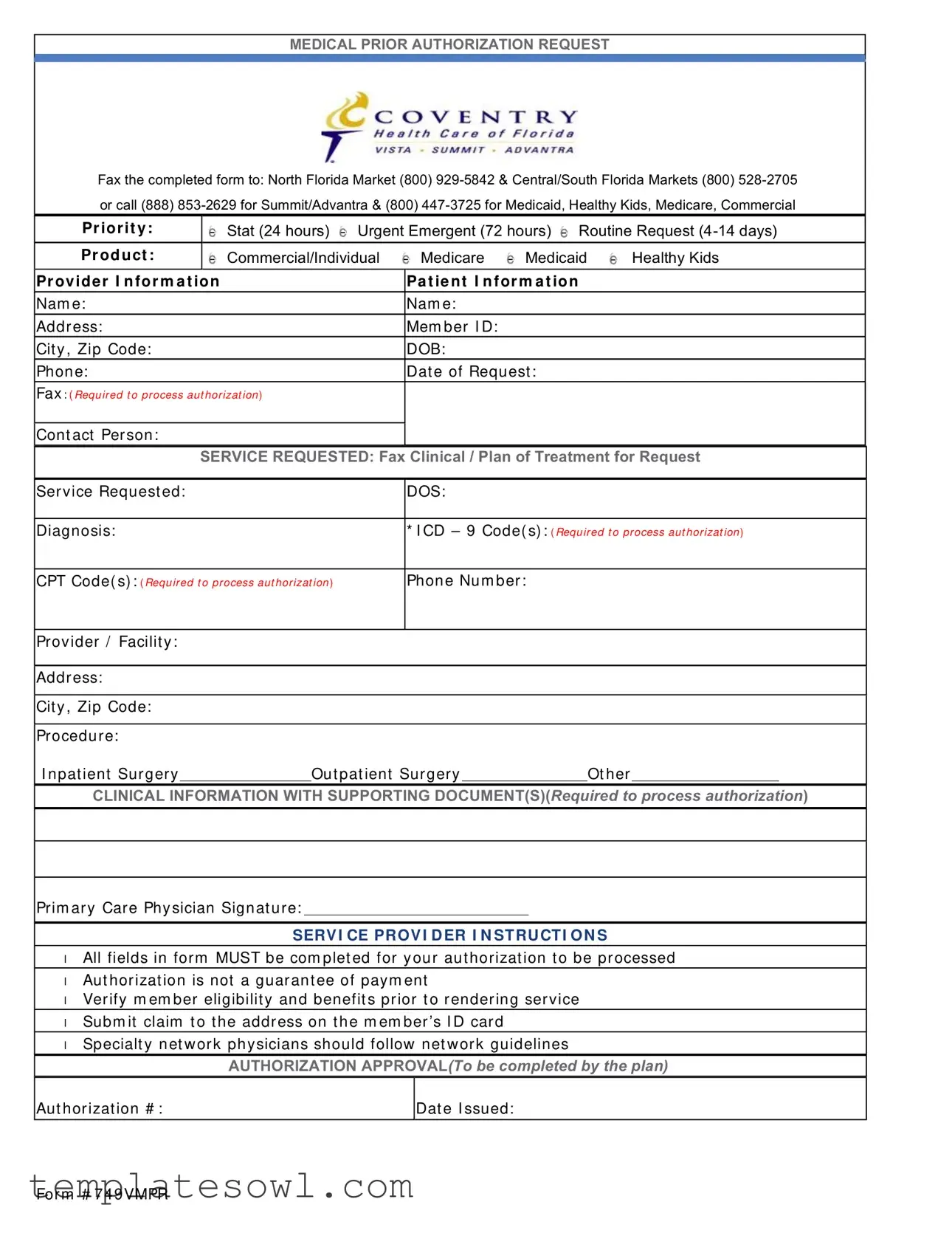
Fill Out Your Coventry Prior Authorization Form
The Coventry Prior Authorization form is an essential document designed to streamline the medical authorization process across various markets in Florida. This form facilitates the approval of requested medical services by requiring detailed patient and provider information. Among the critical components are patient identifiers, including name, date of birth, and member ID numbers, alongside specifics about the service being requested, such as the diagnosis and procedure details. The form also necessitates clinical documentation to support the request, ensuring that all required information is submitted to process the authorization effectively. Urgency levels can vary, with options for stat (24 hours), urgent emergent (72 hours), and routine requests (ranging from 4 to 14 days). Providers must complete all sections of the form to avoid delays, as incomplete submissions can hinder the authorization determination. It is crucial to note that obtaining authorization does not guarantee payment, compelling providers to verify member eligibility and benefits before delivering the requested services. Finally, once the request is processed, a unique authorization number will be issued by the plan, marking the beginning of the coverage process for the necessary medical service.
