Fill Out Your Dap Note Sample Form
The DAP Note Sample form serves as a structured guide for therapists and mental health professionals to effectively document client interactions and therapeutic progress. It consists of three main components: "D" for Data, "A" for Assessment, and "P" for Plan. The Data section requires both subjective and objective observations about the client, capturing their feelings, behaviors, and progress related to specific issues. Objective data includes direct observations made by the therapist, offering a clear picture of the client's situation. The Assessment section focuses on the professional's interpretation of the data, integrating observations into working hypotheses about the client's mental state, such as the improvement or persistence of symptoms like depression. Finally, the Plan outlines actionable steps for future sessions, including scheduling and any homework assignments given to the clients. This comprehensive format not only enhances the clarity and usefulness of case notes but also aids in ensuring continuity of care for clients by providing essential information for other professionals involved in their treatment.
Dap Note Sample Example
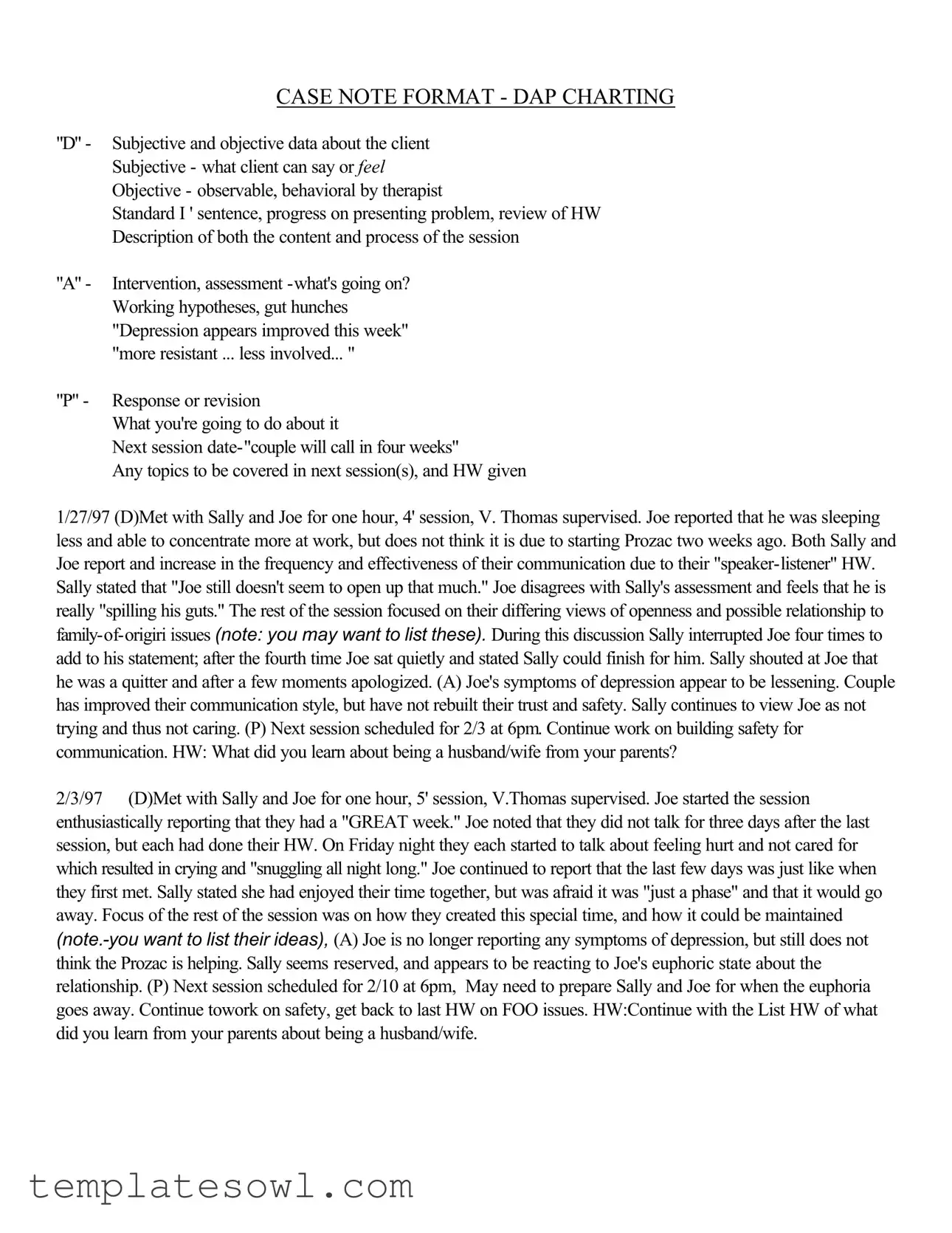
CASE NOTE FORMAT - DAP CHARTING
"D" - Subjective and objective data about the client Subjective - what client can say or FEEL Objective - observable, behavioral by therapist
Standard I ' sentence, progress on presenting problem, review of HW Description of both the content and process of the session
"A" - Intervention, assessment
"P" - Response or revision
What you're going to do about it
Next session
Any topics to be covered in next session(s), and HW given
1/27/97 (D)Met with Sally and Joe for one hour, 4' session, V. Thomas supervised. Joe reported that he was sleeping less and able to concentrate more at work, but does not think it is due to starting Prozac two weeks ago. Both Sally and Joe report and increase in the frequency and effectiveness of their communication due to their
