Fill Out Your Dms 640 Form
The DMS 640 form serves as a critical tool for facilitating access to essential therapy services—specifically Occupational, Physical, and Speech Therapy—for Medicaid-eligible beneficiaries under the age of 21 in Arkansas. This form is primarily used by primary care physicians (PCPs) or attending physicians to issue referrals for therapy evaluations and to prescribe medically necessary services. It requires the physician to indicate the type of therapy needed, whether it be OT, PT, or ST, and to provide relevant patient information, including the child's Medicaid ID number, the last date seen in the office, and a diagnosis that justifies the need for therapy. Additionally, the form establishes a routine for the therapeutic process, requiring renewals of referrals every six months to ensure compliance with state regulations. The physician must meticulously complete various sections of the form, including details regarding treatment duration and frequency, thus enhancing the transparency of the treatment plan. In moments when therapy is deemed unnecessary, the appropriate box must be checked. Beyond its practical use, the data collected through the DMS 640 regarding therapy expenditures and beneficiary statistics helps shape policies and resources allocated for these essential services. The completed form must be kept in both the child's medical records and by the therapy provider, ensuring organized and accessible documentation of a child's therapeutic history within the Medicaid framework.
Dms 640 Example
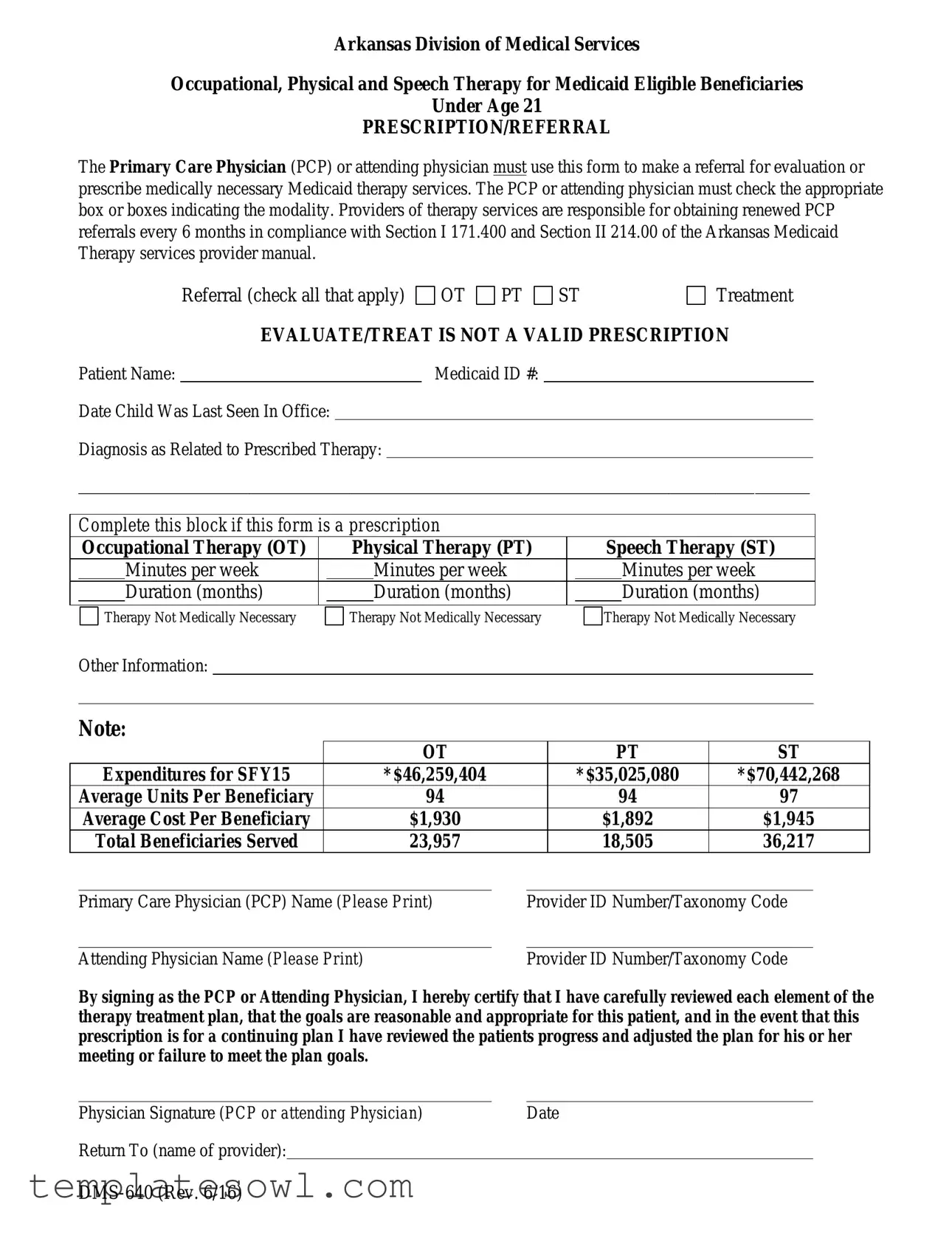
Arkansas Division of Medical Services
Occupational, Physical and Speech Therapy for Medicaid Eligible Beneficiaries
Under Age 21
PRESCRIPTION/REFERRAL
The Primary Care Physician (PCP) or attending physician must use this form to make a referral for evaluation or prescribe medically necessary Medicaid therapy services. The PCP or attending physician must check the appropriate box or boxes indicating the modality. Providers of therapy services are responsible for obtaining renewed PCP referrals every 6 months in compliance with Section I 171.400 and Section II 214.00 of the Arkansas Medicaid Therapy services provider manual.