Coventry Prior Authorization Example
MEDICAL PRIOR AUTHORIZATION REQUEST
Fax the completed form to: North Florida Market (800)
Pr io r i t y : |
cef |
Stat (24 hours) cef Urgent Emergent (72 hours) cef Routine Request |
|||
Pr od u ct : |
cef |
Commercial/Individual |
fec Medicare cef Medicaid |
cef Healthy Kids |
|
Pr ov i d e r I n f o r m a t io n |
|
Pa t ie n t I n f or m a t io n |
|
||
Nam e: |
|
|
Nam e: |
|
|
Addr ess: |
|
|
Mem ber I D: |
|
|
Cit y , Zip Code: |
|
|
DOB: |
|
|
Phon e: |
|
|
Dat e of Request : |
|
|
Fax : ( Requ ir ed t o pr ocess aut hor izat ion ) |
|
|
|
||
Cont act Per son : |
|
|
|
|
|
|
SERVICE REQUESTED: Fax Clinical / Plan of Treatment for Request |
||||
Ser vice Request ed: |
|
|
DOS: |
|
|
Diagnosis: |
|
|
* I CD – 9 Code( s) : ( Requ ir ed t o pr ocess aut hor izat ion ) |
||
CPT Code( s) : ( Requ ir ed t o pr ocess aut hor izat ion ) |
Phon e Nu m ber : |
|
|||
Provider / Facilit y : |
|
|
|
|
|
Addr ess: |
|
|
|
|
|
Cit y , Zip Code: |
|
|
|
|
|
Procedu re: |
|
|
|
|
|
I npat ient Sur gery |
|
Ou t pat ient Sur gery |
|
Ot her |
|
CLINICAL INFORMATION WITH SUPPORTING DOCUMENT(S)(Required to process authorization)
Prim ar y Care Phy sician Sign at u re:
|
|
SERV I CE PR OV I D ER I N ST RU CT I O N S |
l |
All fields in form MUST be com plet ed f or y ou r au t horizat ion t o be pr ocessed |
|
l |
Aut hor izat ion is not a guar an t ee of paym ent |
|
l |
Ver if y m em ber eligibilit y an d benef it s pr ior t o r ender in g ser vice |
|
l |
Subm it claim t o t he addr ess on t h e m em ber ’s I D car d |
|
l |
Specialt y n et w or k ph ysicians should f ollow net w or k guidelines |
|
|
|
AUTHORIZATION APPROVAL(To be completed by the plan) |
Aut hor izat ion # : |
Dat e I ssued: |
|
For m # 74 9VMPR
Form Characteristics
| Fact Name | Description |
|---|---|
| Submission Process | Fax the completed form to North Florida Market at (800) 929-5842 or Central/South Florida Markets at (800) 528-2705. You can also call for assistance. |
| Urgency Levels | The form accommodates three levels of urgency: Priority (24 hours), Urgent/Emergent (72 hours), and Routine Request (4-14 days). |
| Required Information | Completing all fields related to patient and provider information, diagnosis, and supporting documents is essential for processing authorization. |
| Authorization Disclaimer | Obtaining authorization does not guarantee payment. Members must verify eligibility and benefits before services are rendered. |
Guidelines on Utilizing Coventry Prior Authorization
After completing the Coventry Prior Authorization form, the next step involves submitting it to the appropriate fax number based on the market. Ensure that all sections are filled out accurately to avoid any delays in processing. This form requires outlining patient information, provider details, and the specific service requested. Once the form is properly filled out, it can be faxed to the corresponding number indicated on the form.
- Begin by filling out the Provider Information section. Include the provider's name, address, city, zip code, phone number, and fax details.
- Complete the Patient Information section. Fill in the patient's name, address, member ID, date of birth, phone number, and the date of request.
- Identify the Priority of the request. Choose from urgent, emergent, or routine, based on the situation.
- Select the Product type applicable to the patient: Commercial/Individual, Medicare, Medicaid, or Healthy Kids.
- Specify the Service Requested. Indicate the type of service, date of service (DOS), diagnosis, ICD-9 code(s), and CPT code(s).
- Attach any Clinical Information and supporting documents required to process authorization.
- Ensure the Primary Care Physician Signature field is signed by the appropriate doctor.
- Double-check that all fields are completed as required for authorization processing.
- Fax the completed form to the appropriate number for North Florida or Central/South Florida Markets.
What You Should Know About This Form
What is the purpose of the Coventry Prior Authorization form?
The Coventry Prior Authorization form is used to request approval for medical services before they are provided. This process helps ensure that the requested treatments are medically necessary and align with the patient’s insurance benefits. It is essential for securing the necessary funding for prescribed services, especially for surgeries or specialized treatments. Completing this form correctly ensures that the patient receives timely care without unexpected costs.
