Fill Out Your Dmas 225 Form
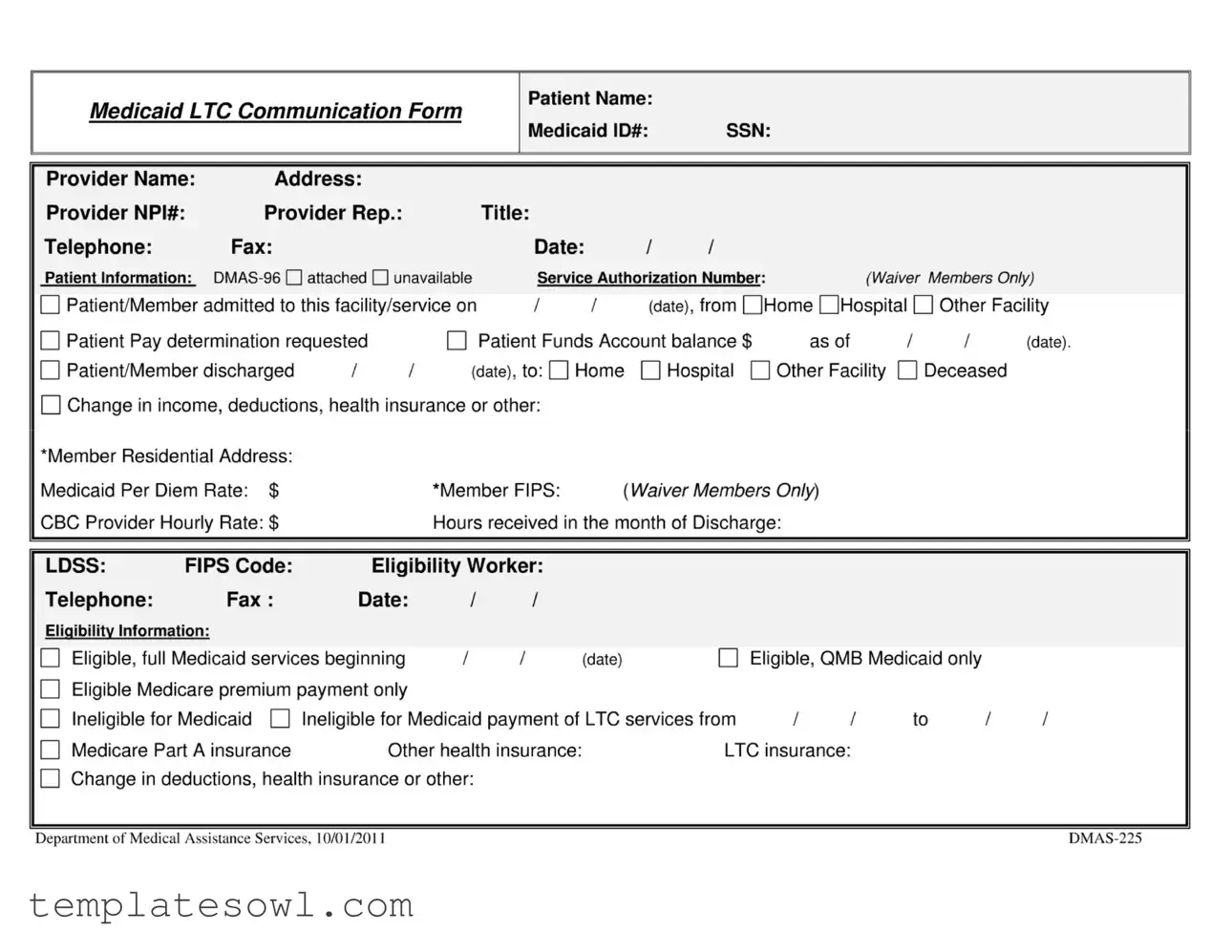
The DMAS 225 form, a crucial document within the Medicaid framework, serves as a vital communication tool between local Departments of Social Services and nursing facilities or Community-Based Care (CBC) Waiver Providers. Ensuring the continuous flow of essential information, the form addresses several key aspects related to patient admission, discharge, and eligibility changes. It captures critical data such as the patient's name, Medicaid identification number, Social Security number, and service authorization number, particularly for waiver members. This form is used to document various factors influencing a member's Medicaid eligibility status, including changes in income, health insurance, or personal circumstances. Furthermore, it requires providers to report any adjustments in the level of care a patient may need. The proper usage of the DMAS 225 form necessitates attention to detail, as accurate completion is essential not only for maintaining compliance with Medicaid regulations but also for ensuring that patients receive the necessary assistance and services promptly. Timely submission and transparent communication can significantly impact an individual's access to critical care and support services, highlighting the form's importance in the broader Medicaid landscape.
