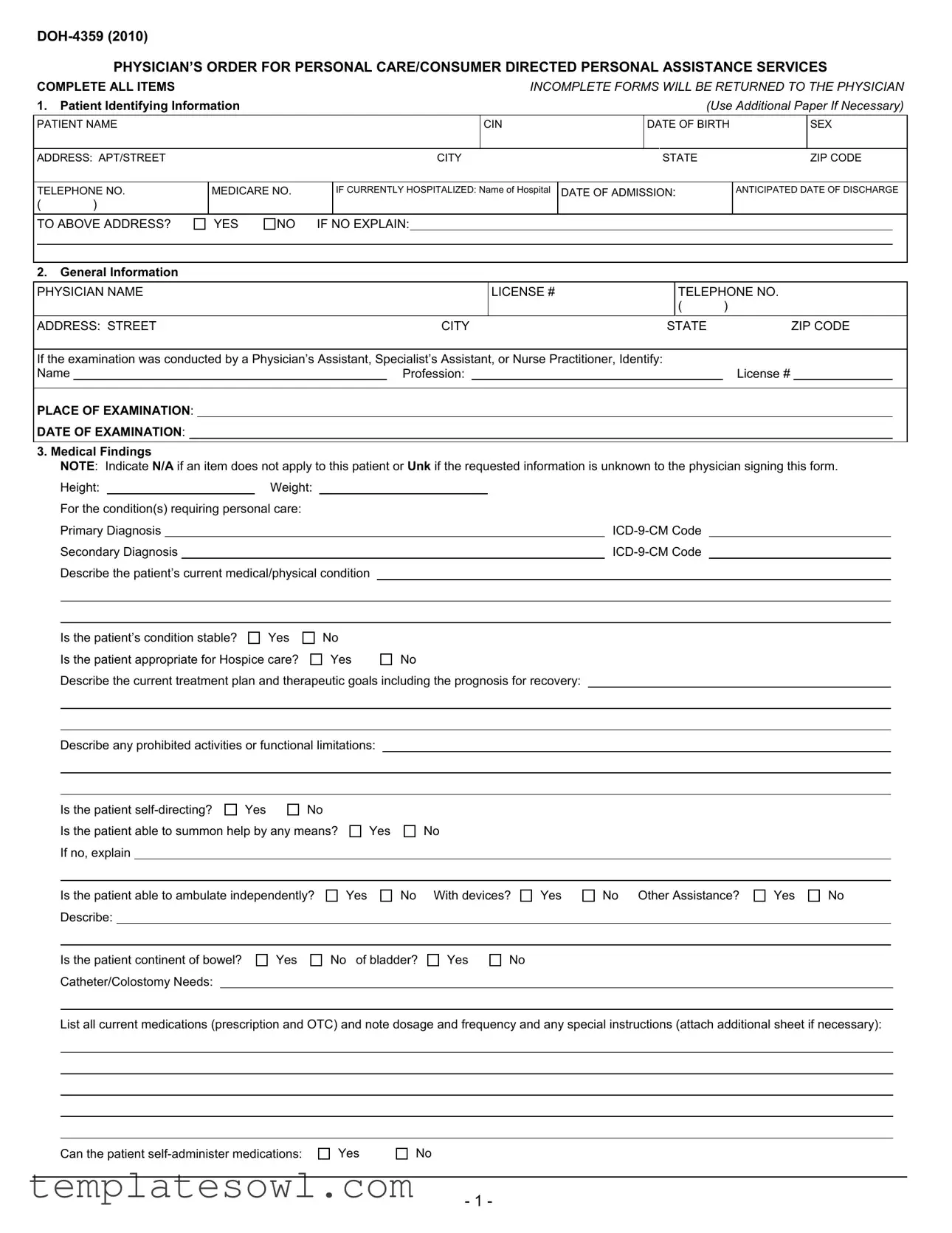
Fill Out Your Doh 4359 Form
The DOH-4359 form is an essential document designed for physicians to authorize personal care or consumer-directed personal assistance services for patients in need. It collects critical identifying information, including the patient's name, date of birth, and medical history, which helps ensure proper care. The document requires a physician’s detailed assessment of the patient’s condition, including their medical diagnoses and treatment plans. Evaluations of the patient’s physical capabilities, such as mobility and self-care abilities, are crucial components of the form. Additionally, the physician must provide insight into the patient's medication regimen, dietary restrictions, and any necessary assistance with daily activities. It is important to complete the form fully, as any missing information could cause delays in needed services. The signed order confirms that the patient can be cared for at home and complies with New York State Department of Health regulations, emphasizing the responsibility of the physician in accurately assessing and documenting the patient's needs.
