Fill Out Your Empire Referral Form
The Empire Referral form plays a crucial role in accessing specialized healthcare services for patients covered by certain Empire health plans, including HMO, Child Health Plus, Healthy NY, and Direct Pay HMO plans. This form is essential for initiating a referral from a primary care physician to a specialist, ensuring that the patient's journey through the healthcare system is streamlined and compliant with the insurance requirements. The referral remains valid for a period of 90 days from the service start date, allowing patients a reasonable timeframe to schedule necessary appointments. Notably, there are mandatory fields within the form, and missing any of these required elements may result in denial or rejection of the referral. Certain services, such as inpatient admissions, surgery performed outside of the physician's office, and emergency admissions, require separate approval from Empire Medical Management, underlining the importance of understanding what is and isn't covered. Additionally, the form captures detailed patient and physician information, which is crucial for maintaining accurate medical records and ensuring continuity of care. Overall, completing the Empire Referral form is a key step for patients seeking specialized treatment and navigating their health insurance requirements effectively.
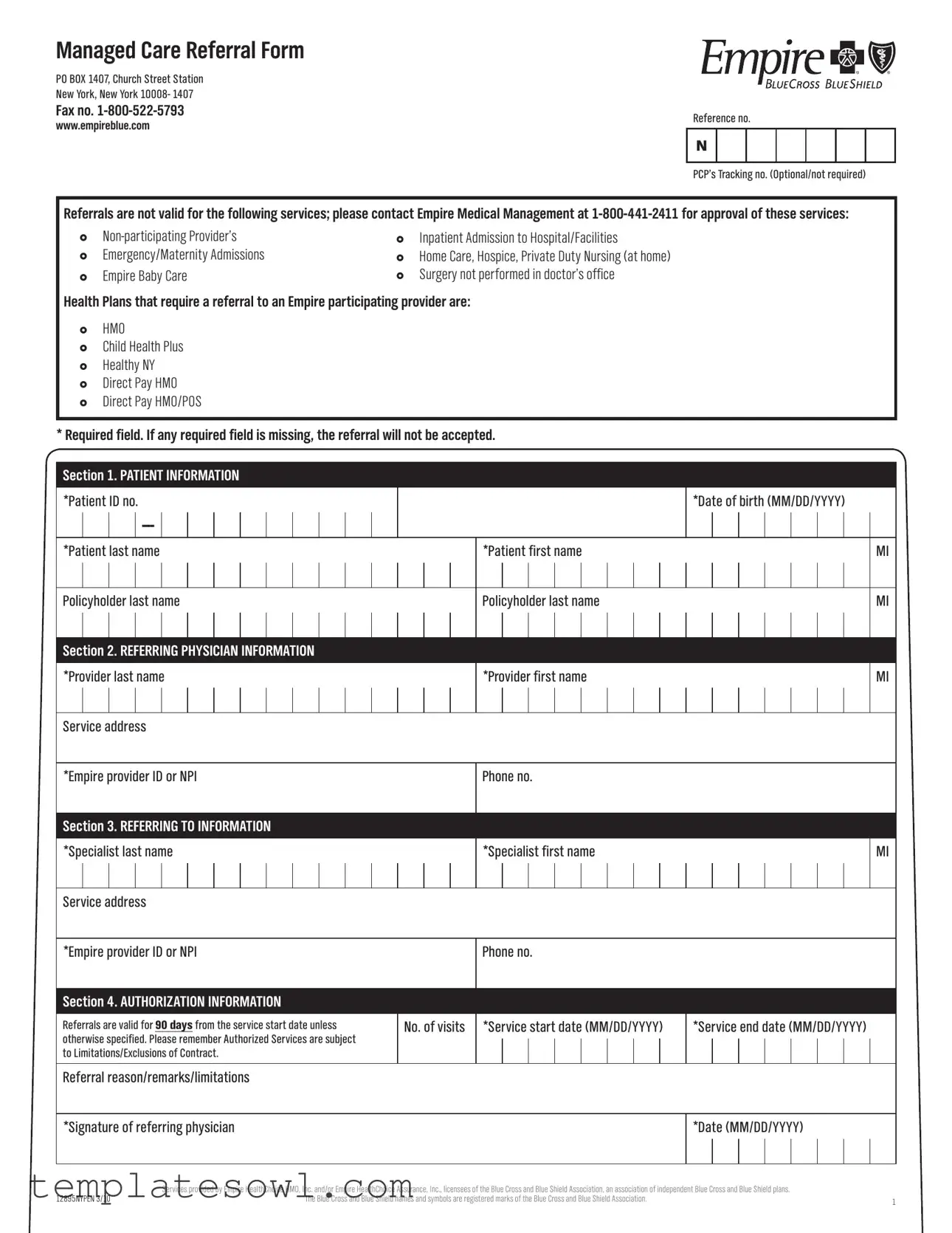
Empire Referral Example
Managed Care Referral Form
PO BOX 1407, Church Street Station
New York, New York 10008- 1407
Fax no.
www.empireblue.com
Reference no.