Dmas 225 Example
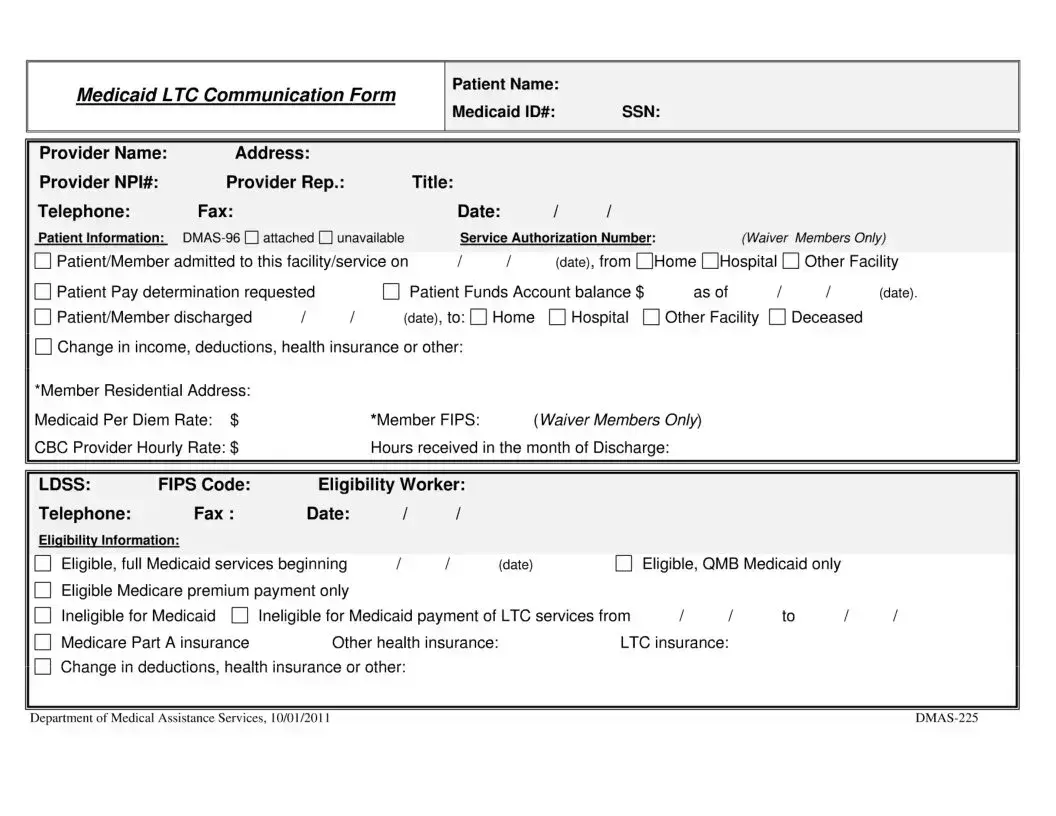
Medicaid LTC Communication Form
Patient Name:
Medicaid ID#: |
SSN: |
Provider Name: |
Address: |
|
|
|
|
|
|
|
|
|
|
|
Provider NPI#: |
Provider Rep.: |
|
|
Title: |
|
|
|
|
|
|
|
|
Telephone: |
Fax: |
|
|
|
Date: |
/ |
/ |
|
|
|
|
|
Patient Information: |
|
Service Authorization Number: |
(Waiver Members Only) |
|||||||||
Patient/Member admitted to this facility/service on |
/ |
/ |
(date), from QHome OHospital |
|
Other Facility |
|||||||
Patient Pay determination requested |
|
|
Patient Funds Account balance $ |
as of |
I |
I |
(date). |
|||||
Patient/Member discharged |
/ |
/ |
(date), to: |
Home |
|
Hospital О Other Facility |
|
Deceased |
|
|||
Change in income, deductions, health insurance or other:
‘Member Residential Address:
Medicaid Per Diem Rate: $ |
‘Member FIPS: |
{WaiverMembers Only) |
CBC Provider Hourly Rate: $ |
Hours received in the month of Discharge: |
|
LDSS: FIPS Code: Eligibility Worker:
Telephone: |
Fax: |
Date: |
|
/ |
/ |
|
|
|
|
Eligibility Information: |
|
|
|
|
|
|
|
|
|
Eligible, full Medicaid services beginning |
1 |
/ |
(date) |
|
Eligible, QMB Medicaid only |
|
|||
Eligible Medicare premium payment only |
|
|
|
|
|
|
|
||