Doh 4359 Example
PHYSICIAN’S ORDER FOR PERSONAL CARE/CONSUMER DIRECTED PERSONAL ASSISTANCE SERVICES
COMPLETE ALL ITEMS |
|
|
|
|
|
|
|
|
|
|
INCOMPLETE FORMS WILL BE RETURNED TO THE PHYSICIAN |
||||||||||||||||||||||
1. |
Patient Identifying Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(Use Additional Paper If Necessary) |
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
PATIENT NAME |
|
|
|
|
|
|
|
|
|
CIN |
|
|
|
DATE OF BIRTH |
|
|
SEX |
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ADDRESS: APT/STREET |
|
|
|
|
|
|
|
CITY |
|
|
|
STATE |
|
|
|
|
|
ZIP CODE |
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
TELEPHONE NO. |
MEDICARE NO. |
|
|
IF CURRENTLY HOSPITALIZED: Name of Hospital |
DATE OF ADMISSION: |
|
|
|
ANTICIPATED DATE OF DISCHARGE |
||||||||||||||||||||||||
( |
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
TO ABOVE ADDRESS? |
YES |
NO |
IF NO EXPLAIN: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. |
General Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
PHYSICIAN NAME |
|
|
|
|
|
|
|
|
|
|
LICENSE # |
|
|
|
|
TELEPHONE NO. |
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
( |
) |
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
ADDRESS: STREET |
|
|
|
|
|
|
|
CITY |
|
|
|
STATE |
ZIP CODE |
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
If the examination was conducted by a Physician’s Assistant, Specialist’s Assistant, or Nurse Practitioner, Identify: |
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||
Name |
|
|
|
|
|
|
|
Profession: |
|
|
|
|
|
|
|
|
|
License # |
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
PLACE OF EXAMINATION: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
DATE OF EXAMINATION: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
3. Medical Findings |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
NOTE: Indicate N/A if an item does not apply to this patient or Unk if the requested information is unknown to the physician signing this form. |
|||||||||||||||||||||||||||||||
|
|
Height: |
|
|
Weight: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
For the condition(s) requiring personal care: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
Primary Diagnosis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
