Fill Out Your Cvs Prior Auth Form
The CVS Prior Authorization Form serves a crucial function in the healthcare process, particularly for those seeking specific medications that may require special approval from insurance providers. This form initiates the request for a Drug Specific Prior Authorization, a necessary step before a treatment can proceed. To start the process, individuals need to fill out essential information about the patient, such as their full name, date of birth, contact details, and cardholder identification number. It is equally important to provide detailed information about the medication in question, including its name and strength. Additionally, a prescriber’s information must be included, emphasizing the healthcare professional's role in providing the necessary context for the request. Accuracy is paramount when completing this form; missing or unclear details can lead to delays in the authorization process. After the initial form is submitted via fax, Caremark will respond with a Drug Specific Prior Authorization Request Form and relevant questions that need to be addressed. Following submission of this form, Caremark will examine the request and communicate the approval or denial of the authorization, along with the reasons if the request is denied. Protecting patient privacy is a top priority, and all staff handle health information with strict confidentiality. Understanding the implications and requirements of the CVS Prior Authorization Form can streamline medication access for patients who depend on timely and effective treatments.
Cvs Prior Auth Example
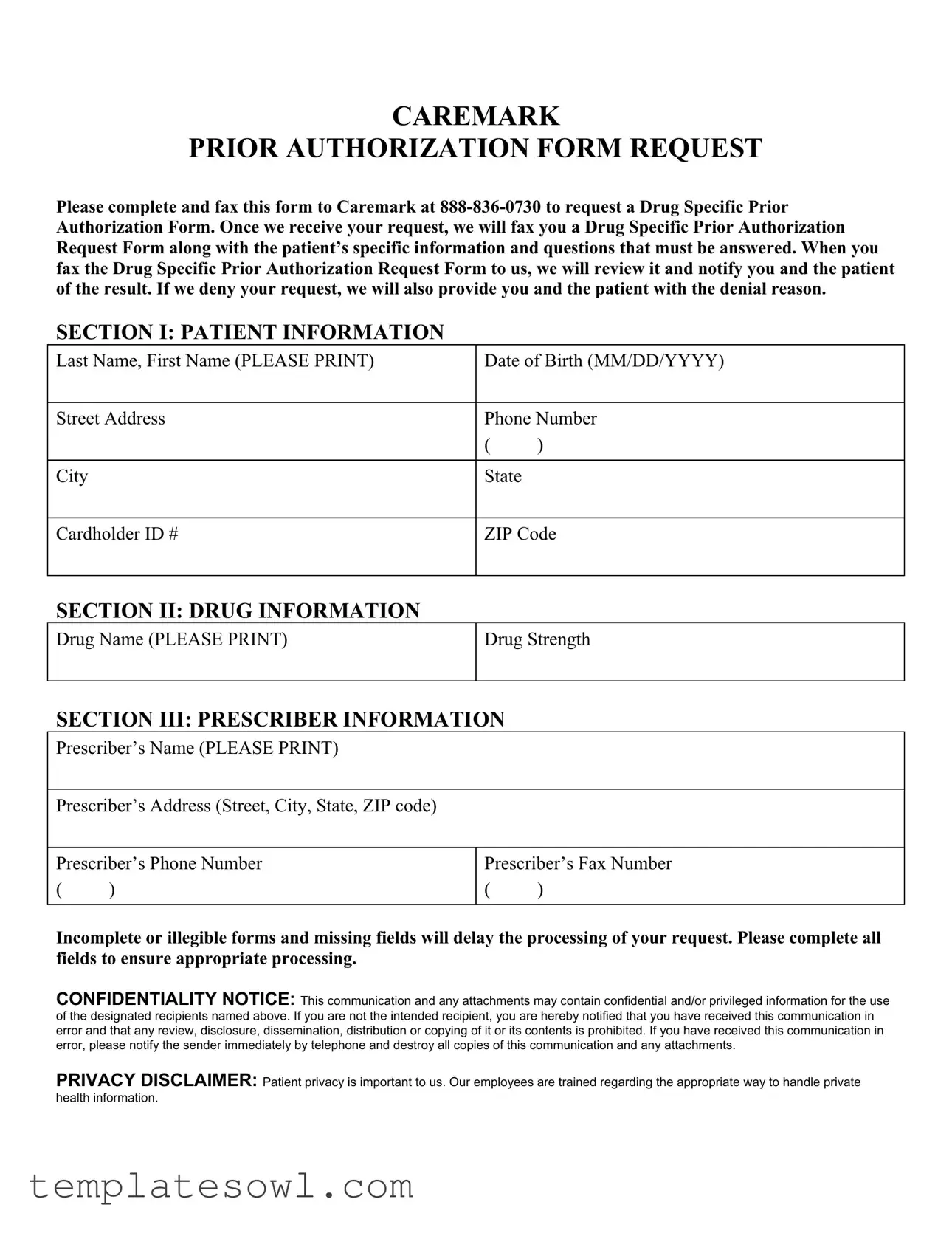
CAREMARK
PRIOR AUTHORIZATION FORM REQUEST
Please complete and fax this form to Caremark at
SECTION I: PATIENT INFORMATION
Last Name, First Name (PLEASE PRINT) |
Date of Birth (MM/DD/YYYY) |
|
|
|
|
Street Address |
Phone Number |
|
|
( |
) |
|
|
|
City |
State |
|
|
|
|
Cardholder ID # |
ZIP Code |
|
|
|
|
SECTION II: DRUG INFORMATION
Drug Name (PLEASE PRINT)
Drug Strength
SECTION III: PRESCRIBER INFORMATION
Prescriber’s Name (PLEASE PRINT)
Prescriber’s Address (Street, City, State, ZIP code)
Prescriber’s Phone Number
()
Prescriber’s Fax Number
()
Incomplete or illegible forms and missing fields will delay the processing of your request. Please complete all fields to ensure appropriate processing.