Ineligible for Medicaid |
Ineligible for Medicaid payment of LTC services from |
II |
to |
II |
|||||
Medicare Part A insurance |
Other health insurance: |
LTC insurance: |
|
|
|||||
Change in deductions, health insurance or other:
Department of Medical Assistance Services, 10/01/2011 |
Medicaid LTC Communication Form, Effective 10/01/2011 |
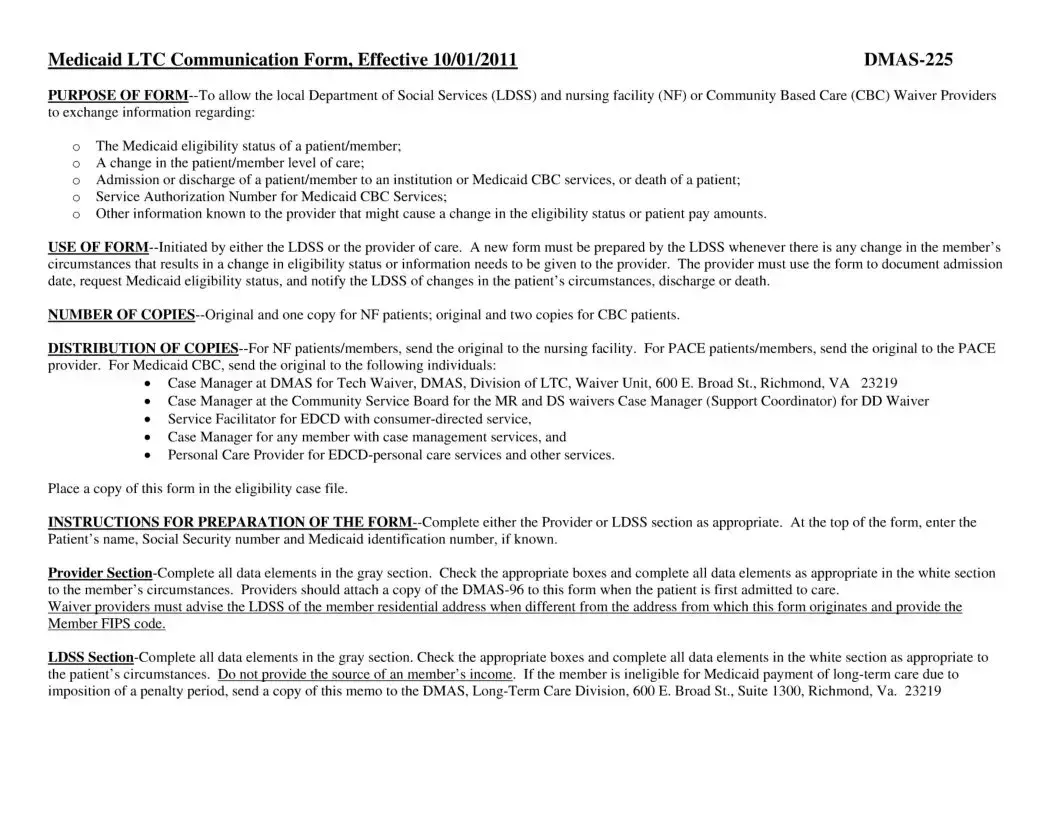
PURPOSE OF
оThe Medicaid eligibility status of a patient/member;
оA change in the patient/member level of care;
оAdmission or discharge of a patient/member to an institution or Medicaid CBC services, or death of a patient;
оService Authorization Number for Medicaid CBC Services;
оOther information known to the provider that might cause a change in the eligibility status or patient pay amounts.
USE OF
NUMBER OF
DISTRIBUTION OF
•Case Manager at DMAS for Tech Waiver, DMAS, Division of LTC, Waiver Unit, 600 E. Broad St., Richmond, VA 23219
•Case Manager at the Community Service Board for the MR and DS waivers Case Manager (Support Coordinator) for DD Waiver
•Service Facilitator for EDCD with
•Case Manager for any member with case management services, and
•Personal Care Provider for
Place a copy of this form in the eligibility case file.