Secondary Diagnosis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
Describe the patient’s current medical/physical condition |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
Is the patient’s condition stable? |
Yes |
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
Is the patient appropriate for Hospice care? |
|
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
Describe the current treatment plan and therapeutic goals including the prognosis for recovery: |
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
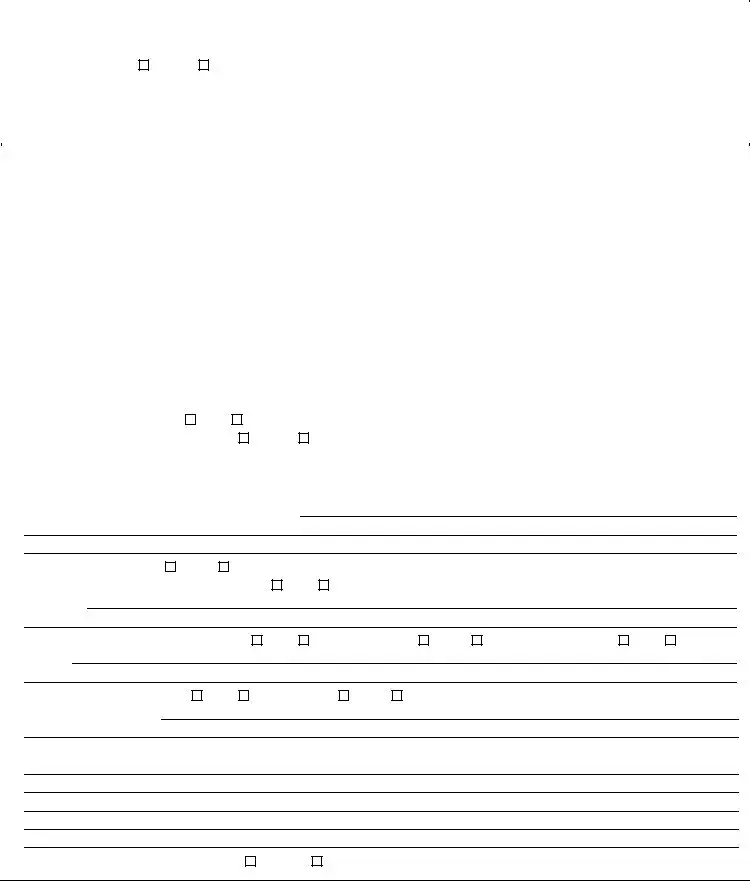
Describe any prohibited activities or functional limitations:
Is the patient |
Yes |
No |
Is the patient able to summon help by any means? If no, explain
Yes
No
Is the patient able to ambulate independently? Describe:
Yes
No With devices?
Yes
No Other Assistance?
Yes
No
Is the patient continent of bowel? Catheter/Colostomy Needs:
Yes
No of bladder?
Yes
No
List all current medications (prescription and OTC) and note dosage and frequency and any special instructions (attach additional sheet if necessary):
Can the patient
Yes
No
- 1 -
If the patient requires a modified diet or has other special nutritional or dietary needs, describe:
Please indicate any task, treatments or therapies currently received, or required by the patient:
Does the patient require assistance with, or provision of, skilled tasks (e.g. monitoring of vital signs, dressing changes, glucose monitoring, etc.)?
Yes
No
If Yes, please indicate:
Based on the medical condition, do you recommend the provision of service to assist with skilled tasks, personal care and/or light housekeeping tasks?
Yes
No
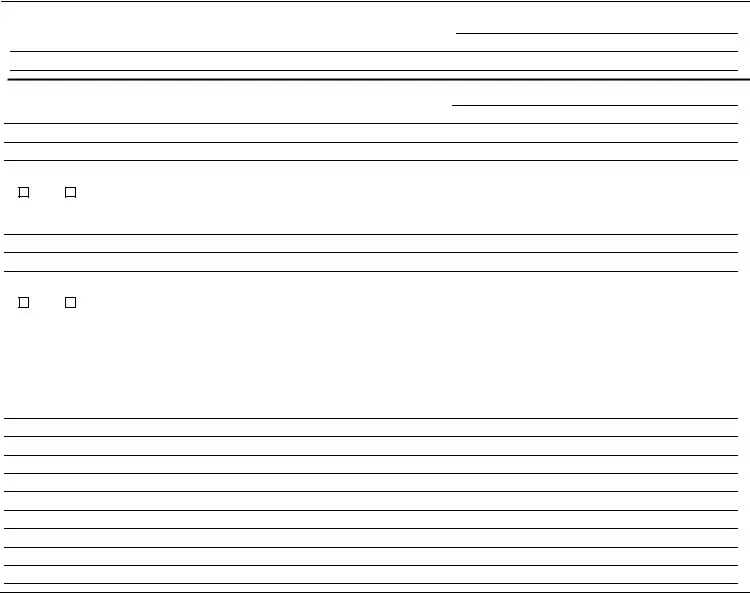
Contributing Factors:
Describe contributing factors including but not limited to the social, family, home or medical (e.g. muscular/motor impairments, poor range of motion,
decreased stamina, etc.) situation that may affect the patient’s ability to function, or may affect the need for home care or that may affect the patient's need
for assistance with skilled tasks, personal care tasks and/or light housekeeping. Please include any other information that may be pertinent to the need for
assistance with home care services.
