Fill Out Your Coventry Claim Form
The Coventry Claim form is a crucial document for providers challenging claim payments made by Coventry Health Care. Understanding its components ensures that you effectively navigate the appeal process. This form is utilized across various products, including Commercial, Individual Medicare, Medicaid, Healthy Kids, and Long Term Care. It addresses reasons for disputes such as incorrect claims payment or medical appeals. Guidelines require that claims be submitted within 35 days of receiving the Remittance Advice. The form collects essential information, including member details, provider information, and specifics about the dates of service. Additionally, it prompts for necessary attachments, such as explanation of benefits and medical records to support your dispute. Accurate completion is vital, as it necessitates using one form per claim denial and allows for multiple claims only if they share the same reason for review. Incomplete submissions, particularly for inpatient service appeals, may delay the review process, as full medical records must accompany them. For comprehensive guidance, the Provider Manual serves as a valuable resource. Ensuring that every detail is correctly provided can significantly impact the outcome of your claims reconsideration.
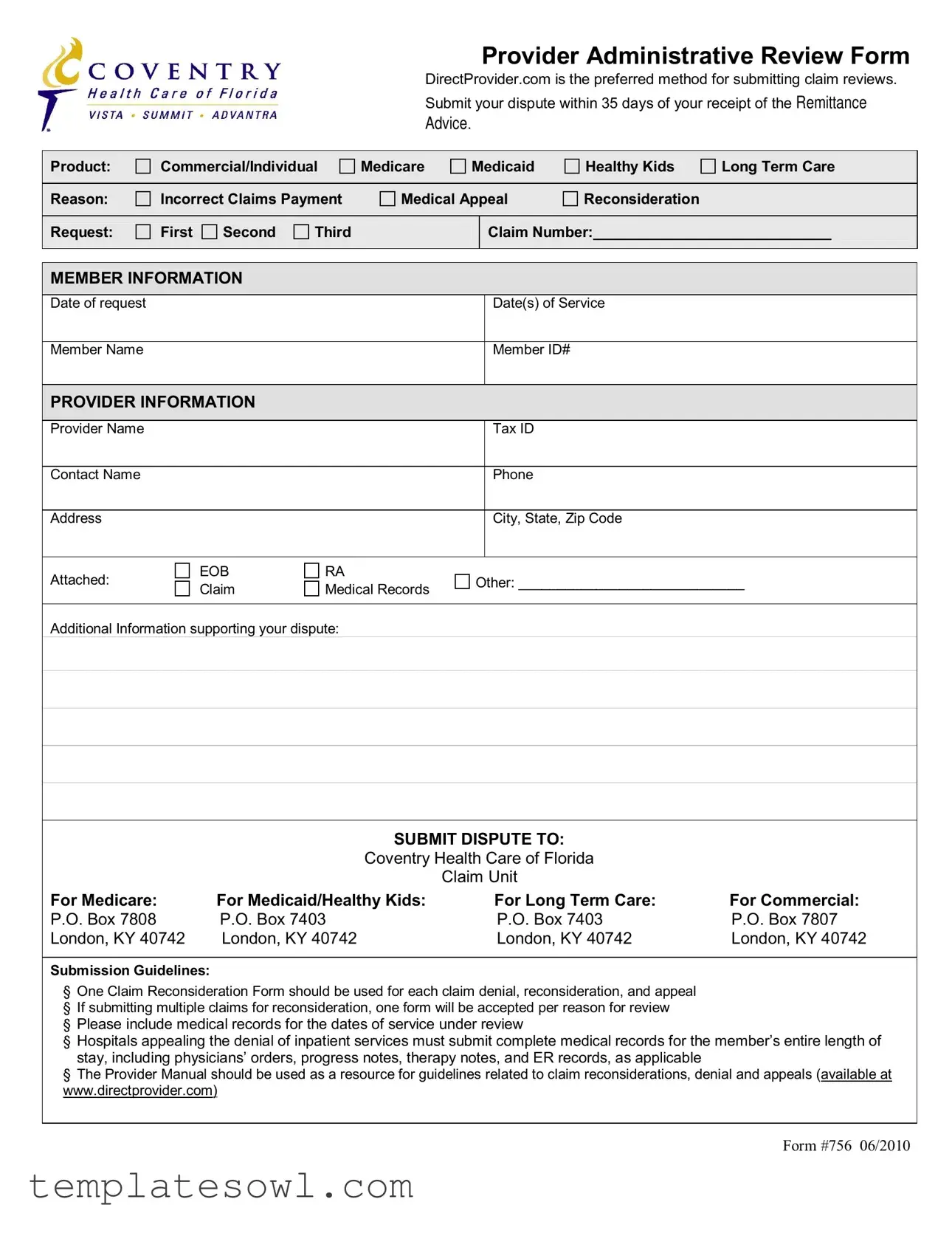
Coventry Claim Example
Provider Administrative Review Form
DirectProvider.com is the preferred method for submitting claim reviews.