INSTRUCTIONS FOR PREPARATION OF THE
Provider
Waiver providers must advise the LDSS of the member residential address when different from the address from which this form originates and provide the Member FIPS code.
LDSS
Form Characteristics
| Fact Name | Detail |
|---|---|
| Purpose | The DMAS-225 form allows the local Department of Social Services (LDSS) and care providers to exchange key information about Medicaid eligibility, patient admission, discharge, and changes in status. |
| Initiation | This form can be initiated by either the LDSS or the provider of care whenever there is a change in the member's circumstances. |
| Documentation Requirement | A new DMAS-225 form must be prepared for any change affecting the member’s eligibility status or other relevant information. |
| Number of Copies | For nursing facility (NF) patients, one original and one copy is needed; for Community Based Care (CBC) patients, one original and two copies are required. |
| Distribution of Copies | The original for a NF must be sent to the nursing facility, while CBC providers receive originals based on specific case manager roles and services. |
| Patient Information | The form collects crucial patient information including Medicaid ID, provider details, admission dates, and discharge plans. |
| Eligibility Information | Sections for eligibility status include full Medicaid services, Medicare premium payment only, and pending changes due to income fluctuations or insurance updates. |
| Governing Laws | The form complies with Virginia Medicaid regulations and ensures adherence as per DMAS policies established on 10/01/2011. |
| Instructions for Use | Details on how to fill out the form are outlined clearly, requiring completion of either the Provider or LDSS section as appropriate based on the patient’s circumstances. |
Guidelines on Utilizing Dmas 225
Filling out the DMAS 225 form requires attention to detail, particularly concerning patient information and eligibility status. The following instructions will guide you through the process of completing the form efficiently and accurately.
- At the top of the form, provide the patient's name, Social Security number (SSN), and Medicaid ID number if known.
- Fill in the provider's name, address, and National Provider Identifier (NPI) number.
- Include the name and title of the provider representative, along with their telephone and fax numbers.
- Record the date on which the form is filled out.
- Indicate whether the DMAS-96 form is attached or unavailable.
- If applicable, enter the service authorization number for Medicaid Waiver members.
- Document the date when the patient/member was admitted to the facility/service, including the name of the previous facility (e.g., home, hospital, or other).
- For patient pay determination, enter the patient's funds account balance and the corresponding date.
- Specify the discharge date and the location to which the patient/member is being discharged (home, hospital, or other facility).
- Note any changes in income, deductions, health insurance, or other relevant information.
- Provide the member’s residential address, Medicaid per diem rate, CBC provider hourly rate, and Member FIPS if applicable.
- List the hours of service received if known.
- In the eligibility information section, check the appropriate eligibility status and enter the date when full Medicaid benefits begin, if applicable.
- Document any other health insurance or long-term care insurance information.
- If necessary, convey any changes in deductions, health insurance, or other relevant details.
- Ensure the form is complete with all relevant signatures and dates.
- For NF patients/members, send the original to the nursing facility. For CBC patients, distribute the original to designated case managers and others as specified in the form’s instructions.
What You Should Know About This Form
What is the purpose of the DMAS 225 form?
The DMAS 225 form serves as a vital communication tool between the local Department of Social Services (LDSS), nursing facilities (NF), and Community Based Care (CBC) Waiver providers. Its main aim is to provide essential information regarding a patient's Medicaid eligibility status, any changes in the patient’s level of care, admission or discharge details, as well as notifications of a patient’s death. Additionally, it helps in documenting service authorization numbers for Medicaid CBC services and conveys any changes that could impact the patient’s eligibility or financial responsibilities.
Who is responsible for initiating the DMAS 225 form?
Either the local Department of Social Services or the care provider can initiate the DMAS 225 form. This ensures that all relevant parties have the most up-to-date information regarding changes in a member's circumstances. When a change occurs that affects the member’s eligibility status, a new form must be prepared by the LDSS to reflect these updates. This collaborative approach aims to streamline communication and enhance care coordination.
How many copies of the DMAS 225 form are needed, and who receives them?
For patients in nursing facilities, the original DMAS 225 form and one copy are required. For those utilizing CBC services, the original and two copies must be completed. The original form is sent directly to the nursing facility for NF patients or to the PACE provider for PACE patients. For Medicaid CBC members, the original is distributed to various individuals, including the case manager at DMAS and other relevant stakeholders, while a copy should remain in the eligibility case file. This multi-copy approach ensures that everyone involved is informed and can act accordingly.
What instructions should be followed when completing the DMAS 225 form?
