |
Complain of |
QD |
Every day |
bid |
Twice a day |
tid |
Three times a day |
qid |
Four times a day |
Q.O.D. |
Every Other Day |
Tanya Oberoi Pandya D.O., M.B.A.
Form Characteristics
| Fact Name | Detail |
|---|---|
| Purpose | The Complete Physical Examination form is utilized to document a thorough health assessment of a patient. |
| Governing Law | In New York, for example, the form follows the New York State Public Health Law § 2164 for school physicals. |
| Vital Signs | Includes important measurements such as temperature, heart rate, respiration rate, blood pressure, and oxygen saturation. |
| General Examination | Describes the patient's overall condition including alertness and signs of distress. |
| Abbreviations | This form employs numerous abbreviations to streamline documentation, like "NAD" for "No Acute Distress." |
| Systematic Review | A detailed assessment is conducted across several systems including neurological, cardiovascular, respiratory, and gastrointestinal. |
| Common Findings | Conditions observed can range from normal findings to signs of underlying medical issues, such as rashes or murmurs. |
| Patient History | This form may incorporate relevant patient history components, including past medical history and social history. |
| Documentation Requirement | Healthcare providers must complete this form as part of regulatory compliance and patient care standards. |
Guidelines on Utilizing Complete Physical Examination
Completing the Complete Physical Examination form requires careful attention to detail. Use the following steps to ensure accurate and thorough documentation of your health status. After filling out the form, submit it to the appropriate medical staff for further evaluation and use in your ongoing healthcare.
- Write your full name at the top of the form.
- Fill in the date of the examination.
- Provide your date of birth.
- Indicate your chief complaint (CC), briefly stating the reason for your visit.
- Complete the History of Present Illness (HPI) section by describing any relevant medical concerns.
- List your past medical history (PMH), including any chronic conditions or significant health issues.
- In the Review of Systems (ROS) section, indicate any current symptoms by marking each relevant item.
- Record vital signs, including temperature (T), heart rate (HR), respiration rate (RR), blood pressure (BP), and oxygen saturation (SPO2) readings.
- Document findings from the physical examination in the designated sections, making sure to be consistent with standard abbreviations.
- Complete the genitourinary (GU) section with appropriate details, ensuring accuracy for both males and females.
- Sign and date the form at the bottom, confirming that all information is complete and accurate.
What You Should Know About This Form
What is the Complete Physical Examination form used for?
The Complete Physical Examination form serves as a comprehensive tool for healthcare providers to capture the health status of an individual. It allows for a systematic evaluation of various bodily systems, including vital signs, cardiovascular health, respiratory function, and neurological integrity. This examination is essential for establishing a baseline of health, identifying any existing medical conditions, and guiding further diagnostic or therapeutic decisions.
What are the key components included in the form?
The form includes several critical components that document the examination findings. Vital signs such as temperature, pulse, and blood pressure are recorded at the beginning. Following this, a thorough review of each body system is assessed. Common sections include General Appearance, Head, Eyes, Ears, Nose, Throat (HEENT), Cardiovascular (CV), Respiratory, Gastrointestinal, and Neurological statuses, among others. Each section utilizes specific abbreviations for detailed evaluation while maintaining clear and concise documentation.
How do the abbreviations in the form help streamline the examination process?
Abbreviations simplify documentation, allowing healthcare providers to quickly record their findings without compromising detail. For instance, terms like “RRR” for Regular Rate and Rhythm or “CTAB” for Clear To Auscultation Bilaterally make the recording process more efficient. These shortened forms enhance communication between healthcare professionals and help in delivering timely patient care.
Why is it important to maintain the accuracy of the Complete Physical Examination form?
Accurate documentation is indispensable for providing quality healthcare. Errors in the Complete Physical Examination form can lead to misdiagnosis, inappropriate treatment plans, and ultimately, negative patient outcomes. Therefore, meticulous attention to detail during examinations and proper recording of findings ensures that all healthcare providers have access to reliable patient information, fostering informed medical decision-making.
What should patients expect during a physical examination?
Patients undergoing a physical examination can expect a thorough review of their medical history, followed by various assessments that inspect different body systems. They may be asked to perform simple tasks like breathing deeply or moving limbs, enabling healthcare providers to evaluate function and coordination. Throughout the process, providers should communicate openly, ensuring that patients are comfortable and informed about each step of the examination.