Submit your dispute within 35 days of your receipt of the REMITTANCE
ADVICE.
Product: |
Commercial/Individual |
Medicare |
Medicaid |
Healthy Kids |
Long Term Care |
|||
|
|
|
|
|
|
|
|
|
Reason: |
Incorrect Claims Payment |
Medical Appeal |
Reconsideration |
|
||||
|
|
|
|
|
|
|
|
|
Request: |
First |
Second |
Third |
|
|
Claim Number:_____________________________ |
||
|
|
|
|
|
|
|
|
|
MEMBER INFORMATION
Date of request |
Date(s) of Service |
|
|
Member Name |
Member ID# |
|
|
PROVIDER INFORMATION
Provider Name |
|
|
|
Tax ID |
|
|
|
|
|
|
|
Contact Name |
|
|
|
Phone |
|
|
|
|
|
|
|
Address |
|
|
|
City, State, Zip Code |
|
|
|
|
|
|
|
Attached: |
EOB |
RA |
Other: _____________________________ |
||
Claim |
Medical Records |
||||
|
|
|
|||
Additional Information supporting your dispute:
SUBMIT DISPUTE TO:
Coventry Health Care of Florida
Claim Unit
For Medicare: |
For Medicaid/Healthy Kids: |
For Long Term Care: |
For Commercial: |
P.O. Box 7808 |
P.O. Box 7403 |
P.O. Box 7403 |
P.O. Box 7807 |
London, KY 40742 |
London, KY 40742 |
London, KY 40742 |
London, KY 40742 |
Submission Guidelines:
§ One Claim Reconsideration Form should be used for each claim denial, reconsideration, and appeal § If submitting multiple claims for reconsideration, one form will be accepted per reason for review
§ Please include medical records for the dates of service under review
§ Hospitals appealing the denial of inpatient services must submit complete medical records for the member’s entire length of stay, including physicians’ orders, progress notes, therapy notes, and ER records, as applicable
§ The Provider Manual should be used as a resource for guidelines related to claim reconsiderations, denial and appeals (available at www.directprovider.com)
FORM #756 06/2010
Form Characteristics
| Fact Name | Details |
|---|---|
| Submission Method | The preferred method for submitting a Coventry Claim form is through DirectProvider.com. |
| Dispute Period | Providers must submit their disputes within 35 days of receiving the remittance advice. |
| Products Covered | This form caters to claims related to Commercial, Individual Medicare, Medicaid, Healthy Kids, and Long-Term Care. |
| Types of Claim Reasons | Claim reasons may include incorrect claims payment, medical appeal, or reconsideration requests which can be first, second, or third. |
| Required Information | Key member and provider information must be provided, including name, ID, tax ID, contact details, and the claim number. |
| Submission Addresses | Specific P.O. Box addresses are designated for different types of claims: Medicare, Medicaid/Healthy Kids, Long-Term Care, and Commercial. |
| Guidelines for Submission | Only one Claim Reconsideration Form should be submitted per claim denial, and medical records for the disputed dates should accompany the form. |
Guidelines on Utilizing Coventry Claim
Completing the Coventry Claim form is an essential process for addressing disputes related to claim payments. This step-by-step guide will assist you through the necessary information you'll need to provide. Each piece of information is critical in ensuring your claim is reviewed properly and promptly.