How should I submit the Coventry Prior Authorization form?
Once you have completed the Coventry Prior Authorization form, you can submit it via fax. For the North Florida Market, use the fax number (800) 929-5842. For the Central and South Florida Markets, use (800) 528-2705. If you prefer to reach out for assistance or have any questions, you can call (888) 853-2629 for Summit/Advantra services or (800) 447-3725 for Medicaid, Healthy Kids, and Medicare inquiries.
What information do I need to provide on the form?
Filling out the form requires specific details about both the provider and the patient. Key items include the patient’s name, date of birth, and member ID, as well as the provider’s contact information. Additionally, it's critical to specify the services requested, including the date of service, diagnosis, and applicable CPT and ICD-9 codes. All fields must be completed for the authorization request to be processed effectively.
What happens after I submit the form?
Once the form is submitted, it undergoes a review process. You will receive an authorization number if the request is approved. However, it’s important to remember that authorization does not guarantee payment. Patients should verify their eligibility and benefits prior to receiving any services. Additionally, those using specialty network physicians should adhere to the specific network guidelines to ensure coverage.
Common mistakes
Filling out the Coventry Prior Authorization form can be straightforward, but many people make common mistakes that can delay the process. One frequent error is not completing all fields. Every section of the form must be filled out to ensure the request can be processed smoothly. If any crucial information is missing, it could lead to rejection or additional delays.
Another mistake is failing to provide supporting documentation. Clinical information, including relevant treatment plans or medical records, is essential. Without this, the authorization request might not be evaluated appropriately, resulting in a denied request.
Some individuals neglect to double-check member eligibility before submitting the form. Ensuring that the patient is eligible for coverage helps prevent unnecessary complications later on. Verifying eligibility beforehand saves everyone time, as it can help avoid processing issues down the road.
Incorrect diagnosis codes are also a common pitfall. When filling out the ICD-9 codes, it is crucial to use the right ones. An error here can lead to miscommunication about the patient's condition, affecting the approval of the request.
The use of wrong CPT codes can cause the same issues. These codes indicate the specific services requested and must accurately reflect the treatment being planned. An incorrect code not only complicates the authorization process but may also lead to billing problems later.
Omitting the provider’s signature is yet another frequent oversight. The primary care physician’s approval is necessary for the process to begin. Without this, the form may be returned or rejected entirely.
People often forget to include contact information for follow-up purposes. Providing a phone number allows the authorization department to reach out quickly with any questions or additional information needed. Including this can greatly improve communication.
Lastly, many people do not adhere to the submission guidelines. Each section of the form has specific requirements, including where to fax the form based on the market. How the form is submitted can impact the speed and success of the authorization process.
Documents used along the form
The Coventry Prior Authorization form is an essential document for requesting approval for medical services. It helps ensure that patients receive the necessary care in a timely manner, while also aligning with insurer requirements. Alongside this form, several other documents are commonly used to support the authorization process. Below is a list of these accompanying forms and documents.
- Clinical Notes: These notes provide detailed information about the patient's medical history, the rationale for treatment, and ongoing health status. They are critical for healthcare providers to justify the necessity of the requested service.
- Plan of Treatment: This document outlines the proposed treatment protocol for the patient. It includes the goals of the treatment, the specific procedures planned, and any anticipated outcomes, helping insurers understand the necessity of the care requested.
- Eligibility Verification: Prior to submitting a prior authorization request, confirming that the patient is eligible for coverage is crucial. This document demonstrates that the patient meets the insurer's criteria for the requested services.
- Diagnostic Imaging Reports: These reports, such as X-rays or MRIs, provide concrete evidence of the medical condition being treated. They can help substantiate the request for particular services by showing the severity and necessity of intervention.
- Current Medication List: A comprehensive list of medications the patient is currently taking assists in assessing the full scope of treatment required. It also helps ensure that the requested services do not conflict with ongoing therapies.
- Informed Consent Form: This document confirms that the patient is aware of the risks, benefits, and alternatives to the proposed treatment. It signifies that the healthcare provider has communicated relevant information to the patient, which can support the necessity of the service requested.
When submitting the Coventry Prior Authorization form, including these additional documents can enhance the likelihood of a timely approval. They provide a comprehensive view of the patient’s situation, ensuring that all necessary information is readily available for review.
Similar forms
The Coventry Prior Authorization form is similar to several other documents used for medical service requests and insurance approvals. Here are six documents that share similar features and purposes:
- Medicare Prior Authorization Request Form: This form requires detailed information about the patient's medical history and the requested services. It also specifies the urgency of the request, including standard and expedited services.