N
PCP’s Tracking no. (Optional/not required)
Referrals are not valid for the following services; please contact Empire Medical Management at
} |
} Inpatient Admission to Hospital/Facilities |
||
} |
Emergency/Maternity Admissions |
} |
Home Care, Hospice, Private Duty Nursing (at home) |
} |
Empire Baby Care |
} |
Surgery not performed in doctor’s office |
Health Plans that require a referral to an Empire participating provider are:
}HMO
}Child Health Plus
}Healthy NY
}Direct Pay HMO
}Direct Pay HMO/POS
* Required field. If any required field is missing, the referral will not be accepted.
Section 1. PATIENT INFORMATION
*Patient ID no.
*Patient last name
Policyholder last name
|
|
|
|
|
|
|
|
*Date of birth (MM/DD/YYYY) |
|||||||
*Patient first name |
|
|
|
|
|
|
|
MI |
|||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Policyholder last name |
|
|
|
|
|
|
|
MI |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Section 2. REFERRING PHYSICIAN INFORMATION
*Provider last name
*Provider first name
MI
Service address
*Empire provider ID or NPI |
|
Phone no. |
Section 3. REFERRING TO INFORMATION |
|
|
|
|
|
*Specialist last name |
|
*Specialist first name |
|
||
|
|
|
MI
Service address
*Empire provider ID or NPI
Phone no.
Section 4. AUTHORIZATION INFORMATION
Referrals are valid for 90 daysfrom the service start date unless otherwise specified. Please remember Authorized Services are subject to Limitations/Exclusions of Contract.
No. of visits
*Service start date (MM/DD/YYYY)
*Service end date (MM/DD/YYYY)
Referral reason/remarks/limitations
*Signature of referring physician
*Date (MM/DD/YYYY)
|
Services provided by Empire HealthChoice HMO, Inc. and/or Empire HealthChoice Assurance, Inc., licensees of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield plans. |
|
12895NYPEN 3/10 |
The Blue Cross and Blue Shield names and symbols are registered marks of the Blue Cross and Blue Shield Association. |
1 |
|
|
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Purpose | This form facilitates referrals to Empire participating providers for specific health plans. |
| Validity Period | Referrals are valid for 90 days from the service start date unless indicated otherwise. |
| Required Fields | Missing any required field will result in the referral being rejected. |
| Services Requiring Approval | Services like inpatient admissions and non-participating providers need prior approval from Empire Medical Management. |
| Applicable Health Plans | Plans such as HMO, Child Health Plus, and Healthy NY require referrals to Empire participating providers. |
| Governing Laws | This form is governed by relevant New York State insurance laws. |
Guidelines on Utilizing Empire Referral
Completing the Empire Referral Form is essential for ensuring that your medical referrals are processed efficiently. Follow these steps carefully to fill out the form, ensuring all required fields are accurately completed. Missing information can delay your referral, so double-check each section before submitting.
- Start with Section 1: Patient Information. Fill in the patient's ID number, last name, first name, middle initial, date of birth, and policyholder's last name and middle initial, where applicable. Remember, these fields marked with an asterisk (*) are required.
- Proceed to Section 2: Referring Physician Information. Here, fill in the provider's last name, first name, middle initial, service address, Empire provider ID (or NPI), and phone number. Again, required fields are marked with an asterisk (*).
- Next, move to Section 3: Referring To Information. Enter the specialist's last name, first name, middle initial, service address, Empire provider ID (or NPI), and phone number. Ensure all necessary fields are completed.
- Now, fill out Section 4: Authorization Information. Specify the number of visits, service start date, and service end date. Note that the service start and end dates should be in the format MM/DD/YYYY. Provide a referral reason and any remarks or limitations as necessary.
- Finally, have the referring physician sign the form and provide the date. These steps confirm authorization for the referral.
Once you have completed the form, send it to the appropriate address or fax number provided at the top of the document. It's also a good idea to keep a copy for your records. By following these steps, you help facilitate timely medical care and ensure that any required approvals are obtained efficiently.
What You Should Know About This Form
What is the purpose of the Empire Referral form?
The Empire Referral form serves as a necessary document for patients seeking specialist services within the Empire network. It is particularly essential for those enrolled in specific health plans that require referrals, including HMO, Child Health Plus, and Healthy NY. By completing this form, patients ensure that their referrals are tracked and approved, facilitating timely access to care. It also outlines the parameters for authorized services, which are crucial for both healthcare providers and patients.
