Fill Out Your Dd 2642 Form
Understanding the DD Form 2642 is essential for anyone navigating the healthcare landscape associated with the TRICARE program. This form, officially titled the TRICARE DoD/CHAMPUS Medical Claim Patient's Request for Medical Payment, serves as a critical tool for beneficiaries seeking reimbursement for medical care received. When providers do not file claims on behalf of their patients, it becomes necessary for individuals to fill out and submit this form to ensure they receive the financial support to which they are entitled. Key components include providing accurate patient and sponsor information, detailing the circumstances of care, and submitting an itemized bill from the medical provider. The form also prompts filers to address any other health insurance coverage, crucial for determining the appropriate reimbursement amounts. While it may seem daunting at first, completing the DD Form 2642 accurately can lead to timely payments and alleviate some financial burdens associated with medical care. It's important to pay close attention to the specific requirements and deadlines for submission, which vary for domestic and overseas claims. This article aims to demystify the process and equip readers with the information necessary to navigate it confidently.
Dd 2642 Example
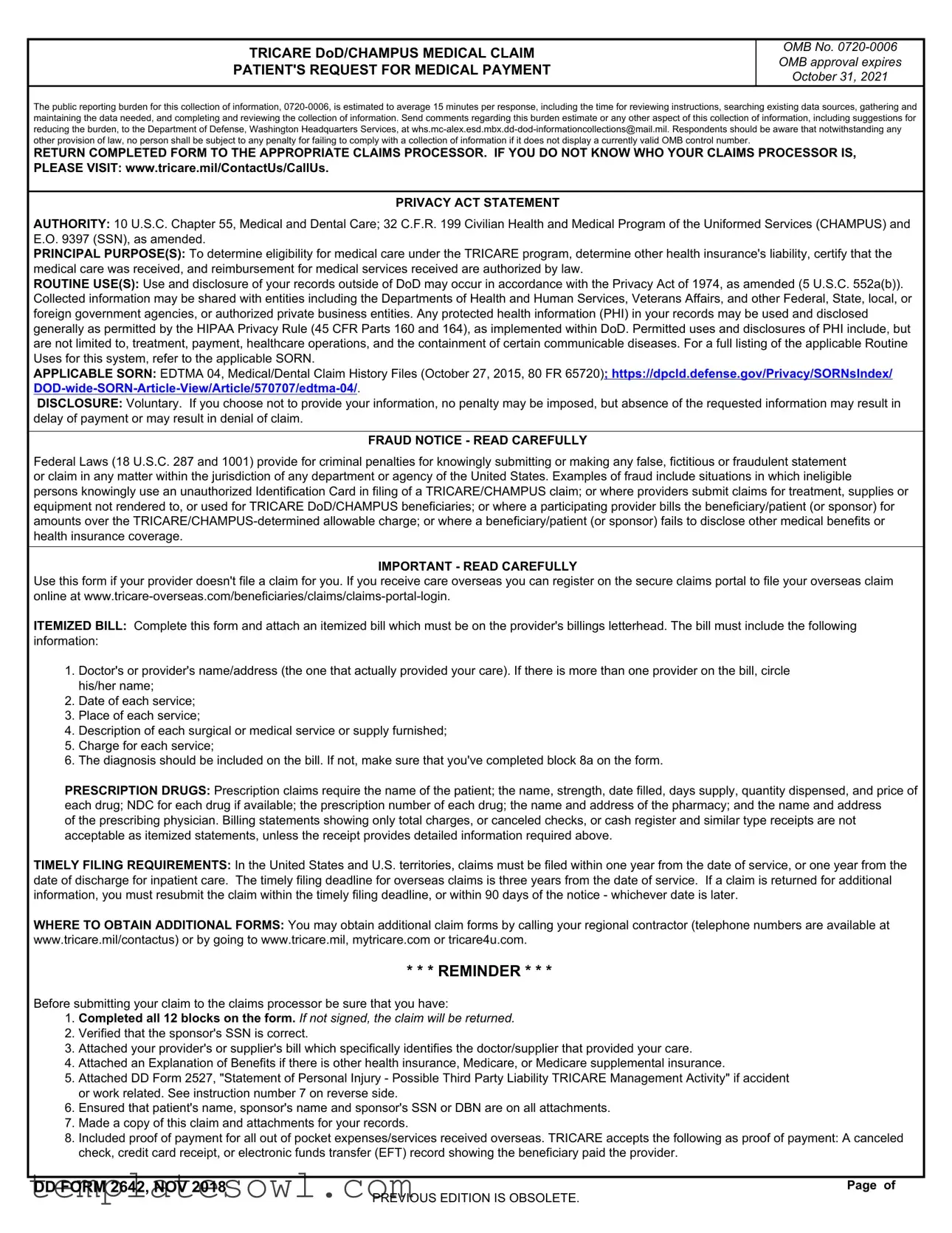
TRICARE DoD/CHAMPUS MEDICAL CLAIM
PATIENT'S REQUEST FOR MEDICAL PAYMENT
OMB No.