- Medicaid Authorization Request Form: Like the Coventry form, this document captures patient data, provider details, and service requests. Both forms necessitate clinical information and supporting documents for review.
- Commercial Insurance Prior Authorization Form: This document serves a similar purpose, requiring the completion of patient and provider information. It also asks for service details and any necessary coding for processing.
- Home Health Services Prior Authorization Form: Similar to the Coventry form, this document requests information related to home health services. It requires patient eligibility verification and specific details about the services to be provided.
- Durable Medical Equipment (DME) Authorization Request Form: This form is used to obtain authorization for DME services. It requires thorough patient data and justification for the necessity of the requested equipment, paralleling the information requested in the Coventry form.
- Inpatient Admission Authorization Form: This document is required for planned inpatient services. It includes detailed patient information, the reason for admission, and the expected length of stay, similar to the Coventry Prior Authorization process.
Dos and Don'ts
When filling out the Coventry Prior Authorization form, consider the following important dos and don’ts:
- Do complete all fields in the form thoroughly.
- Do provide accurate patient and provider information.
- Do fax the completed form to the correct numbers.
- Do verify member eligibility and benefits before providing services.
- Do include clinical information and supporting documents.
- Don't assume authorization guarantees payment.
- Don't forget to include diagnosis and procedure codes.
- Don't use incorrect phone numbers for submission or inquiries.
- Don't skip the signature line for the primary care physician.
- Don't forget to check the appropriate priority for the request.
Misconceptions
Understanding the Coventry Prior Authorization form is essential for healthcare providers and patients alike. However, several misconceptions often arise. Here are ten common myths and the truths behind them.
-
Myth: Filling out the form is optional.
This is incorrect. Completing the Coventry Prior Authorization form is mandatory for services requiring prior approval.
-
Myth: Authorization guarantees payment.
Authorization does not guarantee payment. It only confirms that the service is medically necessary.
-
Myth: The form can be submitted without complete information.
All fields must be fully completed; missing information can lead to delays or denial of requests.
-
Myth: Any healthcare provider can submit the form.
Only authorized healthcare providers can submit this form, and they must verify the patient's eligibility.
-
Myth: Prior authorization is the same for all services.
Different services may have distinct requirements and processing times. Understanding specific needs is crucial.
-
Myth: The form does not require supporting documents.
Supporting documents are necessary for processing the authorization. Clinical information must be included.
-
Myth: You can call to expedite the authorization process.
While you can inquire about the status, calling does not speed up the review process. All requests are handled in the order they are received.
-
Myth: There are no deadlines for submitting the form.
Timeliness matters. Certain services must be requested well in advance to ensure coverage.
-
Myth: Authorization is only necessary for inpatient procedures.
Prior authorization may be required for both inpatient and outpatient services, depending on the situation or plan specifics.
-
Myth: Medicaid and Medicare processes are identical to commercial requests.
Each program has different rules and processes. Always check the specific guidelines for each insurance plan.
Key takeaways
Filling out the Coventry Prior Authorization form is an essential procedure for healthcare providers seeking approval for specific medical services. Understanding how to navigate this process is crucial. Here are key takeaways:
- Complete All Fields: Ensure that every section of the form is filled out accurately. Missing information can delay the authorization process.
- Types of Requests: Be aware of the three different priority levels: Stat (24 hours), Urgent Emergent (72 hours), and Routine (4-14 days). Choose the appropriate option based on the urgency of the request.
- Fax Numbers: The completed form should be faxed to either the North Florida Market at (800) 929-5842 or the Central/South Florida Markets at (800) 528-2705.
- Contact Information: Include your phone number and a contact person. This ensures that you can be reached for any clarifications required during processing.
- Member Information: Provide accurate member details, including Member ID and date of birth, as these are critical for processing authorization.
- Clinical Information: Attach the necessary clinical documentation. This information supports the medical necessity of the requested service.
- Diagnosis Codes: Include the appropriate ICD-9 codes and CPT codes for the procedure being requested. These codes are mandatory for authorization.
- Provider’s Signature: Don’t forget to obtain the primary care physician’s signature, as it validates the request.
- Authorization is Not Guaranteed: It is important to understand that obtaining prior authorization does not guarantee payment for services rendered. Verify member eligibility before proceeding with treatment.
- Claim Submission: After authorization has been received, submit the claim to the address listed on the member’s ID card to ensure proper processing.
Following these takeaways can help streamline the authorization process, ultimately aiding in the efficient delivery of patient care.
Browse Other Templates
Va Form 21-4192 Example - Veterans can grant permission for specific medical information to be disclosed through this form.
Hesser College Transcripts - Transcripts reflect your academic history at Mount Washington College.
Tdi Class 4 Form - The certification details play a significant role in risk assessments by insurers.