Fill Out Your Em Audit Form
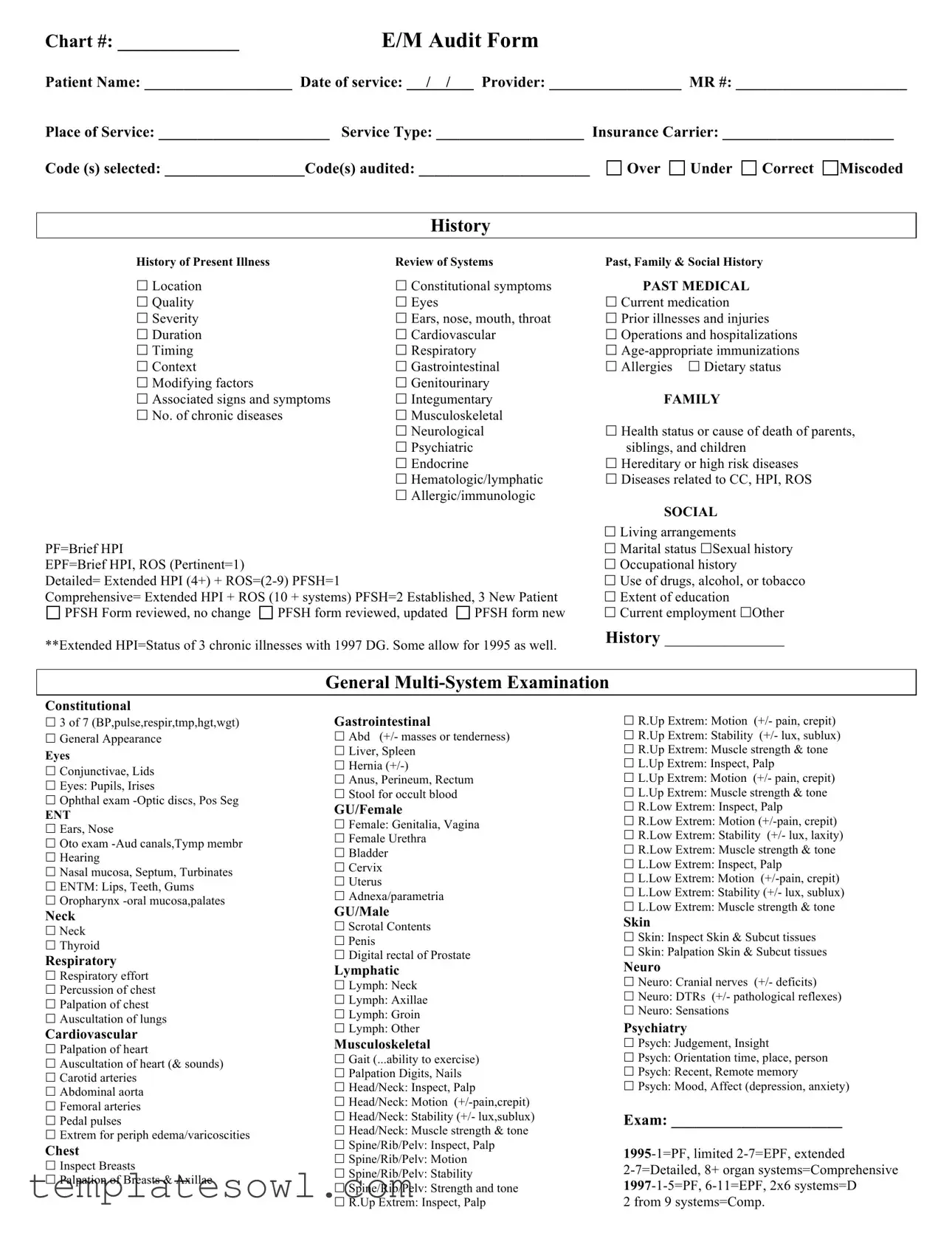
The E/M Audit Form plays a vital role in ensuring that healthcare providers receive appropriate compensation for their services while maintaining compliance with medical documentation standards. This form captures essential patient information, including chart number, patient name, date of service, and provider details. It outlines the components of a thorough evaluation, such as the patient's history, examination findings, and the complexities associated with their medical decision-making. Thorough history sections cover aspects like past medical, family, and social histories, along with the review of systems, which provide a well-rounded view of the patient's health status. The exam section articulates the comprehensive evaluation performed by the provider, detailing findings across various body systems. Moreover, the form highlights the necessity of analyzing diagnoses and management options while assessing the level of risk associated with the patient's condition. By organizing this information systematically, the E/M Audit Form not only streamlines the auditing process but also enhances the integrity of medical coding and billing practices.