The public reporting burden for this collection of information,
RETURN COMPLETED FORM TO THE APPROPRIATE CLAIMS PROCESSOR. IF YOU DO NOT KNOW WHO YOUR CLAIMS PROCESSOR IS, PLEASE VISIT: www.tricare.mil/ContactUs/CallUs.
PRIVACY ACT STATEMENT
AUTHORITY: 10 U.S.C. Chapter 55, Medical and Dental Care; 32 C.F.R. 199 Civilian Health and Medical Program of the Uniformed Services (CHAMPUS) and E.O. 9397 (SSN), as amended.
PRINCIPAL PURPOSE(S): To determine eligibility for medical care under the TRICARE program, determine other health insurance's liability, certify that the medical care was received, and reimbursement for medical services received are authorized by law.
ROUTINE USE(S): Use and disclosure of your records outside of DoD may occur in accordance with the Privacy Act of 1974, as amended (5 U.S.C. 552a(b)). Collected information may be shared with entities including the Departments of Health and Human Services, Veterans Affairs, and other Federal, State, local, or foreign government agencies, or authorized private business entities. Any protected health information (PHI) in your records may be used and disclosed generally as permitted by the HIPAA Privacy Rule (45 CFR Parts 160 and 164), as implemented within DoD. Permitted uses and disclosures of PHI include, but are not limited to, treatment, payment, healthcare operations, and the containment of certain communicable diseases. For a full listing of the applicable Routine Uses for this system, refer to the applicable SORN.
APPLICABLE SORN: EDTMA 04, Medical/Dental Claim History Files (October 27, 2015, 80 FR 65720); https://dpcld.defense.gov/Privacy/SORNsIndex/
DISCLOSURE: Voluntary. If you choose not to provide your information, no penalty may be imposed, but absence of the requested information may result in delay of payment or may result in denial of claim.
FRAUD NOTICE - READ CAREFULLY
Federal Laws (18 U.S.C. 287 and 1001) provide for criminal penalties for knowingly submitting or making any false, fictitious or fraudulent statement or claim in any matter within the jurisdiction of any department or agency of the United States. Examples of fraud include situations in which ineligible persons knowingly use an unauthorized Identification Card in filing of a TRICARE/CHAMPUS claim; or where providers submit claims for treatment, supplies or equipment not rendered to, or used for TRICARE DoD/CHAMPUS beneficiaries; or where a participating provider bills the beneficiary/patient (or sponsor) for amounts over the
IMPORTANT - READ CAREFULLY
Use this form if your provider doesn't file a claim for you. If you receive care overseas you can register on the secure claims portal to file your overseas claim online at
ITEMIZED BILL: Complete this form and attach an itemized bill which must be on the provider's billings letterhead. The bill must include the following information:
1.Doctor's or provider's name/address (the one that actually provided your care). If there is more than one provider on the bill, circle his/her name;
2.Date of each service;
3.Place of each service;
4.Description of each surgical or medical service or supply furnished;
5.Charge for each service;
6.The diagnosis should be included on the bill. If not, make sure that you've completed block 8a on the form.
