Fill Out Your Dma 5003 Form
The DMA 5003 form serves as a critical communication tool between the North Carolina Department of Social Services and individuals applying for Medicaid or NC Health Choice. This document outlines both approvals and denials regarding eligibility, providing essential details about the applicant's eligibility period and Medicaid Identification Number (MID). It stipulates that Medicaid covers necessary medical services, with specific provisions for pregnancy-related care and limited family planning services. Importantly, retroactive Medicaid coverage may also be granted for designated periods. Denials, when applicable, include reasons as defined by state regulations, directing individuals toward alternative health insurance options through the Health Insurance Marketplace. Moreover, the form delineates hearing rights, encouraging applicants to seek redress if they disagree with a decision. Applications and hearing requests can be initiated with a caseworker within a stipulated timeframe. Information regarding free legal assistance is provided, emphasizing that individuals have rights throughout the process, including the option to dispute findings or apply for benefits at any time. The DMA 5003 is, therefore, a comprehensive document that not only addresses eligibility but also delineates rights and available recourses for the applicant.
Dma 5003 Example
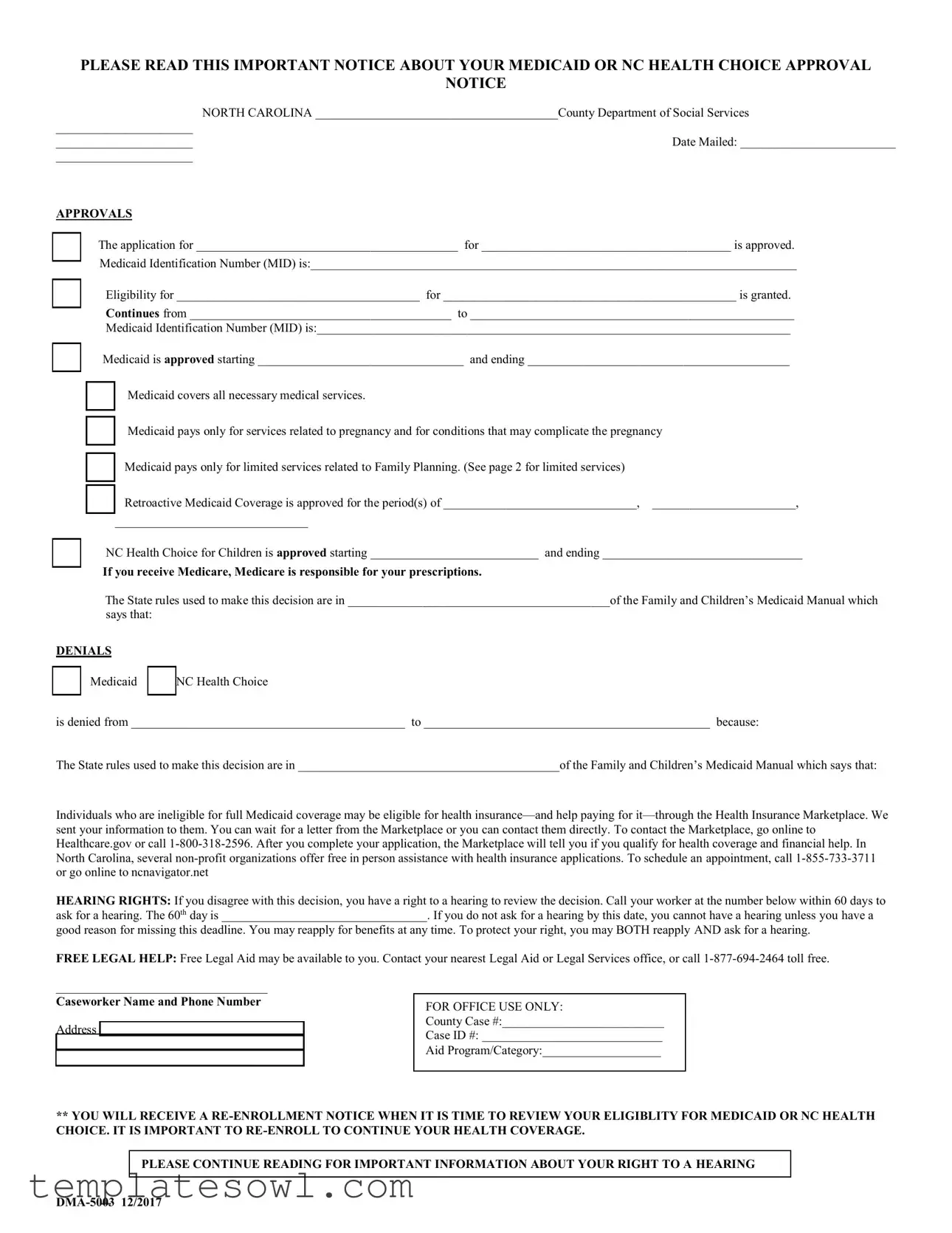
PLEASE READ THIS IMPORTANT NOTICE ABOUT YOUR MEDICAID OR NC HEALTH CHOICE APPROVAL
NOTICE
|
NORTH CAROLINA _______________________________________County Department of Social Services |
______________________ |
|
______________________ |
Date Mailed: _________________________ |
______________________ |
|
APPROVALS
□The application for __________________________________________ for ________________________________________ is approved. Medicaid Identification Number (MID) is:______________________________________________________________________________
□Eligibility for _______________________________________ for _______________________________________________ is granted.
