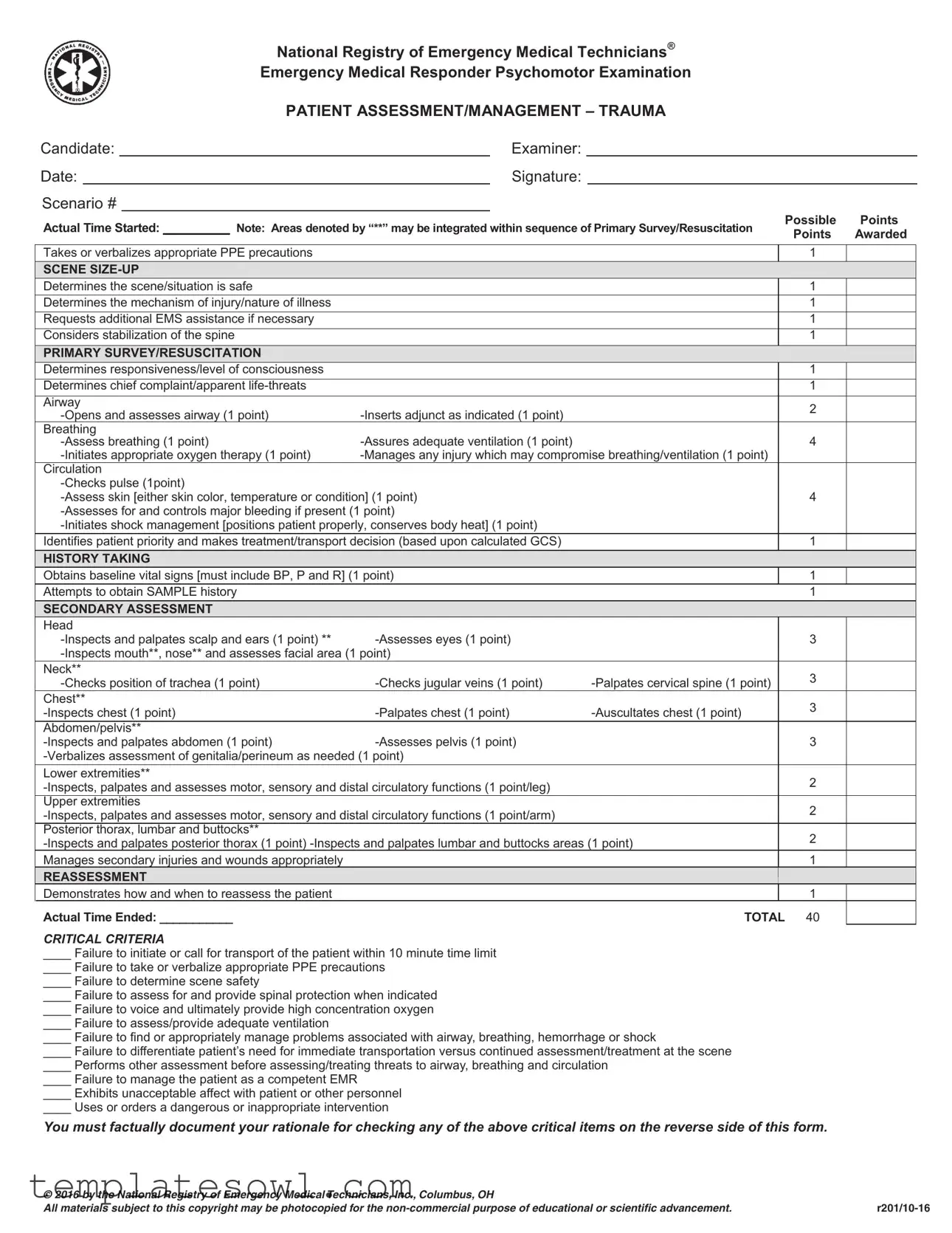
Fill Out Your Emt Trauma Assessment Form
The EMT Trauma Assessment Form is an essential tool used by emergency medical responders to evaluate and manage trauma patients effectively. This comprehensive document guides responders through a series of critical assessments, starting from the scene size-up, where safety and mechanism of injury are assessed, to the primary survey that focuses on the patient's immediate life threats. It provides a structured approach to gather vital information, ensuring that the responder can act quickly and efficiently. The form covers various aspects of patient assessment, including the evaluation of airway, breathing, and circulation, as well as obtaining a thorough history through the SAMPLE method. Additionally, it emphasizes the importance of reassessing the patient to monitor any changes in condition. Each section has clearly defined points that can be awarded based on the responder's performance, fostering a systematic and organized method of trauma care. By adhering to the form's guidelines, EMTs can prioritize interventions and transportation decisions, ultimately improving patient outcomes in critical situations.