Em Audit Example
Chart #: _____________E/M Audit Form
Patient Name: ___________________ Date of service: __ / /__ Provider: _________________ MR #: ______________________
Place of Service: ______________________ Service Type: ___________________ Insurance Carrier: ______________________ |
||||
Code (s) selected: __________________Code(s) audited: ______________________ |
Over |
Under |
Correct |
Miscoded |
History
History of Present Illness |
|
Review of Systems |
Past, Family & Social History |
|
Location |
|
Constitutional symptoms |
PAST MEDICAL |
|
Quality |
|
Eyes |
|
Current medication |
Severity |
|
Ears, nose, mouth, throat |
Prior illnesses and injuries |
|
Duration |
|
Cardiovascular |
Operations and hospitalizations |
|
Timing |
|
Respiratory |
|
|
Context |
|
Gastrointestinal |
Allergies Dietary status |
|
Modifying factors |
|
Genitourinary |
|
|
Associated signs and symptoms |
Integumentary |
FAMILY |
||
No. of chronic diseases |
Musculoskeletal |
|
||
|
|
Neurological |
Health status or cause of death of parents, |
|
|
|
Psychiatric |
|
siblings, and children |
|
|
Endocrine |
|
Hereditary or high risk diseases |
|
|
Hematologic/lymphatic |
Diseases related to CC, HPI, ROS |
|
|
|
Allergic/immunologic |
|
|
|
|
|
|
SOCIAL |
|
|
|
|
Living arrangements |
PF=Brief HPI |
|
|
|
Marital status Sexual history |
EPF=Brief HPI, ROS (Pertinent=1) |
|
|
|
Occupational history |
Detailed= Extended HPI (4+) + |
|
|
Use of drugs, alcohol, or tobacco |
|
Comprehensive= Extended HPI + ROS (10 + systems) PFSH=2 Established, 3 New Patient |
Extent of education |
|||
PFSH Form reviewed, no change |
PFSH form reviewed, updated |
PFSH form new |
Current employment Other |
|
**Extended HPI=Status of 3 chronic illnesses with 1997 DG. Some allow for 1995 as well. |
History ______________ |
|
|
|
|
General |
|
|
|
Constitutional
3 of 7 (BP,pulse,respir,tmp,hgt,wgt)
General Appearance
Eyes
Conjunctivae, Lids
Eyes: Pupils, Irises
Ophthal exam
ENT
Ears, Nose
Oto exam
Hearing
Nasal mucosa, Septum, Turbinates
ENTM: Lips, Teeth, Gums
Oropharynx
Neck
Neck
Thyroid
Respiratory
Respiratory effort
Percussion of chest
Palpation of chest
Auscultation of lungs
Cardiovascular
Palpation of heart
Auscultation of heart (& sounds)
Carotid arteries
Abdominal aorta
Femoral arteries
Pedal pulses
Extrem for periph edema/varicoscities
Chest
Inspect Breasts
Palpation of Breasts & Axillae
Gastrointestinal
Abd (+/- masses or tenderness)
Liver, Spleen
Hernia
Anus, Perineum, Rectum
Stool for occult blood
GU/Female
Female: Genitalia, Vagina
Female Urethra
Bladder
Cervix
Uterus
Adnexa/parametria
GU/Male
Scrotal Contents
Penis
Digital rectal of Prostate
Lymphatic
Lymph: Neck
Lymph: Axillae
Lymph: Groin
Lymph: Other
Musculoskeletal
Gait (...ability to exercise)
Palpation Digits, Nails
Head/Neck: Inspect, Palp
Head/Neck: Motion
Head/Neck: Stability (+/- lux,sublux)
Head/Neck: Muscle strength & tone
Spine/Rib/Pelv: Inspect, Palp
Spine/Rib/Pelv: Motion
Spine/Rib/Pelv: Stability
Spine/Rib/Pelv: Strength and tone
R.Up Extrem: Inspect, Palp
R.Up Extrem: Motion (+/- pain, crepit)
R.Up Extrem: Stability (+/- lux, sublux)
R.Up Extrem: Muscle strength & tone
L.Up Extrem: Inspect, Palp
L.Up Extrem: Motion (+/- pain, crepit)
L.Up Extrem: Muscle strength & tone
R.Low Extrem: Inspect, Palp
R.Low Extrem: Motion
R.Low Extrem: Stability (+/- lux, laxity)
R.Low Extrem: Muscle strength & tone
L.Low Extrem: Inspect, Palp
L.Low Extrem: Motion
L.Low Extrem: Stability (+/- lux, sublux)
L.Low Extrem: Muscle strength & tone
Skin
Skin: Inspect Skin & Subcut tissues
Skin: Palpation Skin & Subcut tissues
Neuro
Neuro: Cranial nerves (+/- deficits)
Neuro: DTRs (+/- pathological reflexes)
Neuro: Sensations
Psychiatry
Psych: Judgement, Insight
Psych: Orientation time, place, person
Psych: Recent, Remote memory
Psych: Mood, Affect (depression, anxiety)
Exam: ______________________
2 from 9 systems=Comp.