This communication and any attachments may contain confidential and/or privileged information for the use of the designated recipients named above. If you are not the intended recipient, you are hereby notified that you have received this communication in error and that any review, disclosure, dissemination, distribution or copying of it or its contents is prohibited. If you have received this communication in error, please notify the sender immediately by telephone and destroy all copies of this communication and any attachments.
PRIVACY DISCLAIMER: Patient privacy is important to us. Our employees are trained regarding the appropriate way to handle private health information.
Form Characteristics
| Fact Name | Fact Details |
|---|---|
| Confidentiality Notice | The form includes a confidentiality notice, emphasizing that it contains privileged information meant only for designated recipients. |
| Submission Method | This form must be completed and faxed to Caremark at 888-836-0730 to initiate a Drug Specific Prior Authorization request. |
| Request Processing | After Caremark receives the submitted request, they will fax back a Drug Specific Prior Authorization Request Form with specific patient information. |
| Notification | Patients will be notified of the authorization result after Caremark reviews the Drug Specific Prior Authorization Request Form. |
| Denial Communication | If a request is denied, the patient and prescriber will receive communication detailing the denial reason. |
| Patient Information Section | The form requires detailed patient information, including last name, first name, DOB, address, phone number, and cardholder ID. |
| Prescriber Information Section | Completing the prescriber's information section is vital, including their name, address, phone number, and fax number. |
| Error Notification | In case of an error, the form instructs unintentional recipients to notify the sender immediately and destroy copies of the communication. |
Guidelines on Utilizing Cvs Prior Auth
Submitting the CVS Prior Authorization form is a crucial step in ensuring that the necessary medication is covered under a patient's insurance. It’s essential to fill out the form accurately to prevent any delays in approval. Once the request is properly submitted, you will receive a Drug Specific Prior Authorization Request Form tailored to the patient's situation. Follow these steps closely to complete the form correctly.
- Prepare the Form: Make sure you have the CVS Prior Authorization form handy. This form should be clear and may need to be printed for completion.
- Patient Information: In SECTION I, provide the patient's last name and first name. Also, include their date of birth in the specified format (MM/DD/YYYY), their street address, city, state, ZIP code, phone number, and the cardholder ID number.
- Drug Information: Moving to SECTION II, write the name of the drug in clear print and specify the drug strength.
- Prescriber Information: In SECTION III, enter the prescriber’s name and their complete address (street, city, state, ZIP code). Include the prescriber’s phone and fax numbers.
- Review the Information: Ensure all fields are filled out completely to avoid processing delays. Check for clarity and legibility.
- Submit the Form: Fax the completed form to Caremark at 888-836-0730. Make sure to send it as soon as possible to expedite the process.
After submitting the form, you will receive a Drug Specific Prior Authorization Request Form that includes more specific questions about the patient's situation. Pay close attention to any follow-up requirements, as this will significantly impact the outcome of the authorization process.
What You Should Know About This Form
What is the purpose of the CVS Prior Authorization Form?
The CVS Prior Authorization Form is designed to facilitate the approval process for certain medications. Healthcare providers must complete this form to request authorization from Caremark for specific drug treatments. This is necessary to ensure that the medication aligns with the patient's health plan and medical necessity guidelines.
How do I submit the CVS Prior Authorization Form?
To submit the CVS Prior Authorization Form, please ensure that all sections are completed accurately. Once filled out, fax the form to Caremark at 888-836-0730. After the initial submission, you will receive a Drug Specific Prior Authorization Request Form tailored to the patient’s information, which must be completed and returned for further processing.