2/3/97 (D)Met with Sally and Joe for one hour, 5' session, V.Thomas supervised. Joe started the session enthusiastically reporting that they had a "GREAT week." Joe noted that they did not talk for three days after the last session, but each had done their HW. On Friday night they each started to talk about feeling hurt and not cared for which resulted in crying and "snuggling all night long." Joe continued to report that the last few days was just like when they first met. Sally stated she had enjoyed their time together, but was afraid it was "just a phase" and that it would go away. Focus of the rest of the session was on how they created this special time, and how it could be maintained
|
Writing Behavioral Goals |
Lends itself to any 2 people agreeing the goal is met |
|
Subject + verb |
|
Action |
|
Frequency |
|
Duration |
|
Monitor |
|
Goals:
·Measurable
·Observable
·
·
·Realistic (achievable)
·Relevant (to the problem)
·Appropriate
·Consistent with the client's values
·Should be able to describe what the client should be able to do to demonstrate improvement/symptom relief
Everything You Ever Wanted To Know About Case Notes
·Think about what you are going to write and formulate before you begin
·Be sure you have the right chart!
·Date and sign every entry
·Proofread
·Record as "late entry" anytime it doesn't fall in chronological order; be timely
·Think about how the client comes through on paper
·Watch
·Errors should have a line through incorrect information. Write error,intital and date
·Write neatly and legibly; print if handwriting is difficult to read
·Use proper spelling, grammar and sentence structure
·Don't leave blank spaces between entries; can imply vital information left out
·Put client name/case number on each page
·Avoid slang,curse words
·Another provider should be able to continue quality care
·Use quotes from client that are clinically pertinent Use descriptive terms
·Describe what you observed, not just your opinion of what you observed
·Reference identified problems from the treatment plan
·Reference diagnostic criteria from
·Use power quotes:
"Client remains at risk for _____________ as evidenced by ___________”
"The current symptoms include _____________”
"Limited progress in ___________”
"Continues to be depressed as evidenced by ____________”
"Client continues to have suicidal ideation as evidenced by the following comment made
to this writer: ____________”
Who Relies On Your Documentation?