Common mistakes
Completing a Complete Physical Examination form can be straightforward, but common mistakes often lead to inaccurate or incomplete information. One frequent error is failing to include vital signs. These measurements—temperature, pulse, respiration rate, and blood pressure—are crucial for assessing overall health and should never be overlooked.
Another common mistake is neglecting to provide a clear chief complaint (CC). This section allows healthcare providers to understand the primary reason for the examination. Omitting this detail can create confusion and hinder effective communication between you and your healthcare provider.
Many individuals also struggle with abbreviations. While they are meant to simplify communication, unfamiliarity with medical abbreviations can lead to misunderstandings. Always verify that you understand each abbreviation before using it. If you’re unsure about any term, clear it up with your healthcare provider beforehand.
Another area of concern is inconsistent information. This includes providing different answers regarding symptoms or medical history when compared to previous visits. This inconsistency can create doubt and complicate your medical records. Make sure your information is accurate and as up-to-date as possible.
It's easy to forget personal health details, such as past medical history or known drug allergies (NKDA). Leaving these sections blank can prevent healthcare providers from delivering the best care. Always take the time to review this crucial information before submitting the form.
In addition, some people skip details about medication use. This includes both prescribed medications and over-the-counter drugs. Omitting this information may hinder the effectiveness of treatments and lead to harmful drug interactions. Always list all medications you are taking.
Another oversight is disregarding your mental health status. Issues like anxiety or depression are vital signs of overall health. Providers need this information to monitor your well-being effectively, so don’t leave this section blank.
Forgetting to mention lifestyle factors can also be a mistake. Things like diet, exercise, and substance use greatly affect health outcomes. Transparency in these areas can lead to more tailored and effective care.
Lastly, individuals often fail to review the completed form before submission. This final step is crucial for catching mistakes or omissions. Take a moment to double-check your form to ensure everything is complete and accurate. This small effort can vastly improve the quality of your healthcare experience.
Documents used along the form
The Complete Physical Examination form is an essential tool used in medical practice to assess a patient's overall health. Alongside this form, several other documents are often utilized to capture additional vital information and facilitate effective patient care. Below is a list of complementary forms that commonly accompany the Complete Physical Examination form.
- Medical History Questionnaire: This document gathers a comprehensive background on the patient's past and present health, including chronic illnesses, surgeries, allergies, and medications. It helps healthcare providers understand the patient’s medical journey.
- Consent Forms: Consent forms are necessary to obtain permission from patients for specific procedures or treatments. They ensure that patients are informed about the risks and benefits and agree to the proposed care plan.
- Lab Request Forms: These forms are used to order laboratory tests, such as blood work or urinalysis. They specify the tests needed and provide the necessary patient identification information for accurate processing and results tracking.
- Immunization Records: This document outlines a patient's vaccination history. Keeping an up-to-date immunization record is crucial for assessing the patient's preventive health measures and fulfilling regulatory requirements.
- Referral Forms: When a patient requires specialized care, referral forms direct them to another healthcare provider. These documents typically summarize the patient’s condition and the purpose of the referral, ensuring that specialists have the necessary context.
- Follow-Up Appointment Schedule: This document lists recommended follow-up visits and screenings based on the examination findings. It helps ensure continuity of care and encourages patients to stay engaged in their health management.
- Prescription Forms: When medications are prescribed as a result of the examination, prescription forms are completed. These include details about the medication, dosage, and instructions for the patient.
- Patient Education Materials: These are informational resources provided to patients to help them understand their health conditions and promote self-care. They can cover topics like diet, exercise, and medication adherence.
Utilizing these forms in conjunction with the Complete Physical Examination form enhances communication between healthcare providers and patients. This comprehensive approach not only promotes effective treatment plans but also supports better patient outcomes and satisfaction.
Similar forms
- Patient History Form: Similar to the Complete Physical Examination (CPE) form, a Patient History Form gathers crucial background information about a patient's medical history, family history, and past surgeries. It provides context for the CPE, helping healthcare providers understand any underlying issues.
- Wellness Exam Form: This form focuses on preventive care and screenings, similar to the CPE form. Both documents aim to assess overall health and identify any potential risk factors for diseases.
- Emergency Room Triage Form: Just like the CPE form, this document assesses a patient's condition using vital signs and physical examination. It helps prioritize patient care in emergency situations.