Emt Trauma Assessment Example
National Registry of Emergency Medical Technicians®
Emergency Medical Responder Psychomotor Examination
|
|
|
PATIENT ASSESSMENT/MANAGEMENT – TRAUMA |
|
|
||||
Candidate: |
|
|
Examiner: |
|
|
|
|||
Date: |
|
|
Signature: |
|
|
|
|||
Scenario # |
|
|
|
|
Possible |
Points |
|||
Actual Time Started: __________ Note: Areas denoted by “**” may be integrated within sequence of Primary Survey/Resuscitation |
|||||||||
Points |
Awarded |
||||||||
|
|
|
|
|
|
|
|||
Takes or verbalizes appropriate PPE precautions |
|
|
|
1 |
|
||||
SCENE |
|
|
|
|
|
||||
Determines the scene/situation is safe |
|
|
|
1 |
|
||||
Determines the mechanism of injury/nature of illness |
|
|
|
1 |
|
||||
Requests additional EMS assistance if necessary |
|
|
|
1 |
|
||||
Considers stabilization of the spine |
|
|
|
1 |
|
||||
PRIMARY SURVEY/RESUSCITATION |
|
|
|
|
|
||||
Determines responsiveness/level of consciousness |
|
|
|
1 |
|
||||
Determines chief complaint/apparent |
|
|
|
1 |
|
||||
Airway |
|
|
|
2 |
|
||||
|
|
||||||||
|
|
|
|||||||
Breathing |
|
4 |
|
||||||
|
|
||||||||
|
|
||||||||
Circulation |
|
|
|
|
|
||||
|
|
|
|
|
|||||
|
4 |
|
|||||||
|
|
|
|||||||
|
|
|
|||||||
Identifies patient priority and makes treatment/transport decision (based upon calculated GCS) |
|
1 |
|
||||||
HISTORY TAKING |
|
|
|
|
|
||||
Obtains baseline vital signs [must include BP, P and R] (1 point) |
|
1 |
|
||||||
Attempts to obtain SAMPLE history |
|
|
|
1 |
|
||||
SECONDARY ASSESSMENT |
|
|
|
|
|
||||
Head |
|
|
|
|
|
||||
|
3 |
|
|||||||
|
|
|
|||||||
Neck** |
|
|
|
3 |
|
||||
|
|||||||||
|
|
||||||||
Chest** |
|
|
|
3 |
|
||||
|
|||||||||
|
|
||||||||
Abdomen/pelvis** |
|
|
|
|
|
||||
|
3 |
|
|||||||
|
|
|
|||||||
Lower extremities** |
|
|
|
2 |
|
||||
|
|
||||||||
Upper extremities |
|
|
|
2 |
|
||||
|
|
||||||||
Posterior thorax, lumbar and buttocks** |
|
|
|
2 |
|
||||
|
|||||||||
|
|
||||||||
Manages secondary injuries and wounds appropriately |
|
|
|
1 |
|
||||
REASSESSMENT |
|
|
|
|
|
||||
Demonstrates how and when to reassess the patient |
|
|
|
1 |
|
||||
Actual Time Ended: ___________ |
|
|
TOTAL 40 |
|
|||||
CRITICAL CRITERIA |
|
|
|
|
|
||||
____ Failure to initiate or call for transport of the patient within 10 minute time limit |
|
|
|
||||||
____ Failure to take or verbalize appropriate PPE precautions |
|
|
|
||||||
____ Failure to determine scene safety |
|
|
|
|
|
||||
____ Failure to assess for and provide spinal protection when indicated |
|
|
|
||||||
____ Failure to voice and ultimately provide high concentration oxygen |
|
|
|
||||||
____ Failure to assess/provide adequate ventilation |
|
|
|
|
|
||||
____ Failure to find or appropriately manage problems associated with airway, breathing, hemorrhage or shock
____ Failure to differentiate patient’s need for immediate transportation versus continued assessment/treatment at the scene
____ Performs other assessment before assessing/treating threats to airway, breathing and circulation
____ Failure to manage the patient as a competent EMR
____ Exhibits unacceptable affect with patient or other personnel
____ Uses or orders a dangerous or inappropriate intervention
You must factually document your rationale for checking any of the above critical items on the reverse side of this form.