Continues from __________________________________________ to ____________________________________________________
Medicaid Identification Number (MID) is:____________________________________________________________________________
□Medicaid is approved starting _________________________________ and ending __________________________________________
□Medicaid covers all necessary medical services.
□Medicaid pays only for services related to pregnancy and for conditions that may complicate the pregnancy
□Medicaid pays only for limited services related to Family Planning. (See page 2 for limited services)
□ Retroactive Medicaid Coverage is approved for the period(s) of _______________________________, _______________________,
_______________________________
□NC Health Choice for Children is approved starting ___________________________ and ending ________________________________
If you receive Medicare, Medicare is responsible for your prescriptions.
The State rules used to make this decision are in __________________________________________of the Family and Children’s Medicaid Manual which
says that:
DENIALS
□Medicaid
□
NC Health Choice
is denied from ____________________________________________ to ______________________________________________ because:
The State rules used to make this decision are in __________________________________________of the Family and Children’s Medicaid Manual which says that:
Individuals who are ineligible for full Medicaid coverage may be eligible for health
HEARING RIGHTS: If you disagree with this decision, you have a right to a hearing to review the decision. Call your worker at the number below within 60 days to ask for a hearing. The 60th day is _________________________________. If you do not ask for a hearing by this date, you cannot have a hearing unless you have a
good reason for missing this deadline. You may reapply for benefits at any time. To protect your right, you may BOTH reapply AND ask for a hearing.
FREE LEGAL HELP: Free Legal Aid may be available to you. Contact your nearest Legal Aid or Legal Services office, or call
__________________________________
Caseworker Name and Phone Number
Address _________________________
________________________________
________________________________
FOR OFFICE USE ONLY:
County Case #:__________________________
Case ID #: _____________________________
Aid Program/Category:___________________
**YOU WILL RECEIVE A
PLEASE CONTINUE READING FOR IMPORTANT INFORMATION ABOUT YOUR RIGHT TO A HEARING
Is there a problem? |
|
You can ask for a hearing. |
Did you know you have the right to see your |
|
|
|
record? |
If you think we are wrong or you have new information, you have the right to a hearing. You must ask for this hearing within 60 days (or 90 days if you have a good reason for delay). This hearing is a meeting to review your case and give you the correct benefits if it was wrong.
Call or write your caseworker to ask for a hearing. A local hearing will be held within 5 days of your request unless you ask for it to be postponed. The hearing can be postponed, for good reasons, for as much as 10 calendar days. Then, if you think the decision in the local hearing is wrong, call or write your caseworker WITHIN 15 DAYS to ask for a second hearing. The second hearing is before a state hearing official.
If you are requesting a hearing about disability, call or write your caseworker to ask for a hearing. There is no local hearing. A state hearing officer holds the disability hearing.
Did you know you have the right to be represented?
You may have someone speak for you at your hearing, such as a relative or a paralegal or attorney obtained at your expense. Free legal services may be available in your community. Contact your nearest Legal Aid or Legal Services office, or call
If you have additional questions or concerns, contact
your caseworker for information, or call the DHHS Customer Service Center, Information and Referral Service, toll free at
If you ask, your caseworker will show you (or the person speaking for you) your benefits record before your hearing. If you ask, you may also see other information to be used at the hearing. You can get free copies of this information. You may see this information again at your hearing.
Do you understand your rights?
Do you understand how to get a hearing? If you have any questions, please contact your caseworker as soon as possible.