PRESCRIPTION DRUGS: Prescription claims require the name of the patient; the name, strength, date filled, days supply, quantity dispensed, and price of each drug; NDC for each drug if available; the prescription number of each drug; the name and address of the pharmacy; and the name and address
of the prescribing physician. Billing statements showing only total charges, or canceled checks, or cash register and similar type receipts are not acceptable as itemized statements, unless the receipt provides detailed information required above.
TIMELY FILING REQUIREMENTS: In the United States and U.S. territories, claims must be filed within one year from the date of service, or one year from the date of discharge for inpatient care. The timely filing deadline for overseas claims is three years from the date of service. If a claim is returned for additional information, you must resubmit the claim within the timely filing deadline, or within 90 days of the notice - whichever date is later.
WHERE TO OBTAIN ADDITIONAL FORMS: You may obtain additional claim forms by calling your regional contractor (telephone numbers are available at www.tricare.mil/contactus) or by going to www.tricare.mil, mytricare.com or tricare4u.com.
* * * REMINDER * * *
Before submitting your claim to the claims processor be sure that you have:
1.Completed all 12 blocks on the form. If not signed, the claim will be returned.
2.Verified that the sponsor's SSN is correct.
3.Attached your provider's or supplier's bill which specifically identifies the doctor/supplier that provided your care.
4.Attached an Explanation of Benefits if there is other health insurance, Medicare, or Medicare supplemental insurance.
5.Attached DD Form 2527, "Statement of Personal Injury - Possible Third Party Liability TRICARE Management Activity" if accident or work related. See instruction number 7 on reverse side.
6.Ensured that patient's name, sponsor's name and sponsor's SSN or DBN are on all attachments.
7.Made a copy of this claim and attachments for your records.
8.Included proof of payment for all out of pocket expenses/services received overseas. TRICARE accepts the following as proof of payment: A canceled check, credit card receipt, or electronic funds transfer (EFT) record showing the beneficiary paid the provider.
DD FORM 2642, NOV 2018 |
Page of |
PREVIOUS EDITION IS OBSOLETE.
1. PATIENT'S NAME (Last, First, Middle Initial) |
|
|
2. PATIENT'S TELEPHONE NUMBER (Include Area Code) |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
Primary ( |
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Secondary ( |
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
3. PATIENT'S ADDRESS (Street, Apt. No., City, State, and ZIP Code) |
|
4. PATIENT'S RELATIONSHIP TO SPONSOR (X one) |
|
|
|
|
||||||||||
|
|
|
|
|
|
|
SELF |
|
|
|
STEPCHILD |
|
|
|
|
|
|
|
|
|
|
|
|
SPOUSE |
|
|
|
FORMER SPOUSE |
|
|
|
|
|
|
|
|
|
|
|
|
NATURAL OR ADOPTED CHILD |
OTHER(Specify) |
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5. PATIENT'S DATE OF BIRTH |
6. PATIENT'S SEX |
|
|
7. IS PATIENT'S CONDITION (X both if applicable) |
|
|
|
|
||||||||
(YYYYMMDD) |
(X one) |
|
|
If yes, see #7 in section below |
|
|
|
|
|
|
||||||
|
|
|
|
|
|
ACCIDENT RELATED? |
Yes |
|
No |
|
|
|
|
|||
|
|
MALE |
FEMALE |
WORK RELATED? |
Yes |
|
No |
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
8a. DESCRIBE ILLNESS, INJURY OR SYMPTOMS THAT REQUIRED TREATMENT, SUPPLIES OR |
8b. WAS PATIENT'S CARE (X one) |
|||||||||||||||
MEDICATION. IF AN INJURY, NOTE HOW IT HAPPENED. REFER TO INSTRUCTIONS BELOW. |
INPATIENT? |
PHARMACY? |
||||||||||||||
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
OUTPATIENT? |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
DAY SURGERY? |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
9. SPONSOR'S OR FORMER SPOUSE'S NAME (Last, First, Middle Initial) |
|
|
|
10. SPONSOR'S OR FORMER SPOUSE'S SOCIAL SECURITY |
||||||||||||
|
|
|
|
|
|
|
|
NUMBER OR DOD BENEFITS NUMBER (DBN) |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
11. OTHER HEALTH INSURANCE COVERAGE |
|
|
|
|
|
|
|
|
|
|
|
|
YES |
|||