What happens after I submit the form?
Once you submit the form, Caremark will review the provided information. You and the patient will be notified of the authorization decision. If the request is denied, Caremark will provide reasons for the denial. Timely communication can help in understanding any further steps needed.
What information is required to complete the form?
The form requires thorough information about the patient, drug details, and the prescribing physician. Key fields include the patient's name, date of birth, street address, and drug specifics. Incomplete or illegible entries could lead to delays, so it is vital to double-check all details before submission.
What should I do if I receive the form in error?
If you have received the CVS Prior Authorization Form by mistake, please notify the sender immediately by telephone and destroy any copies of the communication. This is essential to maintain the confidentiality and privacy of the information contained within the document.
How does CVS ensure patient privacy during this process?
CVS prioritizes patient privacy and has measures in place to protect private health information. Employees are trained to handle such sensitive data appropriately. By filling out this form, it is assumed that necessary safeguards around confidentiality are upheld throughout the authorization process.
Common mistakes
When filling out the CVS Prior Authorization form, several common mistakes can lead to delays or denials of requests. One significant error occurs in the **patient information section**. Providing incomplete or inaccurate details, such as an incorrect date of birth or misspelled names, can hinder the processing of the request. This section needs to be filled out clearly, with no room for ambiguity, as each piece of information is essential for identifying the patient.
Another mistake often seen involves the **drug information section**. People frequently overlook entering the correct drug name or strength. Using abbreviations or informal names can cause confusion and may result in the request being delayed. It’s crucial to fill out this section carefully, ensuring that the name is printed clearly and that the strength matches what was prescribed.
In the **prescriber information section**, mistakes can also arise. A common error is failing to provide complete contact details for the prescriber. Omitting the prescriber’s phone number or fax number can be especially problematic, as these contacts are vital for follow-up communication. Ensuring that this information is complete and accurate will facilitate easier communication and potentially faster authorization.
Furthermore, individuals sometimes neglect to check the **overall completeness of the form** before submitting it. Forms that arrive with missing fields or entries left blank are often returned. To prevent delays, taking a moment to review the entire form before sending it can save time and hassle down the line.
Confidentiality is another area where mistakes are made. Some people fail to understand the importance of ensuring that all sensitive patient information remains private. It’s essential to be aware of what information is shared and to handle the form accordingly. Not following the privacy guidelines can lead to breaches that are both unethical and potentially harmful.
Lastly, not following the **faxing instructions** accurately can lead to complications. People sometimes fax the form to an incorrect number or do not confirm that the fax was sent and received. This step is critical, as ensuring the form reaches the appropriate place promptly can significantly affect processing times. Taking care with each of these components can lead to a smoother authorization process and a better experience overall.
Documents used along the form
When navigating the prior authorization process, several forms and documents are commonly used alongside the CVS Prior Authorization form. Each of these documents plays a role in ensuring that the authorization process runs smoothly and complies with legal requirements.
- Drug-Specific Prior Authorization Request Form: This form is sent from Caremark after the initial request. It includes detailed questions that must be answered to thoroughly assess the authorization for the specific medication.
- Letter of Medical Necessity: A document from the healthcare provider that outlines why a certain treatment is necessary for the patient. This supports the request for prior authorization by detailing the patient's medical condition and recommended treatment plan.
- Patient Consent Form: A form that patients complete to authorize their healthcare provider or pharmacy to disclose necessary information to obtain prior authorization. This ensures compliance with privacy regulations.
- Prescription Information Form: This document contains specific details about the medication prescribed, including dosages and frequency, which may be required by the insurer during the review process.
- Medical Records: Relevant medical records may be required to support the prior authorization request. These documents verify the patient's medical history and support the need for the requested medication.
- Clinical Evidence Document: This supports the medical necessity of the treatment being requested. It often includes studies or guidelines that justify using a specific drug rather than alternatives.
- Denial Appeal Form: If a prior authorization request is denied, this form allows the provider to formally appeal the decision. It includes space for additional evidence or arguments to support the case for approving the authorization.
Understanding these documents can greatly improve the efficiency of the prior authorization process and enhance your chances of obtaining approval for necessary treatments. Always ensure that all forms are filled out completely and accurately to avoid delays.
Similar forms
- Insurance Prior Authorization Form: Like the Cvs Prior Auth form, this document is also used to obtain pre-approval from insurance companies for specific medical services or medications. It requires patient and provider information, similar to the Cvs form.
- Medication Request Form: This form is often completed by healthcare providers to request medication for patients. It includes details about the patient and the medication, reflecting the structure found in the Cvs form.
- Patient Information Form: When new patients visit a healthcare provider, they often fill out this document. It captures necessary personal and medical information, just as the Cvs form does in its Patient Information section.