Clients’ Families
Rely on your documentation to advocate for the most appropriate and effective care
Physicians
Mental Health Professionals
Referral Sources
Rely on the medical record as an official and practical means of communicating with each other
Rely on your documentation to help them provide a unified treatment approach consistent with your work with the client
Rely on your documentation to provide continuity of care from one treatment setting to another
Employers
Other Payors
Managed Care Companies
Rely on your documentation to justify need for continued treatment, need for admission, demonstrate appropriateness and
Licensing and Accreditation Agencies
Rely on your documentation to verify your practice's quality of care and approve your license to operate
Chart Order
Left side
·Case Contact Summary Sheet
·Intake Form
·Client Information Questionnaire
·Release of Information Cover Letter
·Release of Information from Purdue Marriage and Family Therapy Center
·Informed Consent for Treatment
·Fee Contract
·Fee Receipts (balanced)
·Quality Assurance Review Sheets
Right side
·Treatment Plan (formulated by the 3rd session)
·Case Notes
·All drawings, correspondence, and other direct therapy documentation
·Termination/Transfer/Unopened Case Summaries
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of DAP Notes | The DAP Note Sample form is designed to document therapy sessions using a clear structure. This format facilitates communication about the client's progress and therapeutic interventions. |
| Components of DAP | The form is divided into three sections: "D" for Data, which includes subjective and objective observations; "A" for Assessment, where the therapist's insights and evaluations are recorded; and "P" for Plan, detailing future actions and homework assignments. |
| Client Focus | The DAP format emphasizes the client’s perspective. It captures direct quotes and feelings to provide a comprehensive understanding of the client's mental state and therapy progression. |
| Regulatory Guidance | In the U.S., client documentation must comply with the Health Insurance Portability and Accountability Act (HIPAA), ensuring confidentiality and proper handling of personal health information. |
| Aid in Treatment Continuity | Well-documented case notes support continuity of care by enabling other health professionals to understand the client’s progress and treatment history during referrals or transitions. |
| Documentation Quality | Accurate and clear case notes are essential for effective care. They help justify the necessity for continued treatment and play a role in reimbursement processes by managed care companies. |
Guidelines on Utilizing Dap Note Sample
Filling out the DAP Note Sample form requires attention to detail and a systematic approach. The process involves documenting a client's session by breaking down observations and insights into the designated sections. By closely following the steps outlined below, you can ensure that your notes are comprehensive, clear, and useful for ongoing treatment.
- Gather Information: Before starting, ensure you have all relevant information about the client and the session. This includes session dates, participant details, and any homework assigned.
- Document the Subjective Data: In the "D" section, record what the client said or how they felt during the session. Be specific about their emotions and observations.
- Document the Objective Data: Include observable behaviors, your professional observations, and a summary of progress on the presenting problem. Note any homework review as well.
- Analyze the Session: In the "A" section, provide an assessment of the client's current state. Discuss any hypotheses or insights you may have based on their feedback and your observations.
- Plan Next Steps: In the "P" section, outline your plan for the next session. Specify the date, any topics to cover, and homework for the client to complete before the next meeting.
- Review and Revise: Check your notes for clarity and accuracy. Ensure all entries are dated and signed, and correct any errors promptly according to the guidelines.
What You Should Know About This Form
What is a DAP Note Sample form?
A DAP Note Sample form is a structured document used by mental health professionals to record client sessions. It breaks down into three main parts: D for Data, A for Assessment, and P for Plan. Each section helps therapists provide clear information about what happened in the session, their observations, and the next steps for treatment.
What does the "D" in DAP stand for?
The "D" represents the Data section, which includes both subjective and objective information. Subjective data covers what clients express during sessions, like their feelings or thoughts. Objective data involves observable behaviors, like the client's mood or actions that the therapist notices. This section provides a comprehensive view of the client’s status during the session.
What information should I include in the "A" section?
The "A" section stands for Assessment. This includes the therapist's evaluation of the client's situation. It should highlight any progress, setbacks, or hypotheses about the client's mental health. For example, if a client shows signs of improvement or resistance, it should be noted here, alongside any interpretations the therapist has about these behaviors.
What is the purpose of the "P" section?
The "P" section stands for Plan. It outlines what the therapist intends to do moving forward. This may include scheduling the next session, indicating topics to discuss, and assigning homework for the client. This section ensures that both the client and therapist have a clear understanding of what needs to happen next in therapy.
How should I format the notes in a DAP Note Sample form?
Notes should be clear and concise, using complete sentences. Date each entry and ensure it's organized chronologically. Avoid leaving blank spaces, as this can suggest missing information. Whenever possible, use direct quotes from the client that are relevant to their treatment to add clarity and context.