a. Is patient covered by any other health insurance plan or program to include health coverage available through other family members? For |
|
|||||||||||||||
|
|
|||||||||||||||
patients overseas this includes National Health Insurance. If yes, check the "Yes" block and complete blocks 11 and 12 (see instructions |
|
|
||||||||||||||
|
|
|||||||||||||||
below). If no, you must check the "No" block and complete block 12. Do not provide TRICARE/CHAMPUS supplemental insurance |
|
|
|
NO |
||||||||||||
information, but do report Medicare supplements. |
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
b. TYPE OF COVERAGE (Check all that apply) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
(1) EMPLOYMENT (Group) |
(3) MEDICARE |
|
(5) MEDICARE SUPPLEMENTAL INSURANCE |
|
(7) OTHER (Specify) |
|||||||||||
(2) PRIVATE |
(4) STUDENT PLAN |
|
(6) PRESCRIPTION PLAN |
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c. NAME AND ADDRESS OF OTHER HEALTH INSURANCE |
d. INSURANCE IDENTIFICATION |
|
e. INSURANCE |
|
|
f. DRUG |
|||||||||
|
|
EFFECTIVE DATE |
|
|||||||||||||
|
(Street, City, State, and ZIP Code) |
|
|
|
NUMBER |
|
|
|
|
COVERAGE? |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
(YYYYMMDD) |
|
|
|
|
INSURANCE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
YES |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NO |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
INSURANCE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
YES |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NO |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
REMINDER: Attach your other health insurances's Explanation of Benefits or pharmacy receipt that indicates the actual drug cost, |
|
|
||||||||||||||
|
|
|
amount the OHI paid, and the amount that you paid. |
|
|
|
|
|
|
|
|
|||||
12. SIGNATURE OF PATIENT OR AUTHORIZED PERSON CERTIFIES CORRECTNESS OF CLAIM AND |
|
13. OVERSEAS CLAIMS ONLY: |
||||||||||||||
AUTHORIZES RELEASE OF MEDICAL OR OTHER INSURANCE INFORMATION. |
|
|
||||||||||||||
|
|
|
|
PAYMENT IN US CURRENCY? |
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||
a. SIGNATURE |
|
b. DATE SIGNED |
|
c. RELATIONSHIP TO PATIENT |
|
|
||||||||||
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
(YYYYMMDD) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
No |
|
|
|
Yes |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
HOW TO FILL OUT THE TRICARE/CHAMPUS FORM |
|
|
|
|
|
|
|
|
|||||
|
You must attach an itemized bill (see front of form) from your doctor/supplier for CHAMPUS to process this claim. |
|
|
|
|
|||||||||||
|
|
|
||||||||||||||
1. Enter patient's last name, first name and middle initial as it appears on the |
|
11. By law, you must report if the patient is covered by any other health insurance to |
||||||||||||||
military ID Card. Do not use nicknames. |
|
|
|
|
include health coverage available through other family members. If the patient has |
|||||||||||
2. Enter the patient's primary telephone number and secondary telephone |
|
|
supplemental TRICARE/CHAMPUS insurance, do not report. You must, however, |
|||||||||||||
number to include the area code. |
|
|
|
|
report Medicare supplemental coverage. Block 11 allows space to report two |
|||||||||||
3. Enter the complete address of the patient's place of residence at the time of |
|
insurance coverages. If there are additional insurances, report the information as |
||||||||||||||
service (street number, street name, apartment number, city, state, ZIP Code). |
|
required by Block 11 on a separate sheet of paper and attach to the claim. |
||||||||||||||
Do not use a Post Office Box Number except for Rural Routes and numbers. |
|
NOTE: All other health insurances except Medicaid and TRICARE/CHAMPUS |
||||||||||||||
Do not use an APO/FPO address unless the patient was actually residing |
|
|
supplemental plans must pay before TRICARE/CHAMPUS will pay. With the |
|||||||||||||
overseas when care was provided. |
|
|
|
|
exception of Medicaid and CHAMPUS supplemental plans, you must first submit the |
|||||||||||
4. Check the box to indicate patient's relationship to sponsor. If "Other" is |
|
|