- Gather relevant documents including the remittance advice and any additional records needed to support your claim.
- Indicate the product type by selecting one of the options: Commercial, Individual, Medicare, Medicaid, Healthy Kids, or Long Term Care.
- Specify the reason for the dispute, choosing from options like Incorrect Claims Payment, Medical Appeal, or Reconsideration Request.
- Write the claim number in the indicated space.
- Fill out the member information section, including the date of request, the dates of service, the member's name, and the member ID number.
- Complete the provider information section. Include the provider's name, tax ID, contact name, phone number, and address including city, state, and ZIP code.
- List any attached documents in the space provided. Options may include EOB, RA, Claim Medical Records, or other relevant information.
- Submit your dispute to the appropriate Coventry address based on the product type you selected. Use the correct P.O. Box address for Medicare, Medicaid/Healthy Kids, Long Term Care, or Commercial as indicated on the form.
Once you have filled out the form completely, review everything for accuracy. Submitting it promptly will initiate the review process for your dispute. Ensure you adhere to the guidelines regarding submission timelines and necessary documentation. Each detail helps facilitate a thorough examination of your case.
What You Should Know About This Form
What is the Coventry Claim form, and when should it be used?
The Coventry Claim form is utilized to initiate a review of claims disputes in various healthcare programs, including Commercial, Individual Medicare, Medicaid, Healthy Kids, and Long Term Care. Providers should use this form when they believe a claim has been incorrectly paid, or in cases where they wish to appeal a services denial. The form must be submitted within 35 days of receiving the remittance advice.
How do I submit the Coventry Claim form?
The preferred method for submitting the Coventry Claim form is through DirectProvider.com. Providers must ensure that all necessary information, including the claim number, member information, and provider details, is accurately completed. The form should be sent to the appropriate claim unit based on the relevant program, as specified in the instructions.
What documentation is required when submitting the form?
When submitting the Coventry Claim form, it is essential to include the necessary supporting documentation. This includes the Explanation of Benefits (EOB), remittance advice (RA), and any other relevant medical records that support the dispute. For hospitals appealing the denial of inpatient services, complete medical records for the entire length of stay must be included, covering all pertinent orders and notes.
Can I submit more than one claim using the Coventry Claim form?
Each Coventry Claim form should address only one claim denial, reconsideration, or appeal. If multiple claims need reconsideration, it is imperative to submit individual forms for each claim. However, if the claims are part of the same reason for review, they may be submitted together, but each claim must clearly be identified on the form.
Where do I send the Coventry Claim form after it’s completed?
The completed Coventry Claim form must be sent to the specific claim unit designated for the program in question. Each program—Medicare, Medicaid/Healthy Kids, Long Term Care, and Commercial—has its own designated P.O. Box in London, KY. Ensure that the claim form is sent to the correct address based on the type of healthcare service involved.
Common mistakes
Filling out the Coventry Claim form correctly is crucial to a successful claim review. However, many individuals make common mistakes that can delay or even derail their appeals. Here are seven notable errors to avoid.
One major mistake is not submitting the form within the specified timeframe. The instruction states that disputes must be submitted within 35 days of receiving the remittance advice. Missing this deadline can result in automatic denial, leaving people frustrated and without proper recourse.
Another common error involves failing to provide complete member information. Missing details such as the member name, ID number, or the dates of service can lead to significant delays. The claim review process depends on accurate and complete data, so it’s important to double-check this section before submitting.
Many providers forget to include the proper supporting documentation. While it might seem like a minor oversight, attaching relevant medical records and other necessary documents, such as explanation of benefits (EOB) or remittance advice (RA), is essential for a complete review. Claims are often denied simply due to insufficient information.