|
|
Number of |
Points |
|
|
|
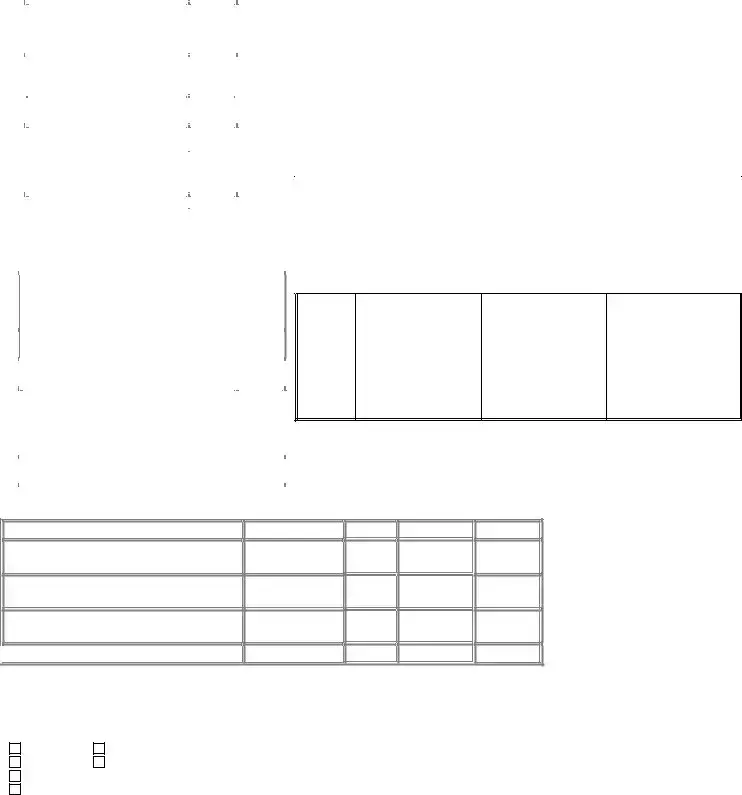
Diagnoses/Management Options |
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
improved or worsening) |
|
|
|
|
Maximum 2 points in this |
|
|
|
|
category. |
|
|
|
|
|
|
|
|
|
Established problem (to |
1 |
|
|
|
examining MD); stable or |
|
|
|
|
improved |
|
|
|
|
|
|
|
|
|
Established problem (to |
2 |
|
|
|
examining MD); worsening |
|
|
|
|
|
|
|
|
|
New problem (to examining MD); |
3 |
|
|
|
no additional |
|
|
|
|
|
|
|
|
|
New problem (to examining MD); |
4 |
|
|
|
additional |
|
|
|
|
admit/transfer) |
|
|
|
|
|
|
|
|
|
Total |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Amount and/or Complexity of Data |
|
Points |
|
|
Reviewed |
|
|
|
|
|
|
|
|
|
Lab ordered and/or reviewed (regardless of # |
1 |
|
|
|
ordered) |
|
|
TABLE OF RISK
Level of |
Presenting Problem(s) |
Diagnostic Procedure(s) |
Management Options |
Risk |
|
Ordered |
Selected |
|
|
|
|
|
•One |
• Laboratory tests requiring |
• Rest |
|
cold, insect bite, tinea corporis |
venipuncture |
• Gargles |
|
|
• Chest |
• Elastic bandages |
|
|
• EKG/EEG |
• Superficial dressings |
|
|
• Urinalysis |
|
|
|
• Ultrasound, eg, echocardiography |
|
Minimal |
|
• KOH prep |
|
|
|
|
|
|
• Two or more |
• Physiologic tests not under stress, eg, |
• |
|
problems |
pulmonary function tests |
• Minor surgery with no identified risk |
|
• One stable chronic illness, eg, well |
• |
factors |
|
controlled hypertension, |
with contrast, eg, barium enema |
• Physical therapy |
|
dependent diabetes, cataract, BPH |
• Superficial needle biopsies |
• Occupational therapy |
|
• Acute uncomplicated illness or injury, |
• Clinical laboratory tests requiring |
• IV fluids without additives |
|
eg, cystitis, allergic rhinitis, simple |
arterial puncture |
|
Low |
sprain |
• Skin biopsies |
|
|
|
|
|
|
• One or more chronic illnesses with |
• Physiologic tests under stress, eg, |
• Minor surgery with identified risk factors |
|
mild exacerbation, progression, or side |
cardiac stress test, fetal contraction |
• Elective major surgery (open, |
|
effects of treatment |
stress test |
percutaneous or endoscopic) with no |
|
• Two or more stable chronic illnesses |
• Diagnostic endoscopies with no |
identified risk factors |
|
• Undiagnosed new problem with |
identified risk factors |
• Prescription drug management |
|
uncertain prognosis, eg, lump in breast |
• Deep needle or incisional biopsy |
• Therapeutic nuclear medicine |
|
• Acute illness with systemic symptoms, |
• Cardiovascular imaging studies with |
• IV fluids with additives |
|
eg, pyelonephritis, pneumonitis, colitis |
contrast and no identified risk factors, |
• Closed treatment of fracture or dislocation |
|
• Acute complicated injury, eg, head |
eg, arteriogram, cardiac |
without manipulation |
|
injury with brief loss of consciousness |
catheterization |
|
|
|
• Obtain fluid from body cavity, eg |
|
|
|