claim to the other health insurer and after that insurance has determined their |
|||||||||||||
checked, indicate how related to the sponsor; e.g., parent. |
|
|
payment, attach the other insurance Explanation of Benefits (EOB) or work sheet to |
|||||||||||||
5. Enter patient's date of birth (YYYYMMDD). |
|
|
this claim. The claims processor cannot process claims until you provide the other |
|||||||||||||
6. Check the box for either male or female (patient). |
|
|
health insurance information. |
|
|
|
|
|
|
|
|
|||||
7. Check box to indicate if patient's condition is accident related, work related |
|
12. The patient or other authorized person must sign the claim. If the patient is |
||||||||||||||
or both. If accident or work related, the patient is required to complete DD |
|
|
under 18 years old, either parent may sign unless the services are confidential and |
|||||||||||||
Form 2527, "Statement of Personal Injury - Possible Third Party Liability |
|
|
then the patient should sign the claim. If the patient is 18 years or older, but cannot |
|||||||||||||
TRICARE Management Activity." Download the form at https://tricare.mil/forms. |
|
sign the claim, the person who signs must be either the legal guardian, or in the |
||||||||||||||
8a. Describe patient's condition for which treatment was provided, e.g., broken |
|
absence of a legal guardian, a spouse or parent of the patient. If other than the |
||||||||||||||
arm, appendicitis, eye infection. If patient's condition is the result of an injury, |
|
patient, the signer should print or type his/her name in Block 12a. and sign the claim. |
||||||||||||||
report how it happened, e.g., fell on stairs at work, car accident. |
|
|
Attach a statement to the claim giving the signer's full name and address, |
|
|
|||||||||||
8b. Check the box to indicate where the care was given. |
|
|
relationship to the patient and the reason the patient is unable to sign. Include |
|||||||||||||
9. Enter the Sponsor's or Former Spouse's last name, first name and middle |
|
documentation of the signer's appointment as legal guardian, or provide your |
||||||||||||||
initial as it appears on the military ID Card. If the sponsor and patient are the |
|
statement that no legal guardian has been appointed. If a power of attorney has |
||||||||||||||
same, enter "same." |
|
|
|
|
been issued, provide a copy. |
|
|
|
|
|
|
|
|
|||
10. Enter the Sponsor's or Former Spouse's Social Security Number (SSN) or Patients 13. If this is a claim for care received overseas, indicate if you want payment in US |
||||||||||||||||
DoD Benefits Number (DBN). |
|
|
|
|
currency. |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DD FORM 2642, NOV 2018 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Page of |
|
PREVIOUS EDITION IS OBSOLETE.
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | The DD 2642 form is used to request medical payment under the TRICARE program. |
| OMB Control Number | The OMB control number for this form is 0720-0006. |
| Average Completion Time | Filling out this form takes about 15 minutes on average. |
| Expiration Date | This form's OMB approval expired on October 31, 2021. |
| Return Instructions | Completed forms should be sent to the appropriate claims processor. |
| Privacy Act Statement | The form operates under the authority of 10 U.S.C. Chapter 55 and 32 C.F.R. 199. |
| Information Disclosure | Your information may be shared with various government agencies as allowed under the Privacy Act of 1974. |
| Timely Filing | Claims must be filed within one year from the date of service in the US, or within three years if overseas. |
| Fraud Notice | Submitting false information is a federal crime and may result in criminal penalties. |
| Additional Forms | Additional claim forms can be obtained by calling your regional contractor or visiting the TRICARE website. |
Guidelines on Utilizing Dd 2642
Completing the DD 2642 form involves various steps, ensuring all necessary information is accurately provided. This form must be returned to the appropriate claims processor once completed. Ensure that all required documents accompany the form to avoid delays in processing.