© 2016 by the National Registry of Emergency Medical Technicians, Inc., Columbus, OH |
|
All materials subject to this copyright may be photocopied for the |
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The EMT Trauma Assessment form is intended to evaluate the skills of Emergency Medical Technicians during patient assessment and management in trauma scenarios. |
| Structure | This assessment is divided into distinct sections including Scene Size-Up, Primary Survey/Resuscitation, History Taking, Secondary Assessment, and Reassessment. |
| Total Points | The form allocates a total of 40 possible points, which are distributed across various assessment tasks. |
| PPE Precautions | Taking or verbalizing appropriate personal protective equipment (PPE) precautions is essential and is worth one point. |
| Critical Criteria | Failures in critical areas, such as airway assessment or timely transport decisions, can lead to detrimental outcomes and are detailed on the form. |
| SAMPLE History | Obtaining a SAMPLE history (Signs, Allergies, Medications, Past medical history, Last oral intake, Events leading to the injury) is crucial for patient assessment. |
| State-Specific Laws | State-specific forms may exist, governed by the state's EMS regulations. Check local laws for details regarding trauma assessment requirements. |
| Patient Priority | Identifying patient priority and making treatment or transport decisions based on calculated Glasgow Coma Scale (GCS) scores is critical. |
| Documentation | It is necessary to document any rationale for checking critical criteria items on the reverse side of the form for accountability and clarity. |
Guidelines on Utilizing Emt Trauma Assessment
Completing the EMT Trauma Assessment form is essential for accurately documenting patient evaluations in emergency situations. Follow these steps carefully to ensure that all relevant information is captured effectively.
- Begin by entering the candidate's name, examiner's name, date, and scenario number at the top of the form.
- Document the actual time started for the assessment.
- Verify the use of appropriate PPE precautions and note this in the designated area.
- Conduct a scene size-up to determine safety, the mechanism of injury, and to request additional EMS assistance if needed.
- Consider stabilization of the spine where appropriate.
- Perform a primary survey by assessing the patient's responsiveness and identifying any chief complaints or life-threatening issues.
- Open and assess the airway, inserting an adjunct if indicated.
- Check for adequate ventilation and manage any injuries that may affect breathing.
- Assess circulation by checking pulse, skin condition, and controlling any major bleeding.
- Make a treatment and transport decision based on the calculated Glasgow Coma Scale (GCS) score.
- Obtain baseline vital signs, including blood pressure, pulse, and respiratory rate.
- Attempt to gather a SAMPLE history from the patient.
- Conduct a secondary assessment of the head, neck, chest, abdomen, and pelvis, including palpation and inspection.
- Assess the lower and upper extremities, noting motor, sensory, and circulatory functions.
- Check the posterior thorax, lumbar, and buttocks areas for any issues.
- Manage any secondary injuries and wounds that may be present.
- Document the actual time ended for the assessment.
- Calculate the total points awarded based on tasks completed.
- If any critical criteria were not met, provide factual documentation on the reverse side of the form.
Once completed, make sure to review the form for accuracy and completeness before submission. Ensure the necessary signatures are obtained to validate the assessment performed.
What You Should Know About This Form
What is the purpose of the EMT Trauma Assessment form?