Don’t forget to report all changes to your county department of social services within 10 calendar
days (5 calendar days for Special Assistance). If you don’t know whether a change is important,
ask your caseworker. If you do not truthfully report information and changes, you may be guilty of a misdemeanor or felony.
Family Planning Limited Services
Family planning services include one annual physical exam per 365 days, which should be scheduled as your first appointment and six family planning visits per 365 days. Services include contraceptive services and supplies, permanent sterilization, and screening for sexually transmitted infections (STDs) and HIV screening. You can access these services through a health department, community health or rural health clinic, or by any provider in your community who accepts your Family Planning Medicaid coverage. If you choose permanent sterilization and the necessary post- surgical
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of DMA 5003 | This form serves as an approval and denial notice for Medicaid and NC Health Choice applications in North Carolina. |
| Eligibility Criteria | Eligibility for Medicaid is determined based on various state rules outlined in the Family and Children’s Medicaid Manual. |
| Hearing Rights | Individuals can request a hearing within 60 days if they disagree with a decision regarding their benefits. |
| Retroactive Coverage | The form can approve retroactive Medicaid coverage for specific past periods if applicable. |
| Free Legal Assistance | Residents may contact local legal aid services for free legal help in navigating their Medicaid applications. |
| Family Planning Services | Medicaid offers limited family planning services, including annual exams and contraceptive consultations. |
| Importance of Re-enrollment | A notice for re-enrollment will be sent, and it is crucial to complete this to maintain health coverage. |
Guidelines on Utilizing Dma 5003
Completing the DMA 5003 form requires careful attention. You’ll need to provide specific information regarding your Medicaid or NC Health Choice approval. Make sure to gather all relevant documents before starting. Follow the steps below to ensure accuracy and completeness.
- Obtain the DMA 5003 form: You can find the form online or request a physical copy from your county department of social services.
- Fill in your personal information: Enter your full name, date of birth, and Social Security number at the top of the form.
- County Department Information: Indicate the name of your county department of social services and the date the document is being mailed.
- Approval or Denial Section: Check the appropriate box for approval or denial of Medicaid and fill in all necessary details related to your application.
- Medicaid Identification Number (MID): If applicable, write down your Medicaid Identification Number in the specified area.
- Eligibility Dates: Clearly state the beginning and ending dates of eligibility as indicated on your approval or denial notification.
- Retroactive Coverage: If granted retroactive Medicaid coverage, list the specific periods of coverage.
- Contact Information: Record the caseworker’s name and phone number, ensuring accuracy to facilitate future communication.
- Review the Additional Information: Read through any additional instructions regarding your rights, hearing requests, and available assistance.
- Submit the Form: Make a copy of the completed form for your records. Then send the DMA 5003 to the appropriate department as instructed.
Once the DMA 5003 form is filled out and submitted, you should expect further communication from your county department regarding the status of your application. It’s crucial to stay informed about your Medicaid or NC Health Choice coverage so you can continue to access necessary medical services without interruption.
What You Should Know About This Form
What is the DMA 5003 form?
The DMA 5003 form serves as an approval or denial notice for applicants seeking Medicaid and NC Health Choice benefits in North Carolina. It informs recipients about their eligibility status, effective dates for coverage, and essential details regarding the services covered. The document plays a crucial role in ensuring that applicants understand their rights and responsibilities within the program.
How do I know if my Medicaid application has been approved or denied?
Your approval or denial will be clearly indicated on the DMA 5003 form. If your application is approved, the form will list the Medicaid Identification Number (MID) along with the effective dates of coverage and details about the medical services that Medicaid will pay for. Conversely, if denied, the form will state the reason for the denial along with the period during which coverage is not granted.
What should I do if I disagree with the decision on my DMA 5003 form?
If you disagree with the decision stated on your DMA 5003 form, you have the right to request a hearing. It is essential to contact your caseworker within 60 days from the date on the notice. This hearing will allow you to appeal the decision and present your case. If you miss the deadline, you may still be able to request a hearing if you have a valid reason for the delay.
What types of services does Medicaid cover according to the DMA 5003 form?
The DMA 5003 form specifies that Medicaid covers all necessary medical services, including services related to pregnancy. However, it is important to note that coverage for family planning services is limited. The form outlines that retroactive Medicaid coverage may also be granted for specified periods.
Can I receive free legal assistance regarding issues with my DMA 5003 form?