- Enter the patient's name (last, first, middle initial) as it appears on the military ID card.
- Input the primary and secondary telephone numbers, including the area code.
- Fill in the patient's complete address, including street number, street name, apartment number (if applicable), city, state, and ZIP Code.
- Check the box indicating the patient's relationship to the sponsor; if "Other," specify the relationship.
- Enter the patient's date of birth in YYYYMMDD format.
- Indicate the patient's sex by checking either the male or female box.
- Check if the condition is accident-related, work-related, or both.
- In block 8a, describe the illness, injury, or symptoms that required treatment.
- In block 8b, choose the appropriate care type: inpatient, outpatient, pharmacy, or day surgery.
- Provide the sponsor's or former spouse's name (last, first, middle initial).
- Enter the sponsor’s or former spouse's Social Security Number (SSN) or DoD Benefits Number (DBN).
- Answer whether the patient has other health insurance. If yes, complete blocks 11 and 12; if no, check the "No" block and complete block 12.
- Sign, date, and provide the relationship to the patient in block 12.
- If applicable, in block 13, indicate whether payment should be in US currency for overseas claims.
What You Should Know About This Form
What is the purpose of the DD 2642 form?
The DD 2642 form is a medical claim form used to request payment for medical services received under the TRICARE program. It helps determine eligibility for medical care under TRICARE/CHAMPUS, verifies other health insurance liability, and authorizes reimbursement for eligible medical services. This form is necessary when a healthcare provider does not file a claim on behalf of the patient.
How do I complete the DD 2642 form?
To fill out the DD 2642 form, complete all 12 blocks with accurate information. Include the patient's full name, address, relationship to the sponsor, and relevant medical information. Attach an itemized bill from your healthcare provider, which must contain details like the provider’s name, date and place of service, diagnosis, and charges. Make sure the form is signed; an unsigned form will be returned.
What should I attach to the DD 2642 form?
When submitting the DD 2642 form, attach an itemized bill that is on the provider’s letterhead. The itemized bill should list every service rendered along with diagnostic information. If applicable, also attach an Explanation of Benefits (EOB) from any other health insurance coverage and proof of payment for all out-of-pocket expenses. For overseas claims, provide additional documentation that proves payment was made.
What are the timely filing requirements for submitting the DD 2642 form?
Claims filed under the United States and U.S. territories must be submitted within one year from the date of service or one year from the date of discharge for inpatient care. For claims related to medical services received overseas, you have three years from the date of service to file. If the claims processor returns your claim for more information, you must resubmit the information within the original filing deadline or within 90 days of the notice, whichever date is later.
What happens if I do not provide the requested information?
If you do not provide the required information, the claims processor may delay payment or deny the claim entirely. While there are no penalties for failing to submit the requested information, the absence of this information can significantly affect your claim's processing time and outcome. It's essential to ensure all blocks are completed and all necessary attachments are included to avoid these issues.
Where can I obtain more information or additional forms for the DD 2642?
For more information or to obtain additional copies of the DD 2642 form, you can visit the TRICARE website at www.tricare.mil. You may also contact your regional contractor, whose phone numbers and information are available on the TRICARE contactus page. These resources will guide you through the claims process and help you with any specific questions.
Common mistakes
Filing the DD 2642 form correctly is crucial to ensure timely processing and reimbursement for medical expenses related to the TRICARE program. However, individuals often make various mistakes while completing the form. One common error involves incomplete information. Many claimants fail to fill out all 12 blocks of the form, which can lead to delays or even rejection of the claim. Missing details such as the patient’s date of birth or Social Security number can hinder the claims process significantly.
Another frequent mistake is not verifying that the sponsor’s Social Security Number (SSN) is accurate. An incorrect SSN can create confusion and will likely lead to unnecessary delays in the processing of the claim. Additionally, if the form isn't signed, it will simply be returned. Claimants might overlook this crucial step, mistakenly thinking their submission is complete when it is not.