When filling out the DMAS 225 form, either the provider or the LDSS section must be completed, depending on who is submitting the form. Key information, such as the patient’s name and Medicaid ID number, should be clearly entered at the top of the form. For the provider section, all boxes should be checked accurately, and data elements completed as they pertain to the patient’s situation. Additionally, if a patient is being admitted for the first time, the provider is advised to attach a DMAS-96 form. It’s crucial to ensure that sensitive information, like the source of income, remains confidential. This attention to detail helps in maintaining compliance and protecting patient information.
What happens if a member changes their eligibility status?
If a member experiences a change in circumstances that affects their eligibility for Medicaid long-term care, it is essential to notify the appropriate parties using the DMAS 225 form. If a member is determined to be ineligible due to a penalty period, the LDSS must send a copy of the notification memo to the DMAS Long-Term Care Division in Richmond, Virginia. This prompt communication ensures that all relevant parties can adjust accordingly and facilitates better management of the patient's care needs.
Common mistakes
Filling out the DMAS 225 form requires attention to detail, and many people make mistakes that can delay processing or lead to complications. One common error is neglecting to provide complete patient information. This includes the patient’s full name, correct Medicaid ID number, and Social Security number. Incomplete information can hinder communication between the provider and the local Department of Social Services, causing unnecessary delays in care.
Another mistake often made involves the failure to document changes promptly. If there are any alterations in the patient’s circumstances—like a change in income, health insurance, or discharge information—the form needs to be updated immediately. Ignoring these changes can lead to incorrect eligibility statuses or payment amounts, which can negatively impact the patient’s access to care and services.
Some individuals also overlook the requirement to attach necessary documentation, such as the DMAS-96 form when admitting the patient. Not providing all required documents can slow down the approval process for Medicaid services. Providers should consistently check that all attachments are included before submitting the form.
Lastly, people frequently fail to make the appropriate copies of the form. Depending on whether the patient is in a nursing facility or receiving community-based care, the number of copies required varies. For nursing facility patients, two copies must be made, while community-based care requires three. Omitting this step can result in delays and confusion regarding the care being provided.
Documents used along the form
The DMAS 225 form, officially known as the Medicaid LTC Communication Form, facilitates communication between the local Department of Social Services (LDSS) and nursing facilities or Community Based Care (CBC) Waiver Providers. Various other forms and documents accompany the DMAS 225 form, helping to ensure effective management of Medicaid services. Below are some of the key documents commonly used in conjunction with the DMAS 225 form.
- DMAS-96: This document serves as a Medicaid Waiver application form. It captures essential information about the patient’s health status, needs, and services required. Providers typically attach the DMAS-96 to the DMAS 225 when a patient is first admitted to care.
- DMAS-10: This form is used for reporting changes in a patient’s circumstances, such as shifts in income or residence. The DMAS-10 helps maintain up-to-date eligibility information for Medicaid services.
- Patient Pay Determination Form: This form calculates the amount a patient is required to contribute toward their care based on their income and resources. It is essential in determining financial responsibility and assists local agencies in planning resources.
- Accredited Waiver Provider Service Plan: This document outlines the care and services an individual will receive within a waiver program. It includes details on care goals, provider responsibilities, and service delivery methods, ensuring that all aspects of the patient’s care are coordinated effectively.
- Medicaid Application for Long Term Care: This application is essential for patients seeking Medicaid assistance for long-term care services. It collects comprehensive information about the patient’s finances, medical history, and eligibility for Medicaid benefits.
Each of these documents serves a crucial role in the Medicaid process, facilitating information exchange and ensuring compliance with regulations. Proper completion and timely submission of these forms help streamline the provision of care and support for Medicaid recipients.
Similar forms
The DMAS 225 form, also known as the Medicaid LTC Communication Form, shares similarities with several other important documents related to Medicaid services and patient information. Below are five documents that are conceptually linked to the DMAS 225 form:
- DMAS-96 - This form is typically attached to the DMAS 225 to provide detailed information about the patient’s status and eligibility. It allows for the documentation of the patient's medical condition and ensures accurate reporting in conjunction with the DMAS 225.
- Medicaid Application Form - The initial application for Medicaid services is foundational for determining eligibility. Just like the DMAS 225, this application gathers vital information about the applicant's financial and medical status, ensuring that patients qualify for the necessary services.
- Patient Pay Determination Form - This document assesses how much a patient must contribute towards their care. Similar to the DMAS 225, it involves financial evaluations and eligibility assessments to determine the patient’s share of cost for long-term care.