Yes, free legal assistance may be available to you if you are facing issues or have concerns related to your DMA 5003 form. You can reach out to your nearest Legal Aid or Legal Services office for support. Additionally, calling 1-877-694-2464 toll-free can connect you with resources and information regarding legal assistance.
What is the process for hearing rights if I want to appeal my case?
The process begins by contacting your caseworker to request a hearing within the designated timeframe (60 days). A local hearing will be held within five days unless you request a postponement. If you disagree with the outcome of the local hearing, you can request a second hearing before a state hearing officer within 15 days of receiving that decision.
How can I keep my Medicaid or NC Health Choice coverage active?
To maintain your coverage, it is crucial to re-enroll when you receive a re-enrollment notice. Additionally, you must report any changes to your condition or circumstances to your local Department of Social Services within 10 calendar days. This proactive approach ensures that you continue to receive health benefits without interruption.
Common mistakes
When individuals fill out the DMA-5003 form, various mistakes can lead to delays or denials of Medicaid or NC Health Choice benefits. Understanding these common errors is critical to ensure timely and accurate processing.
One frequent mistake involves incomplete or incorrect information. Applicants may fail to provide essential details such as their Medicaid Identification Number (MID), leading to confusion in case processing. Omitting information can result in unnecessary delays, and any misreported information may cause outright denials.
Another common error is overlooking the deadlines for requests and appeals. When individuals do not ask for a hearing within 60 days of receiving a decision, they lose their right to challenge that decision. Misunderstanding this timeframe can result in losing benefits without recourse.
Many applicants also neglect to report significant changes affecting their eligibility. Changes in income or family size should be reported within 10 calendar days. Failure to disclose this information may lead to penalties or denied benefits later on.
Additionally, some individuals focus solely on submitting the application without seeking necessary assistance. Many families might benefit from nonprofit organizations providing free in-person help with applications. Delaying this assistance may lead to misfiled applications and subsequent approval issues.
Some applicants mistakenly ignore the importance of understanding the coverage limits associated with the benefits. Medicaid does not cover all services, and relying on incorrect assumptions can lead to unexpected medical bills. Being well-informed about what Medicaid covers is essential.
Moreover, individuals may not realize they need to reapply periodically. Failing to respond to re-enrollment notices can disrupt access to necessary healthcare services. Keeping track of these notifications is vital for maintaining health coverage.
Applicants sometimes also lack awareness regarding their right to representation during hearings. Many do not consult with legal aid or other representatives who could better navigate the process. Having skilled assistance can make a significant difference in the outcome of appeals.
Lastly, not understanding one’s rights can create obstacles. Many individuals are unaware of their rights to see their benefits records or have someone help them during hearings. Awareness of these rights is crucial for effective advocacy.
By avoiding these common mistakes, applicants can improve their chances of securing the healthcare benefits they need. Careful attention to detail during the application process is not just helpful; it is essential for timely access to necessary services.
Documents used along the form
The DMA 5003 form serves as a crucial document for individuals navigating Medicaid or NC Health Choice in North Carolina. It informs recipients about their approval, denial status, and rights regarding healthcare coverage. Alongside this form, several other documents are often used in conjunction with it to support applicants in understanding their eligibility, appeal rights, and necessary procedures. Below is a list of key forms that may accompany the DMA 5003 form.
- DMA-5010: This is the Medicaid Application form. It is used to apply for Medicaid benefits and collects essential personal information, income details, and other eligibility criteria required to determine qualification.
- DMA-5012: This is the Medicaid Renewal form. It allows current beneficiaries to provide updated information to continue receiving Medicaid benefits without interruption.
- DMA-5016: Known as the Medicaid Notice of Decision, it provides a comprehensive explanation of the reasons behind approval or denial of Medicaid benefits, including pertinent state rules used in the decision-making process.
- DMA-5020: This form is used to request a Fair Hearing regarding Medicaid eligibility decisions. It allows individuals to formally contest a determination they disagree with, ensuring their right to appeal is upheld.
- DMA-7030: The Medicaid Change Report form is used to inform the Department of Social Services about changes in circumstances that could affect eligibility, such as changes in income or family size.
- Health Insurance Marketplace Application: This application is used to explore options for health coverage outside of Medicaid, providing details necessary to determine if individuals qualify for coverage and financial assistance through the Marketplace.
- Form 1095-A: This form is sent from the Health Insurance Marketplace, detailing coverage status for the tax year, important for filing taxes related to health insurance under the Affordable Care Act.
- Client Contracts or Agreements: These may include various legal documents that outline the responsibilities and rights of the applicant and the service provider, establishing clear terms before services are rendered.