Referral (check all that apply)  OT
OT 
 PT
PT  ST
ST
Treatment
EVALUATE/TREAT IS NOT A VALID PRESCRIPTION
Patient Name: |
|
Medicaid ID #: |
Date Child Was Last Seen In Office:
Diagnosis as Related to Prescribed Therapy:
______________________________________________________________________________________________
Complete this block if this form is a prescription
|
Occupational Therapy (OT) |
|
Physical Therapy (PT) |
|
Speech Therapy (ST) |
|||
|
|
Minutes per week |
|
|
Minutes per week |
|
|
Minutes per week |
|
|
|
|
|
|
|
|
|
|
|
Duration (months) |
|
|
Duration (months) |
|
|
Duration (months) |
|
|
|
|
|
|
|
|
|
Therapy Not Medically Necessary
Therapy Not Medically Necessary
Therapy Not Medically Necessary
Other Information:
Note:
|
|
|
OT |
|
|
PT |
ST |
|
|
Expenditures for SFY15 |
|
*$46,259,404 |
|
|
*$35,025,080 |
*$70,442,268 |
|
|
Average Units Per Beneficiary |
|
94 |
|
|
94 |
97 |
|
|
Average Cost Per Beneficiary |
|
$1,930 |
|
|
$1,892 |
$1,945 |
|
|
Total Beneficiaries Served |
|
23,957 |
|
|
18,505 |
36,217 |
|
|
|
|
|
|
||||
|
Primary Care Physician (PCP) Name (Please Print) |
|
Provider ID Number/Taxonomy Code |
|||||
|
|
|
|
|
|
|||
|
Attending Physician Name (Please Print) |
|
|
Provider ID Number/Taxonomy Code |
||||
By signing as the PCP or Attending Physician, I hereby certify that I have carefully reviewed each element of the therapy treatment plan, that the goals are reasonable and appropriate for this patient, and in the event that this prescription is for a continuing plan I have reviewed the patients progress and adjusted the plan for his or her meeting or failure to meet the plan goals.
Physician Signature (PCP or attending Physician) |
Date |
Return To (name of provider):
Instructions for Completion
Form
If
Patient Name – Enter the patient’s full name.
Medicaid ID # – Enter the patient’s Medicaid ID number.
Return To – To be completed by requesting provider to include therapy provider/address/fax/secure email.
Physician or Physician’s office staff must complete the following:
Date Child Was Last Seen In Office – Enter the date of the last time you saw this child. (This could be either for a complete physical examination, a routine
Diagnosis as Related to Prescribed Therapy – Enter the diagnosis that indicates or establishes medical necessity for prescribed therapy.
Prescription block – If the form is used for a prescription, enter the prescribed number of minutes per week and the prescribed duration (in months) of therapy.
If therapy is not medically necessary at this time, check the box.
Other Information – Any other information pertinent to the child’s medical condition, plan of treatment, etc., may be entered.
Primary Care Physician (PCP) Name and Provider ID Number and/or Taxonomy Code – Print the name of the prescribing PCP and his or her provider identification number and/or taxonomy code.
Attending Physician Name and Provider ID Number and/or Taxonomy Code – If the Medicaid- eligible child is exempt from PCP requirements, print the name of the prescribing attending physician and his or her provider identification number and/or taxonomy code.