lumbar puncture, thoracentesis, |
|
Moderate |
|
culdocentesis |
|
|
|
|
|
|
|
|
|
|
1 |
|
|
ordered) |
|
|
|
|
|
Medicine section |
1 |
|
and/or reviewed |
|
|
|
|
|
Discussion of test results with performing |
1 |
|
physician |
|
|
|
|
|
Decision to obtain old record and/or obtain hx |
1 |
|
from someone other than patient |
|
|
|
|
|
Review and summary of old records and/or |
|
|
obtaining hx from someone other than patient |
2 |
|
and/or discussion with other health provider |
|
|
|
|
|
Independent visualization of image, tracing, or |
2 |
|
specimen (not simply review of report) |
|
|
|
|
|
Total |
|
|
|
|
High
•One or more chronic illnesses with severe exacerbation, progression, or side effects of treatment
•Acute or chronic illnesses or injuries that pose a threat to life or bodily function, eg, multiple trauma, acute MI, pulmonary embolus, severe respiratory distress, progressive severe rheumatoid arthritis, psychiatric illness with potential threat to self or others, peritonitis, acute renal failure
•An abrupt change in neurologic status, eg, seizure, TIA, weakness, sensory loss
•Cardiovascular imaging studies with contrast with identified risk factors
•Cardiac electrophysiological tests
•Diagnostic Endoscopies with identified risk factors
•Discography
•Elective major surgery (open, percutaneous or endoscopic) with identified risk factors
•Emergency major surgery (open, percutaneous or endoscopic)
•Parenteral controlled substances
•Drug therapy requiring intensive monitoring for toxicity
•Decision not to resuscitate or to de- escalate care because of poor prognosis
Medical Decision Making
Number of Diagnoses or Treatment Options
Amount and/or Complexity of Data to be Reviewed
Risk of Complications, Morbidity, Mortality

 MDM Level=2 out of 3
MDM Level=2 out of 3
SF
1
1
Minimal
LOW
2
2
Low
MOD
3
3
Moderate
HIGH
4
4
High
MDM ______________
Chart Note |
Comments |
Dictated |
Handwritten |
Form |
Illegible |
Note signed
Signature missing
Other Services or Modalities:
Auditor’s Signature
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The E/M Audit form evaluates the medical decision-making process and documentation accuracy for patient visits. |
| Components | It includes sections for history, examination, medical decision-making, and risk assessment. |
| Use Cases | Providers use it during audits to ensure compliance with coding standards and to enhance billing accuracy. |
| State-Specific Requirements | This form complies with federal regulations and state-specific laws as applicable, like the Medicare guidelines. |
| Importance of Accuracy | Accurate completion of the form is crucial to prevent billing errors and potential audits from insurance carriers. |
Guidelines on Utilizing Em Audit
Completing the E/M Audit form requires careful attention to details about the patient encounter. Steps outlined below will guide you through the process of filling out the form to ensure accurate and comprehensive documentation.