IT IS MY OPINION THAT THIS PATIENT CAN BE CARED FOR AT HOME. I HAVE ACCURATELY DESCRIBED HIS OR HER MEDICAL CONDITION. NEEDS AND REGIMENS, INCLUDING ANY MEDICATION REGIMENS, AT THE TIME I EXAMINED HIM OR HER. I UNDERSTAND THAT I AM NOT TO RECOMMEND THE NUMBER OF HOURS OF PERSONAL CARE SERVICES THIS PATIENT MAY REQUIRE. I ALSO UNDERSTAND THAT THIS PHYSI- CIAN'S ORDER IS SUBJECT TO THE NEW YORK STATE DEPARTMENT OF HEALTH REGULATIONS AT PARTS 515, 516, 517 AND 518 OF TITLE 18 NYCRR, WHICH PERMIT THE DEPARTMENT TO IMPOSE MONETARY PENALTIES ON, OR SANCTION AND RECOVER OVERPAYMENTS FROM, PROVIDERS OR PRESCRIBERS OF MEDICAL CARE, SERVICES OR SUPPLIES WHEN MEDICAL CARE, SERVICES OR SUPPLIES THAT ARE UNNECESSARY, IMPROPER OR EXCEED THE PATIENT’S DOCUMENTED MEDICAL CONDITION ARE PROVIDED OR ORDERED.
INCOMPLETE OR MISSING INFORMATION MAY DELAY SERVICES TO THIS PATIENT
Physician’s Signature _________________________________________________________________ Date _________________________
PLEASE SIGN AND RETURN COMPLETED FORM WITHIN 30 CALENDAR DAYS OF EXAMINATION TO:
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
New York State Department of Health
- 2 -
PHYSICIAN’S ORDER FOR PERSONAL CARE/CONSUMER DIRECTED PERSONAL ASSISTANCE SERVICES
INSTRUCTIONS
COMPLETE ALL ITEMS. (Attach additional sheets, if necessary). INCOMPLETE FORMS WILL BE RETURNED TO THE PHYSICIAN.
INCOMPLETE OR MISSING INFORMATION MAY DELAY SERVICES TO THIS PATIENT.
1.Patient Identifying Information
•Patient Name. Enter the patient’s name.
•CIN. Found on the patient’s Medical Assistance ID card.
•Date of Birth. Enter the patient’s date of birth.
•Sex. Enter the patient’s gender.
•Address and telephone number. Enter the patient’s address and telephone number.
•Medicare #. Enter the patient’s Medicare number if available.
•If currently hospitalized. If the patient is hospitalized at the time of completion of the physician's order, indicate the name of the hospital, date of admission, and anticipated date of discharge.
•Discharge to above address. If the patient is to be discharged to an address other than the address listed above please explain.
•General Information
Physician’s Name, License #, Address, Telephone. Enter information for the physician signing the order. Enter either the physician’s license number as issued by the New York State Department of Education or the provider billing number issued by the New York State Department of Health Medicaid Management Information System.
•Examination conducted by other than a physician. If patient was examined, and the order form completed by a physician’s assistant, specialist’s assistant, or nurse practitioner, complete the required information.
•Place of Examination. Indicate the location (office, clinic, home, etc) of the examination of the patient.
•Date of Examination. Enter the date the patient was examined. This must be within 30 days of the date the physician signed the form.
3.Medical Findings
Note: Indicate N/A if an item does not apply to this patient or Unk if the requested information is unknown to the physician signing this form.
•Height, Weight. Enter the patient’s height and weight.