Physician Signature and Date – The prescribing physician must sign and date the prescription for therapy in his or her original signature.
Arkansas Medicaid’s criteria for electronic signatures as stated in Arkansas Code
When an electronic version of the DMS 640 becomes part of the physician/ or providers’ electronic health record, the inclusion of extraneous patient and clinic information does not alter the form.
*These therapy amounts include therapy provided in a Developmental Day Treatment Center (DDTCS)
The original of the completed form
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose | The DMS-640 form is used for referrals and prescriptions for occupational, physical, and speech therapy services for Medicaid-eligible children under 21 in Arkansas. |
| Origin of the Form | This form is issued by the Arkansas Division of Medical Services. |
| Requirement for Physicians | Primary Care Physicians (PCPs) or attending physicians must complete the form for therapy referrals and prescriptions, ensuring compliance with state Medicaid regulations. |
| Renewals | PCPs are responsible for obtaining renewed referrals every six months. |
| Legal Compliance | Section I 171.400 and Section II 214.00 of the Arkansas Medicaid Therapy Services Provider Manual govern the use of this form. |
| Patient Information | The form requires essential patient information, including the child’s name, Medicaid ID number, last visit date, and a diagnosis relevant to the therapy. |
| Signature Requirement | Prescribing physicians must sign and date the form, certifying their review of the therapy treatment plan. |
| Electronic Signature Compliance | The form must meet Arkansas Medicaid's criteria for electronic signatures as indicated in Arkansas Code 25-31-103. |
Guidelines on Utilizing Dms 640
Completing the DMS 640 form is crucial for facilitating necessary therapy services for eligible Medicaid beneficiaries under the age of 21. The process must be done accurately to ensure timely referrals and prescriptions for services. Follow these steps carefully to fill out the form correctly.
- Check Referral Type: Indicate the therapy type that you are referring for evaluation (Occupational Therapy, Physical Therapy, or Speech Therapy) by checking the appropriate box.
- Patient Information: Enter the patient's full name and Medicaid ID number in the designated fields.
- Date of Last Visit: Fill in the date when the child was last seen in your office.
- Diagnosis: Provide the diagnosis related to the prescribed therapy that establishes medical necessity.
- Prescription Block: If applicable, record the number of minutes per week and the duration (in months) for each type of therapy being prescribed.
- Medical Necessity: If therapy is deemed not medically necessary, check the corresponding box.
- Additional Information: Enter any relevant notes pertaining to the child's condition or treatment plan in the designated area.
- Physician Names: Print the primary care physician's name along with their provider ID number and/or taxonomy code. If applicable, also print the attending physician's name and their provider ID/taxonomy code.
- Signature and Date: The prescribing physician must sign and date the form, ensuring compliance with electronic signature criteria.
- Return Information: Provide the name of the provider, including therapy provider's address, fax, or secure email for sending the form back.
- Record Keeping: Maintain the original completed form in the child's medical records and ensure a copy is kept by the therapy provider.
What You Should Know About This Form
What is the purpose of the DMS 640 form?
The DMS 640 form is used by primary care physicians (PCPs) or attending physicians to refer Medicaid-eligible beneficiaries under the age of 21 for occupational, physical, or speech therapy. It serves to prescribe medically necessary therapy services and facilitates communication between the physician and the therapy provider.
Who needs to complete the DMS 640 form?
The form must be completed by the primary care physician or attending physician. This includes providing essential information about the patient, such as diagnosis and therapy prescription, along with the physician's signature to certify the information provided is accurate and appropriate for the patient’s needs.
How often do therapy providers need to renew referrals?
Therapy providers are responsible for obtaining renewed referrals from the PCP every six months. This requirement ensures that therapy services are consistently reevaluated for medical necessity based on the child’s ongoing progress and treatment needs.
What information is required on the DMS 640 form?
The form requires specific details, including the patient’s full name, Medicaid ID number, the date the child was last seen in the office, the diagnosis related to the prescribed therapy, and the therapy modalities being requested. Additionally, it asks for the prescribed therapy minutes per week and duration in months, as well as the names and provider ID numbers of the prescribing physician and attending physician (if applicable).
Can the DMS 640 form be used for multiple therapies?
Yes, the DMS 640 form allows physicians to check multiple therapy modalities if the referral or prescription is for several types of therapy (occupational, physical, or speech). This flexibility accommodates the diverse needs of the patient.
What should I do if therapy is determined to be not medically necessary?