- Authorization for Release of Information: This document allows healthcare providers to share patient information with insurance companies. It shares a similar purpose to the Cvs form in obtaining necessary approval for treatment.
- Claim Submission Form: Used to submit claims to insurance companies, this form typically requires similar patient and provider information, paralleling the details collected in the Cvs Prior Auth form.
- Referral Request Form: This form is utilized when a primary care provider refers a patient to a specialist. Just like the Cvs form, it includes specifics about the patient and the requested service.
- Prescription Drug Prior Authorization Request: Specifically focused on medication, this document seeks approval before a medication is prescribed, much like the Cvs Prior Auth form's intent.
- Diagnostic Test Authorization Form: To order certain diagnostic tests, healthcare providers often complete this form to gain necessary approvals. It demands pertinent patient and test details, akin to the information requested in the Cvs form.
- Appeal for Denied Services Form: If a service is denied by an insurance company, healthcare providers may use this form to appeal the decision. Similar to the Cvs form’s process, it outlines necessary information to support the request.
Dos and Don'ts
When filling out the CVS Prior Authorization form, there are essential actions and pitfalls to avoid to ensure a smooth process. Here’s what to do and what not to do:
- Do: Print all patient and prescriber information clearly to avoid misunderstandings.
- Do: Double-check all fields for completeness before submitting the form.
- Do: Include the correct Drug Name and Drug Strength as specified.
- Do: Fax the completed form to the correct number, 888-836-0730.
- Do: Maintain confidentiality and avoid discussing patient information unnecessarily.
- Do: Follow up if you do not receive acknowledgment after a few days.
- Don’t: Submit an incomplete form, as this will delay processing.
- Don’t: Use small or illegible handwriting that could lead to errors.
- Don’t: Ignore the confidentiality notice; it’s crucial to keep patient information secure.
- Don’t: Forget to provide both the prescriber’s phone and fax numbers.
- Don’t: Delay in submitting the form if all information is readily available.
- Don’t: Share the form with unauthorized individuals or entities.
Misconceptions
There are many misconceptions surrounding the CVS Prior Authorization form. Clarifying these misunderstandings can help ensure successful submissions and timely approvals. Below is a list of ten common misconceptions:
- All prescriptions require a prior authorization. Contrary to popular belief, not every medication needs prior approval. Some drugs are exempt based on insurance coverage.
- The form can be filled out incorrectly without consequences. Incomplete or illegible forms can delay processing. It is crucial to provide accurate information.
- Submitting the form guarantees approval. It's important to note that submitting the form does not guarantee that the request will be approved. Each case undergoes a review process.
- Only the prescriber can submit the prior authorization request. While it is often the prescriber’s responsibility, in some cases, patients or their representatives may also initiate the process.
- The denial reasons are not disclosed. If a request is denied, patients and prescribers will receive an explanation of why the approval was not granted.
- Once submitted, no follow-up is necessary. It is advisable to follow up with CVS or the insurance provider to ensure that the request has been processed.
- The prior authorization form is the same across different insurance plans. Each plan may have its specific requirements and forms, making it vital to check with the respective insurance company.
- Patient privacy is not protected during the process. CVS prioritizes patient privacy. Staff members are trained to handle private health information responsibly.
- All information is processed the same day. Processing times can vary. Completing the form correctly may expedite this, but same-day processing is not guaranteed.
- A faxed form is less reliable than electronic submissions. Faxing the form is a standard and secure method for submission. Care should be taken to confirm successful transmission.
Addressing these misconceptions can lead to smoother interactions with CVS and improve the experiences of those navigating the prior authorization process.
Key takeaways
Here are some key takeaways for filling out and using the CVS Prior Auth form:
- Ensure to complete all fields on the form to avoid delays in processing.
- Fax the completed form to Caremark at 888-836-0730 to initiate the request.
- Once the request is submitted, wait for the Drug Specific Prior Authorization Request Form to be sent back to you.
- Provide accurate patient details, including their name, date of birth, and contact information.
- Include both the prescriber’s information and drug details to facilitate a smooth review process.
- If your request is denied, you will be informed of the reason behind the decision.
- Remember, this form contains confidential information; handle it with care to protect patient privacy.
Browse Other Templates
How Much Is a $100 Savings Bond Worth After 30 Years? - Authority to file a claim can be claimed by an individual or a legal representative.
Construction Authorization Form,Building Approval Application,Permit Request Document,Development Permit Form,Construction Permit Application,Site Work Authorization Form,Permit Application for Building,Structural Permit Form,Project Approval Request - Perjury for false statements in the application is a serious offense.
Sc 107 - Witnesses are entitled to fees for their time and travel, which can be requested upfront.