How long is a referral valid once submitted?
Once the Empire Referral form is submitted and approved, the referral is valid for a period of 90 days from the service start date. This time frame allows patients to schedule necessary appointments within a reasonable period. If additional time is required, it is advisable to communicate with the referring physician or the Empire Medical Management team to discuss further options or extensions.
What happens if a required field on the referral form is incomplete?
If any required field is missing from the referral form, the submission will not be accepted. This means that all essential information, such as patient ID numbers, dates of birth, and signature of the referring physician, must be accurately filled in. It is crucial for patients and providers to double-check the form before submission to prevent delays in processing referrals. Missing information can disrupt access to much-needed specialty care.
Which services require prior approval from Empire Medical Management?
Several services are not valid under the referral process and require prior approval from Empire Medical Management. This includes visits to non-participating providers, inpatient admissions to hospitals or facilities, emergency and maternity admissions, home care, hospice, and private duty nursing at home. Surgery that is not performed in a doctor’s office additionally falls under this category. Patients should contact Empire Medical Management directly at 1-800-441-2411 to obtain approval for these services before proceeding.
Common mistakes
Filling out the Empire Referral form may seem straightforward, but many individuals encounter common pitfalls that can lead to delays or outright rejection of their referrals. Understanding these mistakes can enhance compliance and ensure smoother processing.
One frequent error occurs with the completion of required fields, such as patient information. Essential details like the *Patient ID no.*, *Date of birth*, and names must be accurately filled. Omitting any of these fields often results in the referral not being accepted. Attention to comprehensive detail is crucial.
Additionally, people often overlook the importance of providing an accurate service start date and service end date. Referrals are only valid for 90 days from the service start date unless specified otherwise. Without valid dates, processing may stall, and the referral may no longer be applicable by the time it is reviewed.
Inaccuracies in the referring physician’s information can also create significant challenges. Provider details, including the *Provider last name*, *first name*, and *Empire provider ID or NPI*, must match their official records. Mismatches or typos here can result in unnecessary back-and-forth communication with the insurance carrier.
Moreover, failing to include the reason for referral or other remarks poses another common issue. The form specifically requests a section for referral reason, but incomplete explanations can lead to confusion. A well-articulated reason can clarify the necessity of the referral and expedite approval.
Many individuals neglect to double-check the signature of the referring physician. Without a valid signature and date, the form is incomplete. This simple yet vital detail should not be overlooked, as it is a formal requirement for the referral to be deemed legitimate.
Another mistake occurs when people fail to contact Empire Medical Management regarding services not covered by standard referrals. Services such as inpatient admissions, emergency care, or non-participating providers require separate approval. Not seeking this prior authorization can result in unexpected costs and treatment delays.
Furthermore, there's often confusion surrounding the different health plans that require a referral. If individuals applying for a referral are uncertain whether their plan falls under HMO, Child Health Plus, or another category, it can lead to mistakes. Understanding one's coverage helps navigate this process effectively.
Lastly, many forms do not clearly state or remember the limitations and exclusions stipulated in their insurance contracts. Familiarity with these aspects can help set realistic expectations regarding what treatments or services are approved. Not taking time to review these limitations may result in unexpected denials.
In essence, careful attention to detail while filling out the Empire Referral form is essential. Avoiding these common mistakes can facilitate a more efficient referral process, allowing patients to receive the care they need in a timely manner.
Documents used along the form
When dealing with healthcare referrals, several important documents are often used in conjunction with the Empire Referral form. These forms help ensure that all necessary information is correctly submitted, facilitating smoother processing for patient care. Here’s a brief overview of some of the most commonly used documents:
- Patient Information Form: This document collects essential details about the patient, including contact information, medical history, and insurance details. It is crucial for verifying eligibility and streamlining the referral process.
- Authorization for Release of Information: This form allows healthcare providers to share patient information with other providers or specialists. It ensures compliance with privacy laws while enabling better coordination of care.
- Prior Authorization Request: Certain healthcare services may require prior approval from the insurance provider. This form outlines the medical necessity for services and must be submitted before treatment begins to avoid any delays.
- Specialist Appointment Scheduling Form: Once a referral is made, this form helps coordinate the patient's appointment with the specialist. It usually includes preferences for times and dates to ensure the best fit for the patient.
- Referral Feedback Form: After the patient visits the specialist, this form gathers feedback on the visit and outcomes. It helps referring physicians stay informed and ensures continuity of care.
- Health Plan Benefits Summary: This document outlines what is covered under the patient's health plan, including co-pays, deductibles, and services that may require referrals. Understanding this helps patients navigate their benefits effectively.