Using the wrong claim reconsideration form is a frequent mistake as well. It's crucial to understand that one form should be used for each specific issue, whether it’s a denial, reconsideration, or appeal. Submitting multiple claims for different reasons on the same form can complicate the process and lead to confusion concerning what is being requested.
Inadequate explanation of the reason for the dispute can be a stumbling block too. Simply stating “incorrect payment” without detailing why or providing context does not give enough information for the review team. Taking the time to explain the error thoroughly makes a significant difference in the review outcome.
Another error is neglecting to review the instructions for submitting specific types of claims. Different types of services, like Medicare or Medicaid, have unique submission addresses, as noted in the form. Sending a claim to the wrong address can cause unnecessary delays in the processing of your dispute.
Lastly, failing to refer to the Provider Manual for guidelines can lead to missteps. This manual is an invaluable resource for understanding the nuances of claim reconsiderations, denial, and appeals. Ignoring it may result in missing critical instructions that could strengthen a claim’s chances for approval.
Documents used along the form
The Coventry Claim form is a vital document used by healthcare providers to dispute claims and seek reconsiderations. Accompanying it are other documents necessary for a complete submission. Each plays a specific role in the claims process, ensuring that all pertinent information is provided to facilitate a thorough review.
- Provider Administrative Review Form: This form is essential for initiating a review of a claim. It captures details regarding the reason for the dispute and outlines the necessary member and provider information.
- Explanation of Benefits (EOB): This document outlines the payments made by an insurance company, detailing what is covered under the member’s plan. It provides a clear view of how the claim was processed and can support the need for reconsideration.
- Remittance Advice (RA): This is a statement from the insurance company that explains the payments, adjustments, and denials on a claim. It serves as a reference for understanding discrepancies in payments.
- Medical Records: Documentation that provides evidence for the services rendered. It is crucial for substantiating the necessity of the services and addressing any disputes related to denied claims.
- Appeal Letter: A letter outlining the reasons for appealing a claim denial. This document should clearly state the grounds of the appeal and include any supporting evidence that may strengthen the case.
- Member Authorization Form: This form grants permission for the provider to access the member’s health records. It is necessary when submitting any medical records for the appeal or dispute process.
Each of these documents is integral in building a comprehensive case for reconsideration of a denied claim. Ensure all materials are complete and accurate to facilitate a swift review by Coventry Health Care.
Similar forms
- Insurance Claim Form - This document serves a similar purpose by allowing individuals to request payment or reimbursement from their insurance provider for medical expenses incurred. Both forms require detailed information about the member and the services rendered.
- Medical Appeal Form - Like the Coventry Claim form, this document is used to challenge a decision made by an insurance company regarding claims. It requires specific details about the situation and justification for the appeal.
- Healthcare Provider's Appeal Request - This form allows a healthcare provider to appeal for payment on behalf of a patient. Both forms emphasize the need for supporting documentation and clear reasons for reconsideration.
- Patient Authorization Form - Both documents may require patient information and can necessitate a signed authorization to disclose medical records relevant to the claim or appeal being submitted.
- Medicare Reconsideration Form - Similar in function, this document is tailored specifically for Medicare claims. It provides a structured format for disputing claim denials while requiring information about the member and the denied service.
- Medicaid Appeals Form - This is designed to contest Medicaid-related claims. Much like the Coventry Claim form, it asks for extensive details about the claim being appealed and can require various supporting documents.
- Independent Review Organization Request - Parties may use this form when appealing decisions to an independent body. Both documents aim to outline the details surrounding a claim so as to facilitate a review process.
- Insurance Dispute Form - This is used to formally dispute issues with payments or coverage. It parallels the Coventry Claim form by requiring information about the specific claim and reasons for the dispute.
- Claim Denial Letter Template - While not a claim form per se, this document provides a framework for composing letters that accompany disputes. It echoes the organization and detail required by the Coventry Claim form.