- Start by entering the Chart # in the designated space.
- Fill in the patient's Name and the Date of Service using the format __/__/__.
- Write the Provider's Name and the Medical Record #.
- Indicate the Place of Service.
- Select the Service Type from the provided options.
- Identify the Insurance Carrier associated with the patient.
- Enter the Code(s) selected and the Code(s) audited.
- Identify whether there are any discrepancies in coding by checking the relevant boxes under Over, Under, Correct, or Miscoded.
- Provide details about the patient’s History by completing sections like History of Present Illness and Review of Systems.
- Document the Past, Family & Social History as outlined in the checklist.
- Complete the Physical Examination section by marking the appropriate findings.
- Assess Number of Points for diagnoses and management options based on the patient’s level of complexity.
- Document the Total Amount and/or Complexity of Data Points Reviewed.
- Review the Table of Risk to determine the risk level associated with the presenting problem(s) and document accordingly.
- Calculate the Medical Decision Making (MDM) level based on the defined criteria.
- Take note of any Chart Note Comments and complete all necessary information about dictated or handwritten notes.
- Finally, secure the Auditor’s Signature in the designated area.
What You Should Know About This Form
What is the purpose of the E/M Audit Form?
The E/M Audit Form is designed to evaluate the documentation of Evaluation and Management (E/M) services provided during a patient visit. It helps ensure compliance with coding standards and guidelines, ultimately promoting accurate billing and reimbursement. By auditing the level of service documented, healthcare providers can identify areas of improvement in their documentation practices.
How do I fill in the patient information on the E/M Audit Form?
Begin by entering the patient's chart number, name, and medical record number (MR#) at the top of the form. Next, include the date of service and the name of the provider. Specify the place of service, type of service, and the insurance carrier. Ensuring this information is accurate is essential, as it helps track patient visits and supports billing purposes.
What does the "History" section entail?
The "History" section captures various aspects of the patient's medical history. This includes details on the history of present illness, review of systems, and past, family, and social history. Each bullet point highlights specific elements that should be documented, such as location, severity, and duration of symptoms. Thorough documentation helps in understanding the patient’s condition better and facilitates better treatment.
What counts as "Medical Decision Making" on the form?
Medical Decision Making (MDM) includes assessing the number of diagnoses and treatment options for the patient, the complexity of data to be reviewed, and the associated risks. Each of these components contributes to determining the level of service provided. Detailed information on the patient’s status aids in evaluating the overall situation and guides the next steps in care.
How do I determine the level of risk associated with a patient’s condition?
The form categorizes risk levels into four groups: minimal, low, moderate, and high. Each level corresponds to the severity and complexity of the patient's presenting problems. For example, a self-limited issue would be minimal risk, while an acute illness that poses a threat to life falls under high risk. Assessing risk properly is crucial for determining the appropriate level of care and coding.
What should I do if I find discrepancies in the coding during an audit?
If discrepancies are found during the audit, document your findings clearly. It’s important to communicate these issues to the provider involved for clarification. Correcting any coding errors is necessary to ensure compliance with regulations and to facilitate accurate reimbursement. Keeping open communication improves future documentation practices.
Who is responsible for signing the E/M Audit Form?
The E/M Audit Form should be signed by the auditor who conducted the review. If any additional documentation is needed or if there are comments on the audit, they should be noted on the form as well. This signature signifies that the audit is complete and that the information has been thoroughly evaluated for accuracy.
Common mistakes
Completing the E/M Audit form can be a detailed task, and it's easy to overlook certain aspects. One common mistake is leaving out the chart number or patient name. This information is crucial for identifying the patient's record and linking it to the appropriate medical services rendered. Omitting such details can cause significant delays and lead to confusion during audits. Always ensure that every section requiring basic patient identifiers is filled out accurately.