If therapy is identified as not medically necessary, the physician should check the appropriate box on the DMS 640 form indicating this status. This transparent communication helps manage treatment expectations and documents the decision-making process effectively.
How is the DMS 640 form submitted?
The completed DMS 640 form should be returned to the specified therapy provider. The physician should maintain the original form in the patient’s medical records, while the therapy provider retains a copy for their records. Proper documentation supports compliance with Medicaid requirements.
What if I use an electronic health record system?
When using an electronic health record (EHR) system, the DMS 640 form can be integrated with the patient’s electronic chart. It's important to ensure that it meets Arkansas Medicaid’s criteria for electronic signatures. If the EHR cannot accommodate electronic signatures, the form should be printed, signed, and dated by the physician, and a scanned copy should be stored in the system.
Are there any requirements for the physician's signature on the DMS 640 form?
The prescribing physician must sign the DMS 640 form in their original signature. This certification confirms that the physician has reviewed the treatment plan and goals for the patient. Compliance with Arkansas’s electronic signature laws is also essential if the form is processed electronically.
Common mistakes
One common mistake is failing to check the correct boxes for the type of therapy. It is essential to select the appropriate modality, whether it’s Occupational, Physical, or Speech Therapy. Skipping this step can result in delays or denials for services, as the form will not accurately represent the patient’s needs.
Another frequent oversight occurs when individuals forget to include the patient’s full name. Providing only a first name or an incomplete name can lead to confusion. This information needs to be clear and complete for accurate identification, especially since Medicaid cases can involve multiple children.
Some people neglect to fill in the Medicaid ID number. This number is crucial as it identifies the specific patient in the Medicaid system. An missing number might cause processing issues that could result in delayed therapy services.
There are instances where the date of the child’s last visit is not included. This date is important as it reflects the most recent medical evaluation. Without it, the therapy provider may not have a complete understanding of the child's current condition.
Including a clear medical diagnosis related to the prescribed therapy is another area where mistakes often happen. If no diagnosis is provided, it can hinder the approval process. Therapies need a valid medical reason tied to the child’s condition to be deemed necessary by Medicaid.
Moreover, some individuals mistakenly use the same DMS-640 form for making a referral and prescribing therapy. This is not allowed. A separate form is required for a prescription once the evaluation results indicate the need for therapy. Confusion here can lead to administrative complications.
Lastly, forgetting signatures or the date from the physician can stall the process. The form must have the prescribing physician’s original signature and date to be valid. Without this, the form may be rejected, and the required services may not commence on time.
Documents used along the form
The DMS 640 form serves as a key document for prescribing and referring therapy services for Medicaid eligible beneficiaries under 21 in Arkansas. However, there are other forms and documents that can accompany the DMS 640 to ensure a smooth process. Below is a list of these related documents along with a brief description of each.
- Patient Medical History Form: This form captures the patient's medical history, including prior treatments, allergies, and relevant family medical history. It helps providers understand the patient's background and make informed decisions about treatment.
- Therapy Progress Notes: These notes are made by therapists to document the patient's progress during therapy sessions. They help track improvements and any necessary adjustments to the treatment plan.
- Insurance Authorization Form: This document is often required by insurance companies to approve coverage for therapy services. It provides details about the recommended treatment and the medical necessity behind it.
- Consent for Treatment Form: This form ensures that the patient or guardian agrees to the proposed therapy. It covers the risks, benefits, and any alternative treatments available, ensuring that informed consent is obtained.
- Medicaid Eligibility Verification: This form is used to confirm that the patient qualifies for Medicaid. It typically includes the patient’s ID number and personal details to verify eligibility before services are provided.
- Referral Continuation Form: If therapy needs to be extended, this form allows the PCP to continue the authorization for therapy services. It ensures that ongoing care complies with Medicaid regulations.
Having these documents in order can facilitate the therapy process and ensure compliance with Medicaid requirements. Each form plays a vital role in providing comprehensive care to children who need therapy services.
Similar forms
- Form DMS-645: This form is used for prescribing outpatient therapy services for pediatric patients. Similar to DMS-640, it requires physician signatures, patient identification, and specifies therapy needs for Medicaid-eligible beneficiaries.
- Form DMS-650: This document serves to authorize mental health services under Medicaid. Both forms need the physician’s assessment of medical necessity and include patient demographics and treatment details.
- Form DMS-160: Used to request prior authorization for a variety of medical services, this form shares the need for physician input and documentation of patient diagnosis, similar to DMS-640.