•Primary and Secondary Diagnosis. Enter the primary and secondary diagnosis with
•Describes the current condition. Describe the patient’s current medical/physical condition, including any relevant history.
•Stability. Check Yes if the patient’s condition is not expected to show marked deterioration or improvement. A stable medical condition shall be defined as follows:
(a)the condition is not expected to exhibit sudden deterioration or improvement; and
(b)the condition does not require frequent medical or nursing judgment to determine changes in the patient's plan of care; and
(c)(1) the condition is such that a physically disabled individual is in need of routine supportive assistance and does not need skilled professional care in the home; or
(2)the condition is such that a physically disabled or frail elderly individual does not need professional care but does require assistance in the home to prevent a health or safety crisis from developing.
•Hospice. If the patient’s condition is terminal, indicate if the patient is appropriate for Hospice services.
•Describe the current treatment plan. Include therapeutic goals and prognosis for recovery and anticipated duration of the current treatment plan.
•Limitations. Indicate any functional limitations or prohibited activities.
•
•Able to Summon Help. Check Yes if the patient is able to summon assistance in an emergency situation by any means. If the patient is not able to summon assistance, check No and explain.
-3 -
•Ambulation. Indicate the patient’s ability to ambulate independently, or with the need for assistance or devices. Specify assistance/devices used or needed.
•Bowel/Bladder. Indicate if the patient is continent. Describe any catheter or colostomy needs.
•Medications Required. List all prescription and
•Medication Administration. Indicate the patient’s ability to
•Dietary Needs. Indicate if the patient has special nutritional or dietary needs, i.e. low salt or high potassium.
•Tasks/Treatments/Therapies. Indicate any tasks, treatments or therapies which the patient receives or requires in the home and describe.
•Need for completion/assistance with skilled tasks. If the patient requires assistance with skilled tasks including, but not limited to, glucose monitoring, wound care, vital signs, describe the need for such assistance.
•Recommendation to provide assistance. Check Yes if, in your opinion, the patient can be maintained in his or her home with provision of home care services.
•Contributing factors to need for assistance. Please indicate the functional deficits that support the need for the provision of home care services. Please include any pertinent information you may have regarding the patient’s surroundings, physical condition or other factors that may affect the ability of the patient to function in the community or the patient’s need for assistance with personal care tasks.
4.Physician’s Signature/Date of completion. The signature of the ordering physician as identified in Item 2. Note that by signing this document, the physician certifies that the patient’s condition and needs are accurately described. Forms lacking a signature and/or date are not acceptable.
5.Return Form To. The local district or other case management entity to whom the form is to be returned.
- 4 -
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Title | DOH-4359: Physician’s Order for Personal Care/Consumer Directed Personal Assistance Services |
| Purpose | This form is used to authorize personal care services for patients requiring assistance at home. |
| Completeness Requirement | All items must be completed. Incomplete forms will be returned to the physician. |
| Governing Law | Regulations under Title 18 NYCRR, Parts 515, 516, 517, and 518, govern this form in New York State. |
| Signature Requirement | The form must be signed and dated by the physician who examined the patient. |
| Patient Stability Assessment | The physician must indicate whether the patient's condition is stable, which informs the need for care. |
| Submission Timeline | The completed form must be returned to the appropriate local district within 30 calendar days of the examination date. |
Guidelines on Utilizing Doh 4359
The DOH-4359 form must be completed accurately for timely processing of personal care services. Follow these detailed steps to ensure all required information is included.