The EMT Trauma Assessment form is designed to guide emergency medical responders through the process of evaluating and managing trauma patients. It helps ensure that all necessary steps are taken in a systematic manner, promoting patient safety and effective care.
Who uses the EMT Trauma Assessment form?
This form is utilized by emergency medical technicians (EMTs) and emergency medical responders (EMRs) during training and actual emergency response situations. It serves as a checklist to ensure that responders do not overlook critical aspects of patient assessment.
What are the main sections of the form?
The form is divided into several key sections: Scene Size-Up, Primary Survey/Resuscitation, History Taking, Secondary Assessment, and Reassessment. Each section includes specific tasks that responders need to complete or verbalize, ensuring a thorough evaluation of the patient.
What criteria must be met for successful completion of the assessment?
Responders must meet specific criteria outlined in the form. These include initiating transport within a certain time limit, taking necessary precautions, determining scene safety, and managing airway, breathing, and circulation. Failure to meet critical criteria can affect patient outcomes.
How are points awarded on the assessment form?
Points are awarded for various tasks as responders complete them. Each section contains tasks worth specific points, contributing to a total possible score of 40 points. Achieving a high score indicates proficiency in trauma assessment and management.
What happens if an EMT fails to meet a critical criterion?
If an EMT fails to meet a critical criterion, it is necessary to document the rationale on the back of the form. This documentation helps review the assessment and provides insights into areas requiring improvement in future scenarios.
Can the form be used for training purposes?
Yes, the EMT Trauma Assessment form is suitable for training purposes. It helps trainees practice their assessment skills in a structured manner. In addition, it serves as a valuable reference for examiners evaluating the performance of candidates during psychomotor examinations.
How often should EMTs review the assessment form?
Regular review of the assessment form is recommended. Frequent practice helps EMTs stay familiar with the procedures and criteria, allowing them to respond effectively in real-life situations. Using the form as a guide can bolster the confidence and skills of emergency responders.
Common mistakes
Filling out the EMT Trauma Assessment form requires attention to detail. One common mistake is failing to take or verbalize appropriate personal protective equipment (PPE) precautions. Safety is the first priority in any emergency situation. Neglecting to mention this or skipping this step can jeopardize both the responder's and the patient's safety.
Another frequent error occurs during the scene size-up. Responders sometimes rush through this part, not fully determining if the scene is safe. This critical assessment helps ensure that further complications do not arise during the treatment phase. Without establishing a safe environment, both the patient and EMS crews may be at risk.
Additionally, some responders do not adequately assess the mechanism of injury or the nature of the illness. This oversight may lead to mismanagement of the patient’s condition. Understanding the specific circumstances surrounding an injury is vital for effective treatment. Failing to gather this information can hinder proper intervention and delay effective care.
In the primary survey, not recognizing potential life threats can have serious consequences. Some responders may skip assessing the airway, breathing, or circulation adequately. Each of these components plays a critical role in stabilizing the patient. For instance, without opening the airway properly, the chances of successful ventilation decrease dramatically.
There is also a tendency to rush through obtaining baseline vital signs. Vital signs, including blood pressure, pulse, and respiration rate, provide essential data on the patient's stability. Ignoring this step can result in a lack of understanding of the patient's condition, making it difficult to monitor changes over time.
Finally, a major mistake occurs during the secondary assessment when responders fail to comprehensively inspect all areas, including the head, neck, and chest. Omitting any area can leave potential injuries unaddressed and complicate the patient's treatment. It is crucial to complete a thorough assessment to ensure no significant issues are overlooked.
Documents used along the form
The EMT Trauma Assessment form is a critical component in the management of traumatic injuries. However, it is often accompanied by several other documents that contribute to effective patient assessment and care. Each of these documents serves a distinct purpose that ensures a comprehensive approach to trauma management.
- Patient Care Report (PCR) - This document captures detailed information about the patient's condition, treatments administered, and the response to those treatments. The PCR is essential for continuity of care and provides vital information for the receiving medical facility.