One error that could cause a denial of the claim is not attaching the required documentation. Claimants often forget to include an itemized bill from the service provider. This bill must detail the services received, including the provider's name and address, as well as a full description of the medical services rendered and their charges. Without this necessary itemization, claims cannot be processed effectively.
Lastly, many individuals fail to report other health insurance coverage. Block 11 on the form explicitly asks for this information, and neglecting to provide it can lead to serious repercussions. If the patient has other insurance, this must be disclosed to allow for a proper processing of the claim. Remember, it’s important to check the “Yes” block if applicable, because the claims processor cannot evaluate the claim without complete disclosure of all existing health insurance.
Documents used along the form
The DD 2642 form, also known as the Patient's Request for Medical Payment, is a crucial document for individuals seeking reimbursement for medical services under the TRICARE program. Along with this form, there are several other documents that often accompany it to ensure a smooth claims process. Here are four common forms and documents that may be required.
- Itemized Bill: This is a detailed invoice from the healthcare provider that lists all the services rendered, including the provider's name, service dates, descriptions, charges, and the diagnosis. It must be printed on the provider’s letterhead to validate the expenses.
- Explanation of Benefits (EOB): This document is issued by other health insurance providers and outlines what services were covered, the amount paid by the insurer, and any remaining balance due from the patient. Submitting the EOB can help TRICARE efficiently process claims when multiple insurances are involved.
- DD Form 2527: Known as the Statement of Personal Injury - Possible Third Party Liability form, this document is necessary if the medical care was related to an accident or workplace incident. It provides essential details about the incident and any potential liability.
- Proof of Payment: To validate out-of-pocket expenses, a document like a canceled check, credit card receipt, or electronic funds transfer record is required. This proof ensures that the payment for medical services was made by the patient.
Having these documents ready can significantly enhance the efficiency of the claims process, minimizing delays and ensuring appropriate reimbursement. Always verify that each document is completed correctly and submitted together to the claims processor for optimal results.
Similar forms
The DD Form 2642 is a critical document for patients seeking reimbursement for medical expenses under the TRICARE program. Several other forms serve similar purposes, with each offering its specific context and requirements. Here’s a list of documents that share similarities with the DD Form 2642:
- CMS-1500 Form: This form is primarily used by medical providers to submit claims for services rendered to patients under Medicare and other health insurances. Like the DD Form 2642, it requires detailed information about the patient, provider, and services provided for claims processing.
- UB-04 Form: Often used by hospitals to bill for inpatient and outpatient services, the UB-04 form captures detailed service information and payment data. Similar to DD Form 2642, it aims to facilitate the reimbursement processes for medical care.
- TRICARE Form 1: This document is utilized for the submission of dental claims under the TRICARE Dental Program. It parallels the DD Form 2642 in that both require patient verification and service details for claims outcomes.
- VA Form 10-10EZ: Utilized by veterans for applying for health care benefits, this form serves a similar purpose in assessing eligibility and covering medical expenses. Like the DD Form 2642, it requires various personal and medical details.
- Medicare Advantage Claim Form: This form allows beneficiaries of Medicare Advantage plans to file claims for medical services received. Much like the DD Form 2642, it specifies the need for detailed billing information to process claims efficiently.
- HMO Claim Form: This form is used by health maintenance organizations for patients to submit claims related to health services. It shares similarities with the DD Form 2642 by requiring comprehensive details about the care received and the costs involved.
- State Medicaid Claim Form: This document is used to request payment from state Medicaid programs. Similarity lies in the necessity for itemized bills and proof of service, akin to what's required with the DD Form 2642.
- Supplemental Health Insurance Claim Form: Individuals can use this form to claim reimbursement from their supplemental insurance after primary insurance has paid. This mirrors the purpose of the DD Form 2642 in covering additional medical expenses.
- DD Form 2527: Specifically aimed at reporting personal injury claims, this form is used when seeking services due to accidents. Like the DD Form 2642, it often involves questions of other insurance coverage and relevant healthcare details.
Each of these forms plays a unique role in the healthcare reimbursement landscape. However, they share a common goal: to ensure that patients can navigate their healthcare options and seek the financial support they need for medical services.