- Enter the patient's identifying information:
- Patient Name
- CIN (from the patient’s Medical Assistance ID card)
- Date of Birth
- Sex
- Address and Telephone Number
- Medicare Number (if applicable)
- If the patient is hospitalized:
- Indicate the hospital's name
- Provide the date of admission
- Enter the anticipated date of discharge
- If the discharge is to an address other than the listed one, provide an explanation
- Fill in the general information:
- Physician’s Name, License Number, Address, and Telephone Number
- If applicable, provide information for the Physician's Assistant, Specialist's Assistant, or Nurse Practitioner
- Indicate the place and date of examination
- Complete the medical findings section:
- Enter the patient's height and weight
- List primary and secondary diagnoses with ICD-9-CM codes
- Describe the patient’s current medical/physical condition
- Indicate if the condition is stable and if the patient is appropriate for Hospice care
- Detail the current treatment plan, limits, and patient’s ability to self-direct
- Identify if the patient can summon help and describe ambulation ability
- Note bowel and bladder continence and any catheter/colostomy needs
- List all medications, including dosage and frequency
- Indicate if the patient can self-administer medications
- If applicable, describe any dietary needs and pertinent tasks or therapies required
- Answer questions regarding the need for assistance with skilled tasks and provide a recommendation for home care services based on the medical condition.
- Describe any contributing factors affecting the patient's need for assistance.
- Sign and date the form, certifying that the patient's condition and needs are accurately described.
- Return the completed form within 30 days to the appropriate local district or case management entity.
What You Should Know About This Form
What is the purpose of the DOH-4359 form?
The DOH-4359 form, titled "Physician’s Order for Personal Care/Consumer Directed Personal Assistance Services," is primarily used to document the medical necessity for personal care services. Physicians complete the form to communicate the patient’s medical condition, treatment needs, and eligibility for receiving home care services. This ensures that patients receive appropriate assistance based on their specific health requirements.
Who is required to fill out the DOH-4359 form?
The form must be completed by a licensed physician. If a physician’s assistant, specialist’s assistant, or nurse practitioner conducts the examination, that individual's information also needs to be documented. The physician's signature certifies the accuracy of the information provided regarding the patient's medical condition and care needs.
What information is needed in the Patient Identifying Information section?
This section requires essential details about the patient, including name, date of birth, gender, address, phone number, and Medicare number if applicable. If the patient is currently hospitalized, the physician must include the hospital's name, admission date, and anticipated discharge date. This information ensures accurate identification and facilitates the provision of services.
What type of medical findings must be reported on the form?
Physicians must document pertinent medical findings, including height, weight, primary and secondary diagnoses, and any functional limitations the patient may experience. It is also crucial to state whether the patient’s condition is stable and to provide information on current medications, treatment plans, and any dietary restrictions. This comprehensive medical history helps assess the need for personal care services.
How can incomplete forms affect patient care?
Incomplete forms can lead to significant delays in the provision of necessary services to patients. If any required information is missing, the form will be returned to the physician for correction. Timeliness is critical; therefore, ensuring that all relevant sections are fully completed is essential for facilitating efficient patient care.
What is the role of the physician regarding hours of service recommended on the form?
Physicians are specifically instructed not to recommend the number of hours of personal care services a patient may require. Instead, they must focus on accurately describing the patient’s medical condition and needs. The determination of service hours is addressed separately by the appropriate authorities based on the provided medical information.
Where should the completed DOH-4359 form be sent?
Once the form is completed and signed, it must be returned to the designated local district or case management entity. Prompt submission is important, as it directly influences the pace at which the patient can begin receiving the necessary home care services. Adhering to the 30-day submission guideline following the examination date is essential to avoid delays.
Common mistakes
When completing the DOH 4359 form, many people make common mistakes that can lead to delays in service or confusion about the patient's needs. One major error involves providing incomplete patient identifying information. Every field, from the patient's name to their address and telephone number, must be filled out accurately. Omitting any detail, such as the patient's Medicare number or even a telephone number, can cause unnecessary setbacks.
Another frequent mistake is neglecting to include all relevant medical findings. Be sure to specify both the primary and secondary diagnoses, including their corresponding ICD-9-CM codes. Not properly documenting these diagnoses can lead to misunderstandings about the patient’s condition, which may affect the type of care they receive.
Inconsistent information regarding the patient's current treatment plan is also a common issue. Describe the treatment thoroughly, articulating therapeutic goals and expected recovery times. If this section is vague or incomplete, it may result in delays as the health department seeks clarification.