Understanding these additional forms will aid individuals in better managing their Medicaid-related needs. Each document serves a specific purpose, helping navigate the complex healthcare landscape while ensuring that individuals are informed about their rights and responsibilities.
Similar forms
-
Medicaid Application Form: Much like the DMA 5003, the Medicaid Application Form serves as an official document to apply for Medicaid benefits. It collects necessary information about the applicant’s financial and personal circumstances to determine eligibility for various health services.
-
Approval Letter for Medicaid Benefits: This document outlines the approval of Medicaid benefits, including the specific medical services covered. Similar to the DMA 5003, it communicates critical details about eligibility periods and any limitations on coverage.
-
Notice of Action for Medicaid: This notice informs applicants about the status of their application. Whether approved or denied, it contains information regarding the reasoning behind the decision, closely resembling the DMA 5003’s structure, which outlines the approval and denial of benefits.
-
Medicaid Re-Enrollment Notice: Just as the DMA 5003 indicates the re-enrollment process for continued coverage, this notice specifically prompts recipients to renew their eligibility and provides guidance on how to do so, ensuring uninterrupted health coverage.
-
Medicaid Hearing Request Form: Similar to the DMA 5003's instructions on requesting a hearing, this form allows individuals to formally appeal decisions regarding their Medicaid eligibility. It provides individuals with information on their rights and the process for contesting decisions.
-
Health Insurance Marketplace Application: Although focused on a different health coverage avenue, this application functions similarly to the DMA 5003 by collecting relevant information to determine eligibility for health coverage and financial assistance through the marketplace.
Dos and Don'ts
When filling out the DMA 5003 form, it is important to follow the right steps to ensure your application is processed smoothly. Here are seven things you should and shouldn't do:
- Do ensure all personal information is complete and accurate.
- Don't leave any sections blank unless instructed to do so.
- Do double-check your Medicaid Identification Number (MID) for correctness.
- Don't submit your application late or after the deadline.
- Do report any changes in your status immediately to your caseworker.
- Don't provide false information, as this can lead to serious consequences.
- Do ask for help if you're unsure about any part of the form.
Taking the time to follow these guidelines can help avoid delays or issues with your application.
Misconceptions
Understanding the DMA-5003 form is crucial for anyone navigating Medicaid or NC Health Choice. However, several misconceptions can lead to confusion. Here’s a look at five common myths:
- The DMA-5003 form guarantees approval for Medicaid. Many believe that simply submitting the form results in automatic approval. In reality, eligibility depends on various factors, including income and household size.
- Medicaid only covers basic health needs. Some people think that Medicaid provides limited services. However, it actually covers a range of medical services, including preventive care and treatments for chronic conditions.
- You cannot ask for a hearing after a denial. There’s a misconception that if your Medicaid application is denied, you can’t contest it. In truth, individuals have the right to request a hearing within 60 days to review the decision.
- Free legal help is not available for Medicaid issues. Many assume that legal assistance is only for serious legal matters. However, free legal aid is often accessible for individuals needing help with Medicaid applications and denials.
- You cannot report changes once your application is submitted. Some think they can simply submit their application and forget about it. Reporting changes to your situation—like income or household changes—is essential and required within a specific timeframe.
By clearing up these misconceptions, individuals will have a better understanding of the DMA-5003 form and their rights within the Medicaid system. Awareness and accurate information empower you in your healthcare journey.
Key takeaways
Filling out and using the DMA 5003 form is an important step in managing health coverage through Medicaid or NC Health Choice. Here are four key takeaways:
- Eligibility Notification: The form indicates whether an application for Medicaid or NC Health Choice has been approved or denied. It includes specific dates and services covered under the approval.
- Hearing Rights: If there is a disagreement with the decision, individuals have the right to request a hearing within 60 days. This allows for a review of the case and a chance to potentially correct any errors.
- Free Legal Assistance: Access to free legal aid is available for those who may need help navigating the Medicaid process. Individuals can contact local Legal Aid offices for support.
- Reporting Changes: Any changes in circumstances must be reported to the county department of social services within specific time frames. Not reporting accurately may lead to legal consequences.
Browse Other Templates
Hazmat Bill of Lading Pdf - The document clarifies terms related to freight charges and payment responsibilities.
How Much Does a Live Scan Cost - It verifies your identity through an official photo document, such as a driver's license or passport.
Complaint Letter to Council - Support for a unified effort to enhance local water protection standards.