- Service Plan for Community-Based Services - This plan outlines the services that a patient will receive, evolving in response to their needs. This is akin to the DMAS 225 in that both documents facilitate communication between providers about the patient’s care level and eligibility for services.
- Nursing Facility Admission Agreement - This agreement specifies the terms and conditions of the resident's stay at a facility. Like the DMAS 225, it details patient information, including care expectations and responsibilities, ensuring that all parties understand the arrangement ahead of the patient’s admission.
Dos and Don'ts
When filling out the DMAS 225 form, here are eight important do's and don'ts:
- Do enter the patient’s name, Social Security number, and Medicaid ID number accurately at the top of the form.
- Do provide complete information in all required sections, including both the Provider and LDSS sections.
- Do attach a copy of the DMAS-96 form to the DMAS 225 when the patient is first admitted to care.
- Do check all appropriate boxes to ensure nothing is overlooked.
- Don't share the source of the member’s income anywhere on the form.
- Don't forget to send a copy of the memo to DMAS if the member is ineligible due to a penalty period.
- Don't neglect to include the member’s residential address if it differs from the address on the form.
- Don't skip the process of documenting any changes in a patient’s circumstances that may affect eligibility.
Misconceptions
Understanding the DMAS 225 form can be challenging, leading to various misconceptions. Here are some common misunderstandings about this important document:
- The DMAS 225 form is only for nursing homes. This form is used in various settings, including community-based care facilities and long-term care services, making it applicable beyond just nursing homes.
- Only the provider needs to fill out the DMAS 225 form. Both the local Department of Social Services (LDSS) and the provider of care must complete relevant sections to ensure accurate communication and exchange of information.
- Once submitted, the DMAS 225 form never needs to be updated. This form must be revised anytime there is a change in the patient's status or circumstances, such as discharge or modifications in income.
- The DMAS 225 form is not legally required. Accurate completion and submission of the form is crucial for compliance with Medicaid regulations and to ensure that patients receive the correct benefits.
- There is no need to attach additional documents. When a patient is first admitted, it is necessary to attach the DMAS-96 form to the DMAS 225 form to provide complete information.
- Patients can directly submit the DMAS 225 form. Patients cannot submit this form themselves. It must be initiated by either the LDSS or the provider to maintain proper channels of communication.
- All copies of the DMAS 225 form are sent to the same place. Different copies of the form must be sent to various recipients depending on whether the patient is in nursing facilities or community-based care.
- General information is sufficient to complete the DMAS 225 form. Specific and detailed information about the patient's status, eligibility, and any changes must be provided to ensure accurate processing.
- Confidential information is always appropriate to share. The source of the member’s income should not be disclosed on the DMAS 225 form, highlighting the importance of privacy regulations.
It is crucial for providers and LDSS officials to understand these points clearly. Misinterpretations can lead to delays in care or improper handling of Medicaid services, making it imperative to communicate accurately and efficiently.
Key takeaways
Here are key takeaways for filling out and utilizing the DMAS 225 form:
- Purpose: The DMAS 225 form is essential for sharing information between the local Department of Social Services (LDSS) and nursing facilities or Community-Based Care (CBC) Waiver Providers.
- Eligibility Status: The form allows for the communication of the Medicaid eligibility status of a patient/member.
- Changes in Care: It is used to report changes in the patient/member's level of care.
- Documentation Required: Providers must document admission dates, request eligibility status, and notify the LDSS of any significant changes in the patient's circumstances.
- Form Completion Requirement: Whenever there is a change in the member’s situation that affects eligibility, a new form must be prepared.
- Copy Distribution: Send the original form to the relevant facility and keep necessary copies for distribution to other appropriate parties, including case managers.
- Use of Additional Documents: Attach a copy of the DMAS-96 when the patient first enters care.
- FIPS Code: Waiver providers must provide the Member FIPS code, especially if the residential address differs from the one on the form.
- Handling Ineligibility: If a member is deemed ineligible for Medicaid long-term care due to a penalty period, notify DMAS with the appropriate documentation.
- Compliance with Instructions: Complete the appropriate sections within the form accurately, avoiding the provision of income sources for members.
Browse Other Templates
Communication With Staff - This form is an important part of maintaining a safe work environment.
Can I Sue a State - Documenting your experience is vital for legal processes.
Texas Sales Tax Id - City driving requires three hours of practice to build decision-making skills.