- Form DMS-680: This form is a referral for specialized medical care. Like DMS-640, it requires signature verification from the attending physician and specifies the patient’s medical condition.
- Form DMS-400: This document is used for Medicaid eligibility verification. It parallels DMS-640 by including patient identifiers and needs for accurate record-keeping by healthcare providers.
- Form DMS-810: This is a request for durable medical equipment. Both forms need healthcare provider input and the foundation of medical necessity for items or therapy services requested.
- Form DMS-930: Used for pediatric nursing services, this form also requires detailed information on patient conditions and the prescribing physician’s approval, mirroring the procedure followed in DMS-640.
Dos and Don'ts
When filling out the DMS-640 form, there are a few important things to keep in mind. Below are four key dos and don'ts to ensure everything goes smoothly:
- Do: Carefully check the appropriate boxes indicating the therapy modalities you are referring to, whether it's Occupational Therapy (OT), Physical Therapy (PT), or Speech Therapy (ST).
- Do: Fill in the patient's full name and Medicaid ID number accurately to avoid any confusion.
- Don't: Forget to include the date of the child's last office visit; this is essential information for evaluating medical necessity.
- Don't: Submit an incomplete form; make sure all required sections are filled out before finalizing.
Following these guidelines can help ensure that you submit an effective and accurate referral or prescription for therapy services. Properly completing the DMS-640 form is essential for the well-being of your patients and helps streamline the process of securing necessary medical services.
Misconceptions
When it comes to the DMS 640 form, misconceptions can lead to confusion about its use in therapy referrals and prescriptions for Medicaid eligible beneficiaries. Here’s a list of eight common misunderstandings along with clarifications to help clear them up.
- The DMS 640 form is only for initial therapy evaluations. Many believe this form can only be used to initiate evaluations. In reality, it can also be used to prescribe ongoing therapy after evaluating a patient.
- Only certain healthcare providers can complete the DMS 640. While primarily a tool for primary care physicians (PCPs) and attending physicians, other qualified providers may assist in filling it out as long as they are authorized and recognize the patient's needs.
- This form is optional for Medicaid therapy. Some assume that completing the DMS 640 is not mandatory. However, it is a required document to validate the need for therapy services under Medicaid guidelines.
- Referrals don't need to be renewed. Another misconception is about the renewal of referrals. Providers are responsible for renewing referrals every six months to comply with Arkansas Medicaid guidelines.
- Filling out the form is a straightforward process. Many find it confusing, but the DMS 640 has specific fields and instructions that need to be followed carefully to ensure proper submission and avoid delays in therapy services.
- Any physician's signature is sufficient. Some believe that any signature suffices, yet the signature must belong to the prescribing physician, meeting the criteria for verification in accordance with Arkansas law.
- All completed forms are treated the same. Each DMS 640 form must be stored appropriately. The original must be kept in the child's medical records, while a copy should be retained by the therapy provider.
- The DMS 640 does not require supporting information. In reality, physicians should provide additional context regarding the patient's condition and treatment plan beyond just filling out the basic information.
Understanding these points helps ensure that the DMS 640 form is used correctly, which ultimately benefits the beneficiaries and their access to necessary therapy services.
Key takeaways
Key takeaways for filling out and using the DMS-640 form:
- The DMS-640 form is essential for referrals and prescriptions regarding therapy services for Medicaid-eligible beneficiaries under the age of 21.
- The Primary Care Physician (PCP) or attending physician must complete the form to indicate the necessary therapy type, which includes Occupational Therapy (OT), Physical Therapy (PT), or Speech Therapy (ST).
- Each therapy service requires a renewed referral every six months, in accordance with Medicaid regulations.
- Patients must have their personal information, including their full name and Medicaid ID number, accurately filled in on the form.
- If the form is initially used for evaluation, a new DMS-640 must be submitted to prescribe therapy services after evaluation results are obtained.
- The prescribing physician must document the date the child was last seen in the office, establishing the continuity of care.
- It is vital to provide a clear diagnosis that justifies the medical necessity of the prescribed therapy.
- The form requires the physical signature of the PCP or attending physician, who must also include their provider ID number or taxonomy code.
- Retention of the completed form is mandatory; the original must be kept in the child's medical record, while a copy should be held by the therapy provider.
Browse Other Templates
2022 Tax Checklist - The costs of income-producing activities, such as certain hobbies, may offer potential deductions.
Application for Writ of Possession - This application is crucial for those needing urgent recovery of property.
Plumbing Work Order Template - Inspect plumbing system for leaks.