Using these forms together with the Empire Referral form can lead to a more efficient and thorough referral process. Proper documentation supports better communication among providers, which ultimately enhances patient care.
Similar forms
- Insurance Authorization Form: Like the Empire Referral form, the Insurance Authorization form requests permission for specific services or procedures. Both require detailed patient information and physician signatures, ensuring that necessary approvals are obtained before treatment.
- Pre-Authorization Request: Similar to the Empire Referral, this document is used to obtain pre-approval from an insurer before a service is rendered. It asks for similar details regarding the patient and refers to any limitations or exclusions that may apply.
- Referral Letter: A Referral Letter serves to direct patients from one healthcare provider to another. It includes patient and provider details, much like the Empire Referral form, and explains the reason for the referral to ensure continuity of care.
- Service Agreement: This document outlines the terms and conditions under which a service will be provided. While it does not focus on referrals, it shares the requirement for clear communication between providers and detailed patient information, akin to what is found on the Empire Referral form.
- Patient Information Form: This document collects a wide range of personal and medical history information from patients. It is similar to the Empire Referral form in its emphasis on gathering necessary details to facilitate communication and care between providers.
Dos and Don'ts
When filling out the Empire Referral form, it's important to be mindful of several key points. Here’s a list of things you should and shouldn’t do:
- Do: Ensure all required fields are filled out completely.
- Do: Use the correct format for the date (MM/DD/YYYY).
- Do: Verify that the patient ID number is accurate and included.
- Do: Provide the complete name of both the referring physician and the specialist.
- Do: Keep a copy of the filled form for your records.
- Don't: Forget to include the referral reason or any remarks.
- Don't: Leave out the signature of the referring physician.
- Don't: Submit the form without checking for any missing information.
- Don't: Use an outdated referral form; ensure you have the latest version.
- Don't: Assume that the referral is valid beyond the specified 90 days unless confirmed.
By following these guidelines, you can help ensure that the referral process goes smoothly and efficiently.
Misconceptions
Here are six common misconceptions about the Empire Referral form:
- Referrals are not mandatory for all services. Many people believe that all healthcare services require a referral. However, only specific plans, like HMO, require referrals. Always confirm your plan's requirements.
- The referral is valid indefinitely. Some assume once a referral is given, it lasts forever. In reality, referrals are valid for 90 days from the service start date unless specified otherwise.
- Contacting the referring physician is optional. Individuals might think they don't need to reach out to their physician for the referral. In truth, incomplete forms or missing required fields will lead to rejection, so it’s essential to follow up.
- Any physician can provide a referral. People often think any healthcare provider can refer patients. Only Empire participating providers can issue valid referrals under the plans that require them.
- It's fine to use a non-participating provider. Some may believe they can see any specialist regardless of their status. Referrals for non-participating providers will not be accepted, so prior approval is crucial.
- You can fill out the form at any time. Many assume that there's flexibility in when to submit the referral. However, it's essential to complete and submit the form before any scheduled services to ensure coverage.
Understanding these points will help streamline the referral process and avoid potential issues. Take action promptly to ensure you receive the necessary care without delays.
Key takeaways
When filling out and using the Empire Referral form, there are several important considerations to keep in mind to ensure a smooth process. Below are key takeaways that can guide you through this task.
- Validity Period: Referrals are valid for 90 days from the service start date unless noted otherwise.
- Required Information: Complete all required fields. Missing information will result in the referral being rejected.
- Contact Numbers: For services not covered under the referral, contact Empire Medical Management at 1-800-441-2411.
- Service Limitations: Remember that authorized services may have limitations and exclusions as outlined in the contract.
- Provider Information: Ensure correct details for both the referring physician and the specialist are filled out accurately.
- Tracking Number: While optional, including the PCP’s tracking number can help in monitoring the referral process.
- Submission Methods: The form can be submitted via mail or fax. The fax number is 1-800-522-5793.
- Emergency Services: Specific services such as inpatient admissions and emergency care require separate approval.
- Health Plans: Ensure awareness of the health plans requiring a referral to an Empire participating provider, including HMO and Child Health Plus.
Being vigilant about these details will facilitate obtaining the necessary authorizations for medical services, helping to provide patients with the care they need.
Browse Other Templates
Roundtable Pizza - If you cannot perform specific duties, detail those limitations.
Cash Vault Services - Changes can reflect in your account shortly after the request is verified.
Assistance Disclosure Form,Recipient Update Report,HUD Assistance Summary,Project Funding Disclosure,Government Assistance Application,Recipient Information Report,Financial Interest Disclosure,Assistance Request Form,Application Assistance Disclosur - Ultimately, the HUD 2880 strives to create a transparent environment for both applicants and the funding agency.