Another mistake involves the date of service. Failing to write the correct date can result in complications, especially if the visit needs to be correlated with other medical records. It is essential to double-check the date against the patient's visit notes to avoid discrepancies that could complicate billing and reporting.
People often misinterpret the sections dealing with history taking. A common error is not clearly documenting the History of Present Illness (HPI) or associated past medical history. Details should be explained thoroughly, including attributes of the symptoms, context, and modifying factors. Incomplete HPI can lead to undercoding or misclassification of the severity of the visit.
Additionally, coding mistakes can be frequent. Individuals sometimes select codes without adequately reviewing the specific requirements for each coding level. It is vital to understand the differences between categories like established and new patient visits, as well as the conditions that affect coding criteria, such as the complexity of medical decision making.
Neglecting the review of systems can also hinder proper documentation. This section should include pertinent symptoms reviewed to avoid missing out on critical patient information that could affect both diagnosis and treatment decisions. Documenting only superficial details, while ignoring significant related systems, can misrepresent the patient's medical condition.
Another area where mistakes occur is in the documentation of medical decision-making levels. Individuals may not fully understand how to categorize diagnoses or the complexity of data reviewed. Consequently, it’s essential to clarify how many diagnoses are considered and which procedures were utilized to accurately reflect the service provided.
Moreover, signing the form is often overlooked. Individuals might complete all sections but forget to provide a signature. This oversight can invalidate the form and cause significant delays in processing, making it necessary to follow up again to remedy the situation.
Lastly, individuals sometimes fail to provide sufficient detail in the comments section. The comments should provide context or highlight unusual aspects of the visit. This section is essential to convey important nuances that a simple checkmark cannot capture. Clear and detailed notes can improve the understanding of the service provided during audits.
Documents used along the form
The E/M Audit Form is a crucial document used by healthcare providers to assess the appropriateness of the billing codes associated with patient encounters. Alongside this form, there are several additional documents and forms that help support, clarify, or complement the auditing process. Each of these documents plays a specific role in ensuring accurate coding, billing, and patient care documentation.
- Patient Encounter Notes: These are detailed records of a patient's visit, typically including the patient's history, examination findings, and the provider's clinical decision-making. They are essential for justifying the use of specific billing codes.
- History and Physical (H&P) Examination: This document captures both the medical history of the patient and the findings from the physical examination. It provides context for the care provided and informs the coding decision.
- Progress Notes: Progress notes are used to document the patient's ongoing care. These notes outline any changes in the patient's condition, responses to treatment, and any additional evaluations or treatments performed during their care.
- Referral Forms: Referral forms are essential when a patient is referred to another provider for specialized care. These forms generally include important clinical information that both the referring and receiving providers need.
- Consent Forms: Obtaining informed consent from patients before procedures or treatments is crucial. These forms ensure that patients understand and accept the risks associated with their care.
- Insurance Verification Documents: These documents are used to confirm a patient's insurance coverage and benefits before services are rendered. They ensure that the services provided will be covered by the patient's insurance plan.
- Diagnostic Test Results: Reports from tests such as lab results, imaging studies, or other diagnostics provide critical information that guides treatment and supports coding decisions.
- Billing Statements: Billing statements summarize the services provided, the associated costs, and the patient’s financial responsibility. They provide transparency and clarity regarding charges related to patient care.
- Audit Reports: Following the E/M audit, reports detailing findings and recommendations are generated. These reports are essential in identifying coding discrepancies and ensuring compliance with regulations.
By utilizing these documents alongside the E/M Audit Form, healthcare providers can foster a thorough review process that aids in maintaining compliance and ensuring that patient care is documented accurately. This comprehensive approach contributes to better patient outcomes and boosts the integrity of the billing process.
Similar forms
- SOAP Notes: Both the Em Audit form and SOAP notes require structured documentation of patient encounters. SOAP stands for Subjective, Objective, Assessment, and Plan, focusing on summarizing patient information and care processes.
- Clinical Evaluation Templates: These documents share the goal of standardizing the assessment of patient conditions. They guide healthcare providers through specific criteria for evaluations.
- Billing and Coding Forms: The Em Audit form aligns closely with billing and coding forms as both address the classification of services provided, ensuring accurate reimbursement and compliance.