People often forget to indicate if the patient is self-directing, which is critical. If the patient can make decisions regarding their care, it should be noted. This detail impacts the level of assistance they receive. Also, failure to clearly state whether the patient can summon help in emergencies can lead to serious safety risks.
Providing insufficient details about medications is another misstep. Each medication, whether prescription or over-the-counter, should be listed with specific dosage instructions. If there are any special instructions or if the patient cannot self-administer, this information should be clearly documented.
Some individuals mistakenly think they can indicate contributing factors in a vague manner. Instead, specific details about the patient’s home environment, social situation, and any physical limitations should be included. This information is vital for understanding the patient's need for assistance and ensuring they receive the appropriate services.
Finally, people often fail to sign and date the form. It is crucial for the physician completing the DOH 4359 to provide their signature and the date of completion. Without these, the form may be considered invalid, significantly delaying the patient's access to necessary services.
Documents used along the form
The DOH-4359 form, known as the Physician’s Order for Personal Care/Consumer Directed Personal Assistance Services, plays a crucial role in ensuring patients receive the appropriate home care they need. Alongside this form, several other documents often complement the process of securing personal care services. Each of these documents provides essential information that helps authorities make informed decisions regarding a patient's care and treatment. Below is a list of several forms that are commonly used in conjunction with the DOH-4359 form.
- DOH-7011: Application for Home and Community-Based Services - This form captures the patient's eligibility and specific needs for home and community-based services. It provides detailed information about the individual’s medical history and living situation, ensuring that the right type and level of care are provided.
- DOH-5055: Personal Care Service Assessment Form - This document evaluates a patient’s current condition, needs, and the availability of support from family or community resources. It assists health care providers in determining the appropriate services that can be offered.
- DOH-4358: Case Management Plan - The Case Management Plan details the care strategies for a patient, outlining goals, interventions, and resources required to enhance the patient's care. It serves as a vital overview of the services needed and how they will be coordinated.
- Medicaid Application Form - This application form is necessary for patients seeking Medicaid coverage for home care services. It captures income, asset details, and other financial information, which helps determine eligibility for assistance.
- Health Insurance Portability and Accountability Act (HIPAA) Release Form - This form grants permission for healthcare providers to share relevant medical information. It is vital for coordinating care among various providers involved in the patient’s treatment plan.
- Patient Care Plan - The Patient Care Plan outlines day-to-day care procedures and specific medical interventions required for the patient. It helps caregivers understand their responsibilities and provides a clear guide for monitoring the patient’s progress.
These documents serve not only to streamline the process of securing personal care services but also to ensure that patients receive tailored and comprehensive support. Having all necessary forms completed accurately helps to facilitate timely and efficient care for patients in need. Each document contributes to a larger picture, allowing healthcare providers to deliver the best possible services.
Similar forms
-
Form CMS-485 (Home Health Certifications and Plan of Care): This document outlines the home health services that a patient will receive, similar to how the DOH 4359 specifies personal care services. Both require detailed medical histories and diagnoses to ensure the correct services are funded and provided.
-
Form 485.99.90 (Illinois Home Services Application): Like the DOH 4359, this document collects extensive patient information to determine eligibility for home services. It also requires details about medications and specific service needs.
-
Form 4505 (Personal Care Attendant (PCA) Assessment): This assessment gathers comprehensive patient details and specifies the type of personal care services needed, mirroring the information collected in the DOH 4359 for service determination.
-
Form HCA 1 (Home Care Aide Services Authorization): This form is similar to the DOH 4359 as it provides an official record of the patient's need for home assistance, including specific medical conditions and requested services.
-
Form 101 (Personal Care Services Assessment in Family Care): This assessment documents the patient's conditions, current care needs, and social determinants, akin to the DOH 4359's comprehensive approach to determining care requirements.