Dos and Don'ts
When filling out the DD 2642 form, there are important guidelines to follow. Here is a list of things you should and shouldn't do:
- Do: Complete all 12 blocks on the form.
- Do: Check that the sponsor's Social Security Number is accurate.
- Do: Attach an itemized bill that clearly identifies the provider.
- Do: Include an Explanation of Benefits if there is other health insurance.
- Do: Make a copy of the claim and all attachments for your records.
- Do: Include proof of payment for any out-of-pocket expenses incurred overseas.
- Do: Sign the form to certify the correctness of the claim.
- Don't: Ignore the timely filing requirements—claims must be submitted within one year.
- Don't: Use nicknames; only enter the patient’s legal name as it appears on the military ID.
- Don't: Provide incomplete or unclear billing statements.
- Don't: Attach receipts that do not contain the required detailed information.
- Don't: Submit claims without verifying that all necessary documents are included.
- Don't: Fail to report coverage from other health insurance plans.
- Don't: Forget to check the box indicating the patient’s relationship to the sponsor.
Misconceptions
Misconception 1: The DD 2642 form is only necessary for outpatient services.
Many believe that this form is only needed for outpatient services, but that’s not entirely accurate. The DD 2642 form must be completed for both inpatient and outpatient care when the provider does not submit a claim on behalf of the patient. It's crucial to remember that this applies regardless of the type or setting of the medical service received.
Misconception 2: You can submit the form without an itemized bill.
There's a common misunderstanding that you can simply submit the DD 2642 form on its own. However, you must attach an itemized bill from the service provider. This bill must be detailed, showing specific information such as the date of service and the type of treatment provided. Without it, the claim cannot be processed correctly, leading to potential delays or denials.
Misconception 3: Filing a claim means you will automatically be reimbursed.
Many individuals think that submitting the DD 2642 form guarantees reimbursement, but this isn't the case. The claim will be reviewed for accuracy and completeness, including verification of eligibility and determination of coverage. Factors such as prior insurance coverage or incomplete information can impact the outcome of your claim.
Misconception 4: You don’t have to worry about deadlines for submitting claims.
It’s a mistaken belief that there are no strict deadlines for submitting the DD 2642 form. Claims must typically be filed within one year from the date of service in the U.S. and three years if you received care overseas. Missing these deadlines can result in your claim being denied, so it’s vital to be aware and proactive in submitting all necessary documents on time.
Key takeaways
When filling out and using the DD 2642 form, keep these key takeaways in mind:
- Use the form when necessary. If your provider does not file a claim on your behalf, it is crucial to complete the DD 2642 form to seek reimbursement.
- Attach an itemized bill. Ensure you include a detailed bill from your healthcare provider, which should contain the provider's information and specifics about the services rendered.
- Check timely filing requirements. Claims must generally be submitted within one year from the service date in the U.S. and within three years for overseas care.
- Complete all 12 blocks. Verify that every section of the form is filled out accurately. An incomplete form may result in delays or denials.
- Provide proof of payment. Attach suitable proof of payment for out-of-pocket expenses. Acceptable forms include canceled checks or credit card receipts that show the payment was made.
- Report other health insurance. If the patient has other health insurance, this must be disclosed on the form, as it affects TRICARE’s payment process.
- Keep copies of everything. Before submitting, make copies of the completed form and all attachments for your records. This is vital in case of future inquiries or disputes.
Attention to these details can ensure smoother processing of your medical claim. Take action promptly to avoid unnecessary delays.
Browse Other Templates
Incident Witness Report,Military Accident Testimony Form,Army Safety Interview Document,Confidential Witness Statement Form,U.S. Army Accident Statement Sheet,Accident Investigation Witness Account,DA Witness Confidentiality Form,Safety Investigation - Clear instructions on confidentiality help guide witnesses through the process.
Form 1049 Client's Statement of Self-employment Income - Instructions are provided for subtracting farm losses from self-employment income.
Dhr Huntsville Al - Be mindful of deadlines to ensure timely access to food assistance.