- Progress Notes: While both document patient interactions over time, the Em Audit focuses more on compliance and coding accuracy, whereas progress notes detail ongoing care and changes in patient condition.
- History and Physical (H&P) Reports: Both documents collect comprehensive patient data. H&P reports capture a patient's medical history and findings from physical exams, which are also crucial for audits.
- Quality Assurance Checklists: Similar to the Em Audit form, quality assurance checklists are used to evaluate the completeness and accuracy of patient care standards, ensuring protocols are followed consistently.
- Referral and Consultation Documentation: Both types of documents address patient assessments and management plans. However, referral documentation often requires detailing why a patient needs specialist care, while the Em Audit form focuses on auditing service types and coding.
Dos and Don'ts
When filling out the E/M Audit form, there are important guidelines to keep in mind. Here are nine essential do's and don'ts to help you navigate this process effectively.
- Do: Ensure all fields are filled out completely.
- Do: Double-check patient information for accuracy.
- Do: Use clear and concise descriptions in the history sections.
- Do: Verify that selected codes match the documented services.
- Do: Review prior notes or forms to track changes in the patient's status.
- Don't: Forget to sign and date the form.
- Don't: Leave any sections blank unless not applicable.
- Don't: Use medical jargon that could confuse other reviewers.
- Don't: Underestimate the importance of thorough documentation.
- Don't: Rush through the audit process; take the time necessary to ensure accuracy.
Misconceptions
Understanding the E/M Audit Form is crucial for effective medical billing and coding. However, several misconceptions about this form can lead to confusion. Here are six common misconceptions, along with clarifications for each.
- Misconception 1: The E/M Audit Form is only for new patients.
- Misconception 2: All sections need to be completed for every visit.
- Misconception 3: The E/M Audit Form replaces the need for other documentation.
- Misconception 4: Using the highest level code automatically guarantees reimbursement.
- Misconception 5: E/M coding is straightforward and does not require ongoing education.
- Misconception 6: The E/M Audit Form is designed only for auditors.
This is incorrect. The form applies to both new and established patients. The code selection process and documentation requirements differ based on patient status, but both types can be evaluated using the form.
Not necessarily. While comprehensive documentation is often beneficial, the level of detail required can depend on the complexity of the visit. A brief visit may only need key sections filled out to appropriately reflect the service provided.
This is misleading. The E/M Audit Form serves as a tool to assist in coding and billing but does not replace clinical notes or other medical documentation. Providers must maintain comprehensive records to substantiate care decisions.
This is a misunderstanding of the process. Reimbursement is based not just on the code level but also on the clinical documentation that supports it. Appropriate justification for the chosen code is paramount for successful reimbursement.
This misconception undermines the complex and evolving nature of medical coding. Coding guidelines frequently change, and staying informed is essential. Regular training and updates are necessary to ensure compliance and accuracy.
This is incorrect as well. While auditors utilize this form for evaluation, healthcare providers should also be familiar with its structure and requirements. Understanding the form enhances the accuracy of documentation and coding from the outset.
Key takeaways
Here are some key takeaways for effectively filling out and using the E/M Audit form:
- Accurate Patient Information: Always ensure that patient details, such as name, chart number, and date of service, are accurately recorded to avoid processing errors.
- Comprehensive Documentation: Record all aspects of the patient’s history, examination, and medical decision-making to provide clear evidence of the services rendered.
- Understanding Code Selection: Familiarize yourself with the various E/M codes available. Selecting the correct code is crucial for appropriate billing and compliance.
- Review of Systems: Conduct a thorough review of systems. This helps in documenting relevant information that supports the medical necessity of the services provided.
- Audit Completion: Ensure that the form is fully completed before submission. Missing information can lead to delays or denials in reimbursement.
Following these takeaways will enhance the accuracy and efficiency of the E/M audit process, ensuring better compliance and optimized reimbursement.
Browse Other Templates
Private Investigator Agency Application,P.I. Principal Endorsement Addendum,Business License Addendum for Investigative Agencies,BLS Private Investigative Agency Supplemental Form,Principal Investigator Licensing Form,Agency and Principal Endorsement - The detailed nature of the form reflects the serious nature of private investigative work and public safety.
Gcaar Residential Lease Washington Dc - Pet ownership is addressed, with sections dedicated to the type and number of pets being moved into the property.
If You Win the Lottery Can You Remain Anonymous in California - Submit your claim promptly to ensure timely processing of the prize.