-
Form 122 (Assisted Living Facility Resident Assessment): This document evaluates the health status and care needs of residents. Its structured questions about medical conditions and care preferences align closely with those in DOH 4359.
-
Form 2580 (Skilled Nursing Facility Admission Assessment): Similar to the DOH 4359, this form assesses a patient's medical condition upon entry into a skilled nursing facility, gathering vital information on diagnoses and care needed.
-
Form 3824 (Long-Term Care Services Needs Assessment): This assessment assesses the long-term care needs of an individual, similar to how the DOH 4359 identifies personal care requirements for those needing assistance at home.
Dos and Don'ts
When filling out the DOH-4359 form, there are several important practices to follow. Here’s a list of things you should and shouldn’t do:
- Do complete all items on the form to avoid delays in processing.
- Do provide accurate patient identifying information including the patient's name, date of birth, and Medicare number if available.
- Do include any additional sheets necessary for explaining the patient's condition or needs.
- Do indicate if a patient has special dietary needs or is receiving particular therapies.
- Do ensure the form is signed and dated by the physician to validate the information provided.
- Don't leave any fields blank, as incomplete forms may be returned.
- Don't make assumptions about the patient's condition; every detail should be based on the latest assessment.
Following these guidelines will help streamline the process and ensure that the patient's needs are met promptly.
Misconceptions
- Misconception 1: The DOH 4359 form is optional. Many people believe that this form is optional for patients needing personal assistance services. In reality, completing the DOH 4359 is essential for ensuring that patients receive the necessary home care services.
- Misconception 2: The physician must recommend specific hours of care on the form. Some individuals think that physicians are required to specify the number of hours of care a patient requires. However, the form explicitly states that the physician should not recommend the number of hours needed.
- Misconception 3: Incomplete forms will still be accepted. There is a common belief that incomplete forms will not significantly delay care services. Unfortunately, it is critical to fill out all sections of the form, as missing information can lead to delays in processing and services.
- Misconception 4: The form is only for elderly patients. Many assume that the DOH 4359 is exclusively for older adults. In fact, this form is for any patient who requires personal care services, regardless of age.
- Misconception 5: The physician’s signature is not crucial. Some people may think that the physician’s signature is a formality and can be overlooked. In truth, the form requires the physician's signature to be valid; without it, the form cannot be processed.
- Misconception 6: Only physicians can complete this form. There is a misunderstanding that only physicians can complete the DOH 4359. While physicians traditionally fill out the form, qualified healthcare professionals like physician assistants or nurse practitioners can also complete it under certain circumstances.
- Misconception 7: The form has no impact on insurance coverage. Some individuals may believe that completing the DOH 4359 does not affect insurance claims. However, this form plays a pivotal role in documenting the need for services, which can, in turn, affect approval and reimbursement from insurance companies.
Key takeaways
Here are some important points to remember when filling out and using the DOH 4359 form:
- Complete All Sections: Ensure that every section of the form is filled out completely. Incomplete forms will be returned, which can delay necessary services.
- Patient Identifying Information: Accurately enter the patient's name, date of birth, address, and contact information. This information is essential for identification.
- Medical Findings: Provide detailed medical information. Include height, weight, primary and secondary diagnosis, and a description of the patient’s current condition.
- Stability of Condition: Clearly indicate if the patient’s condition is stable. This helps healthcare providers understand the level of care required.
- Medication Details: List all medications the patient is taking, including dosage and frequency. This should encompass both prescription and over-the-counter medications.
- Signature Required: A physician’s signature is mandatory. The physician certifies that the information provided is accurate by signing the form.
- Timely Submission: Return the completed form within 30 calendar days of the examination to avoid delays in care services.
Browse Other Templates
Sales Tax Certificate Virginia - Farmers should keep copies of the ST-18 for their records and potential future reference.
Department of Veterans Affairs Letterhead - Date of birth and Social Security number are requested for identification.
Mary K Cosmetics - Submitting your order is the first step to enjoying Mary Kay products.