Why is it important for documentation to be neat and legible?
Proper documentation that is neat and easy to read is crucial in mental health practice. It helps ensure that anyone reviewing the notes can easily understand the client’s status and history. Neat documentation prevents misunderstandings and supports continuity of care among providers. If handwriting is difficult to read, printing should be used for clarity.
Can I use any abbreviations when writing case notes?
Abbreviations should be used with caution. Only approved abbreviations are acceptable to avoid confusion. Each entry should be clear, enabling other therapists or professionals to understand the notes without ambiguity. Unapproved abbreviations can lead to misinterpretations of the client’s needs or treatment plan.
What types of professionals rely on DAP Note documentation?
Multiple stakeholders rely on DAP Note documentation. This includes the clients’ families, other mental health professionals, physicians, employers, and managed care companies. Each group depends on these notes for various reasons, such as ensuring the effectiveness of treatment, compliance with care standards, and even justifying costs associated with the care provided.
How should I address errors in the case notes?
If an error is found in the case notes, it should be crossed out with a line and the correction should be noted alongside it. Include your initials and the date of the correction. This method maintains the integrity of the documentation while ensuring that the corrections are clear and accountable.
What should be included in the chart order of a DAP Note Sample form?
The chart should include several essential documents, organized effectively. On the left side, include items like the Case Contact Summary Sheet, Intake Form, and Informed Consent for Treatment. The right side should include the Treatment Plan and Case Notes. This organization helps create a cohesive and comprehensive record of the client's treatment journey.
Common mistakes
People often encounter several common mistakes when filling out the DAP Note Sample form. These errors can significantly impact the quality of documentation and the continuity of care for clients. First, failing to accurately date each entry can lead to confusion regarding the timeline of treatment. Proper dating is essential, as it establishes a clear chronological order of sessions and interventions. Without accurate dates, it becomes challenging for other providers to understand the progression of a client's treatment.
Another frequent mistake involves the use of excessive abbreviations. While abbreviations can be useful for saving time, using too many or non-standard abbreviations can create misinterpretation. Clarity is vital in documentation, as other professionals rely on these notes to understand a client's history effectively. Abbreviations must be limited to only those that are widely accepted within the field to prevent any misunderstandings that could potentially affect client care.
A third common error occurs when practitioners neglect to include the client's name or case number on each page of the notes. This oversight might seem trivial; however, it can complicate matters when retrieving or sharing documentation. Each page should clearly identify the client to ensure that information is accurately assigned and can be easily located in the event of a review or transfer of care.
Lastly, leaving blank spaces between entries is a mistake that can imply vital information was omitted. It is important to fill out every section of the form completely and thoughtfully. Blank spaces can confuse future readers of the notes, leading to the perception that care was not thorough. Completing each section maximizes the clarity and relevance of the documentation, ultimately improving the quality of ongoing client care.
Documents used along the form
When working with the DAP Note Sample form, several other documents often come into play. Each of these forms serves a specific purpose in the therapeutic process, helping to ensure clear communication and continuity of care. Below is a list of commonly associated documents that you may find useful.
- Intake Form: This document collects essential information from the client at the beginning of treatment. It covers personal details, mental health history, and the reasons for seeking therapy. It helps the therapist understand the client's background and needs.
- Treatment Plan: Created after the initial sessions, this plan outlines the goals for therapy and the methods for achieving them. It serves as a roadmap for both the client and the therapist, detailing what the client hopes to accomplish and how progress will be measured.
- Release of Information Cover Letter: This letter formalizes the client's consent for sharing their information with other healthcare providers or parties involved in their care. This is important for ensuring that all parties are on the same page regarding the client’s treatment.
- Case Contact Summary Sheet: This document summarizes each interaction with the client, noting key points discussed and any follow-up actions required. It acts as a quick reference for both the therapist and any other professionals involved in the client’s care.
- Termination/Transfer Document: This is used when a client completes treatment or is being referred to another provider. It provides details about the therapy process and the client's progress, ensuring that the new provider has a thorough understanding of the client’s history and needs.