- Request for Medical Records Form - This form allows patients or providers to request medical documentation necessary for appealing a claim. It shares a focus on supporting information, similar to the Coventry form.
Dos and Don'ts
When filling out the Coventry Claim form, there are important dos and don'ts to keep in mind to ensure a smooth submission process. Below is a helpful list to guide you.
Things You Should Do:
- Review the claim thoroughly before submission.
- Use DirectProvider.com for submitting your claim reviews, as it is the preferred method.
- Submit your dispute within 35 days of receiving the remittance advice.
- Attach all necessary documents, including medical records, EOBs, and additional supporting information.
- Complete one Claim Reconsideration Form for each claim denial or appeal.
Things You Shouldn't Do:
- Do not use the same claim form for multiple claim denials.
- Avoid incomplete submissions; ensure all fields are filled out accurately.
- Never submit forms without proper supporting documentation.
- Do not forget to check the Provider Manual for guidelines related to your specific situation.
- Refrain from submitting forms by any method other than the specified mailing addresses for each type of coverage.
Misconceptions
Understanding the Coventry Claim form is crucial for successful submissions. However, several misconceptions often lead to confusion. Here are six common misunderstandings and clarifications to help navigate the process:
- Submission must occur immediately. Many believe claims should be submitted instantly after receiving a denial. In reality, there is a 35-day window for submitting disputes after getting the remittance advice, allowing providers time to gather necessary documentation.
- Only one claim can be submitted per form. This is a prevalent myth. In truth, you can submit multiple claims, but each must pertain to different reasons for review. Each reason requires a separate form.
- Medical records are optional. Some providers think they can skip including medical records with their submissions. This is inaccurate; providing relevant medical records is critical, especially for medical appeal requests.
- The Provider Manual is not necessary. There’s a belief that skipping the Provider Manual is fine. However, this manual is a valuable resource, offering essential guidelines for the claims process that can enhance the likelihood of a successful appeal.
- All claims can be combined on a single form. Many assume that combining different claims on one form is acceptable. This is incorrect. Each claim denial requires its own reconsideration form tailored to the specific circumstances.
- Only certain types of claims can be appealed. Some providers mistakenly think that only a subset of claims is eligible for appeal. In fact, claims from various categories, including Medicare, Medicaid, and commercial insurance, can be disputed as long as they meet the designated criteria.
By addressing these misconceptions, providers can better prepare their Coventry Claim submissions and increase their chances of success in obtaining the desired outcomes.
Key takeaways
Filling out and using the Coventry Claim form requires attention to detail. Here are key takeaways to consider:
- Submission Timeline: You must submit your dispute within 35 days of receiving the Remittance Advice.
- Claim Number Required: Ensure to include the correct claim number; this is essential for tracking your dispute.
- Provider Information: Complete all sections related to provider information, including name, Tax ID, and contact details.
- Member Information: Accurately fill out the member's details, including dates of service and member ID.
- One Form per Claim: Use a separate claim reconsideration form for each claim denial, reconsideration, or appeal.
- Supporting Documents: Attach all necessary medical records and any relevant information to support your dispute.
- Submission Address: Double-check the correct address for submitting your dispute based on the product (Medicare, Medicaid, etc.).
- Complete Medical Records: Hospitals must submit comprehensive medical records when appealing inpatient service denials.
- Utilize Resources: Refer to the Provider Manual available at DirectProvider.com for additional guidelines and resources.
Following these steps carefully can facilitate a smoother claims process and improve your chances of a successful appeal.
Browse Other Templates
How Long Do Credits Last for College - Complete the form thoughtfully to avoid unnecessary complications.
Test Report for RPZ Device,RPZ Valve Certification Form,Backflow Prevention Test Summary,RPZ Device Evaluation Certificate,Water Supplier RPZ Test Document,RPZ Device Compliance Report,RPZ Valve Inspection Record,Test Certificate for RPZ Assembly,RPZ - Test report for RPZ valve compliance.