- Referral Form: A Referral Form captures a patient's details and the reason for the referral, paralleling the CPE's approach of documenting vital signs and health observations for continuity of care.
- Annual Physical Exam Form: This is another preventative care document, capturing similar information as the CPE. Both forms are designed to evaluate a patient’s health status annually.
- Pre-Operative Assessment Form: Just like the CPE form, this assesses a patient's health and risks before a surgical procedure. Both forms include evaluations of systems and vital signs.
- Insurance Enrollment Form: Though primarily administrative, this form sometimes requires a summary of health statuses, akin to how the CPE compiles current health information necessary for care coverage decisions.
- Patient Consent Form: It outlines the patient’s understanding of procedures and risks, similar to the CPE's role in informing patients about their health status prior to treatment or testing.
- Discharge Summary: After a patient leaves care, this document summarizes findings from the CPE and treatment provided, mirroring the CPE’s goal of documenting health information.
- Chronic Care Management Plan: This plan outlines ongoing care for patients with chronic conditions. Similar to the CPE, it reviews vital signs and overall health to guide long-term management strategies.
Dos and Don'ts
When filling out the Complete Physical Examination form, attention to detail and accuracy is essential. The following list outlines important actions to take and avoid during this process.
- Do: Carefully read all instructions provided with the form.
- Do: Provide clear and accurate information regarding medical history and current health status.
- Do: Use correct abbreviations as specified to ensure clarity.
- Do: Review the form for completeness before submission.
- Don't: Leave any sections blank unless instructed.
- Don't: Provide vague answers; specifics are important for accurate assessment.
Misconceptions
Misconceptions can often lead to misunderstandings, especially regarding important medical documents like the Complete Physical Examination form. Below are five common misconceptions and clarifications about this form.
- The form is only required for new patients. Many believe that the Complete Physical Examination form is only necessary for new patients during their initial visit. In reality, this form serves as a vital tool for ongoing patient assessments, enabling healthcare providers to track changes in health status over time. It is crucial for both new and returning patients.
- The form is overly complicated and difficult to understand. While the Complete Physical Examination form contains medical abbreviations and terminology, healthcare professionals are trained to interpret these details. The intention is to provide a thorough evaluation without burdening the patient. Clarity may improve as patients familiarize themselves with the information.
- All examination details are shared with third parties automatically. Some people worry that their medical information will be shared without consent. However, medical confidentiality laws protect patient information from unauthorized access. The Complete Physical Examination form is kept secure and shared only with authorized healthcare providers, unless the patient grants permission otherwise.
- The form only focuses on physical health. Many assume that the examination is solely about physical health, overlooking the mental and emotional aspects of care. The Complete Physical Examination includes assessments of psychological well-being, ensuring a comprehensive approach to health that incorporates mental health evaluations alongside physical checks.
- Patients must be symptom-free to undergo a complete examination. A common belief is that only healthy individuals can receive a physical exam because they have no complaints. In fact, physical examinations are crucial regardless of existing symptoms. They can help identify underlying issues early, even when a patient feels fine, promoting proactive health management.
Understanding these misconceptions can lead to a more informed approach to health assessments and enhance the patient experience during medical visits.
Key takeaways
1. Accurate Completion is Essential: Ensure all sections of the Complete Physical Examination form are filled out accurately. Missing or incorrect information may lead to misdiagnosis or inappropriate treatment.
2. Understand the Abbreviations: Familiarize yourself with the common abbreviations used in the examination. For example, "NAD" means "no acute distress," and "RRR" indicates "regular rate and rhythm." This will help in both filling out the form and understanding the findings.
3. Be Thorough with Documentation: Document all observations from each body system, including vital signs and any abnormalities noted. A thorough assessment provides a comprehensive picture of the patient's health.
4. Review Past Medical History: Take time to review the patient's past medical history (PMH) and any known drug allergies (NKDA). This information is crucial for ongoing care and treatment decisions.
5. Keep a Copy for Records: After filling out the form, keep a copy for your records. This allows for better tracking of a patient’s progress and helps when comparing future examinations.
Browse Other Templates
Jackson National Insurance - Detail any disciplinary actions on the background investigation form.
Dd Form 518 - The SSN helps to minimize confusion due to similar names among drivers.