These forms, along with the DAP note, create a comprehensive framework for documenting the therapeutic process. They help maintain continuity of care and ensure that information is communicated effectively among everyone involved. Each document plays a key role in supporting the therapeutic relationship and the overall treatment goals.
Similar forms
- SOAP Note: Similar to the DAP Note, the SOAP Note also arranges patient information systematically. It divides details into four sections: Subjective, Objective, Assessment, and Plan, allowing for organized documentation of client sessions.
- Progress Note: Progress Notes detail updates on a client's treatment progress. Much like the DAP Note, these notes capture observations and interventions made during a session, effectively tracking the client's journey.
- Assessment Note: This document focuses primarily on the assessment side of client interactions. Like the DAP Note, it includes observations and clinical impressions that inform treatment planning and future interventions.
- Client Session Summary: This document summarizes key points from client sessions, very similar to the DAP Note in that it synthesizes subjective accounts and observable behaviors to convey the essence of the session.
- Treatment Plan: While more structured, the Treatment Plan shares similarities with the DAP Note in that it outlines objectives and interventions based on the client's specific needs and circumstances observed in therapy sessions.
- Case Management Note: These notes document interactions and interventions to manage a client's care. They relate closely to the DAP Note by capturing essential subjective and objective data, providing a comprehensive view of the client's case.
Dos and Don'ts
When filling out the DAP Note Sample form, it is essential to ensure clarity and compliance with best practices. Below is a concise list of things you should and shouldn't do:
- Do: Provide both subjective and objective data regarding the client clearly.
- Do: Date and sign every entry to maintain an accurate record.
- Do: Use quotes from the client that are clinically relevant to support your observations.
- Do: Ensure your writing is neat and legible for others to understand your notes.
- Don't: Leave blank spaces between entries; this can imply missing vital information.
- Don't: Use slang or curse words; maintain a professional tone throughout.
- Don't: Include personal opinions without supporting observations; focus on factual reporting.
- Don't: Forget to reference the treatment plan and diagnostic criteria from DSM-IV.
Misconceptions
Here are seven common misconceptions about the DAP Note Sample form, along with clarifications to help clear up any confusion.
- All DAP notes are the same. Each note is unique and should reflect the specifics of a session. While the DAP format provides a structure, the content varies based on the client's situation and progress.
- The DAP format is too complicated. Many find the DAP structure to be quite straightforward once they understand each component. It organizes thoughts and observations in a clear way that benefits both the therapist and the client.
- You can skip the subjective data section. This part is crucial as it captures the client’s feelings and thoughts. Ignoring it can lead to a lack of understanding of the client’s perspective and progress.
- Interventions don’t need to be documented thoroughly. Each intervention should be accurately recorded. This is essential for tracking the client’s response to different strategies and ensuring continuity of care.
- Only therapists read DAP notes. In reality, multiple parties often rely on this documentation, including other mental health professionals, families, and insurance providers. Clear and comprehensive notes benefit everyone involved.
- It’s unnecessary to summarize session outcomes. Summarizing helps to reflect on what was accomplished during the session and sets the stage for future sessions. This can guide the therapeutic process effectively.
- Handwriting legibility isn't important. In fact, clear and neat handwriting is vital. Illegible notes can lead to misunderstandings and miscommunications among providers and hinder effective client care.
Key takeaways
- DAP Notes stand for Description, Assessment, and Plan, providing a clear structure for case documentation.
- Begin with the "D" for documenting both subjective feelings expressed by the client and observable behaviors noted by the therapist.
- For the "A", assess the situation and outline your hypothesis or gut feeling about the client’s progress.
- The final part, "P", details the plan for future sessions and any homework assignments for the client.
- Regularly date and sign each entry to ensure your documentation remains organized and verifiable.
- Make certain to proofread your notes for errors, as clarity and accuracy are essential in professional documentation.
- Remember, your notes should provide insight not just for you but also for any other professionals involved in the client’s care.
Browse Other Templates
Easiest Loans to Get Approved for - Let us know if you've applied for a loan with us previously for our records.
Screen Printing Quotes - Remember to indicate the sizes needed: kids or adult sizes.