- SAMPLE History Form - This acronym stands for Signs, Allergies, Medications, Past medical history, Last oral intake, and Events leading up to the incident. It helps responders gather relevant patient history that can inform treatment decisions.
- Trauma Protocol Checklist - This checklist outlines specific protocols that must be followed in trauma situations. It serves as a guide to ensure that responders do not overlook critical steps in patient care.
- Spinal Precautions Form - This document records the measures taken to protect the spine in cases of suspected spinal injury. It provides a record of spinal stabilization efforts and helps guide further treatment.
- Incident Report - This report documents the circumstances surrounding the call or incident. It includes information about the scene, the mechanism of injury, and any challenges encountered during the response.
- EMS Transfer of Care Form - Used when transferring a patient to a hospital or another medical team, this form contains crucial information about the patient’s condition and the pre-hospital care provided. It ensures that the receiving team is fully informed and prepared to continue care.
In summary, these additional forms and documents are integral to ensuring effective communication and comprehensive care during trauma assessments. They provide the necessary framework for EMTs to deliver high-quality medical assistance while safeguarding patient information and promoting continuity of care.
Similar forms
- EMT Patient Care Report: This document captures the details of the patient’s condition throughout the pre-hospital phase. Like the Trauma Assessment form, it includes vital signs and the interventions performed.
- Pre-Hospital Care Report: Similar in that it records the entire course of patient assessment and treatment, this report emphasizes the chronological narrative of actions taken during emergencies.
- Trauma Record: This document focuses specifically on trauma-related injuries and treatments. It shares the structure of evaluating injury severity and response similar to the Trauma Assessment form.
- Emergency Department Triage Sheet: Emergency department staff use this document to quickly assess patients. It reflects a similar process of determining patient priority and immediate needs.
- Consent for Treatment Form: While primarily focused on legal permissions, it still includes assessment elements, ensuring patients are informed of the care they will receive, akin to the Trauma Assessment process.
- Vital Signs Record: This document logs the patient’s vital indicators such as blood pressure, heart rate, and respiratory rate. It provides a snapshot, similar to the baseline vital signs gathered in the Trauma Assessment.
- Patient History Form: Collecting relevant medical background, this form parallels the SAMPLE history approach in the Trauma Assessment, aiding in thorough patient evaluation.
- Patient Transfer Form: This document is utilized when transferring patients to other facilities. It includes a summary of assessments and treatments, aligning closely with the structure of the Trauma Assessment form.
Dos and Don'ts
When completing the EMT Trauma Assessment form, adhering to best practices is essential to ensure accurate and effective patient assessment. The following list outlines what to do and what to avoid during this process.
- Do: Take or verbalize appropriate PPE precautions before proceeding with the assessment.
- Do: Determine that the scene is safe before approaching the patient.
- Do: Assess the mechanism of injury and the nature of the illness thoroughly.
- Do: Request additional EMS assistance if the situation warrants it.
- Do: Stabilize the spine if there is a potential for spinal injuries.
- Do: Identify the patient's priority and make timely treatment or transport decisions.
- Do: Obtain baseline vital signs, including blood pressure, pulse, and respiration.
- Do: Reassess the patient according to established protocols.
- Don't: Fail to initiate patient transport within the required time limit.
- Don't: Neglect to assess for spinal protection when indicated.
- Don't: Ignore situations that require high concentration oxygen therapy.
- Don't: Underestimate the importance of airway management, breathing, and circulation checks.
- Don't: Conduct other assessments before addressing immediate threats to the patient's airway, breathing, and circulation.
- Don't: Exhibit an unacceptable demeanor towards the patient or other personnel involved.
- Don't: Order or use any potentially dangerous or inappropriate interventions.
- Don't: Provide an incomplete or unclear documentation of assessments and interventions.
Misconceptions
When it comes to the EMT Trauma Assessment form, various misconceptions may arise. Understanding these can help clarify its purpose and functionality. Here are some common myths:
- 1. The form is only for advanced practitioners. This form is designed for Emergency Medical Responders, ensuring that even those with basic training can effectively assess trauma situations.
- 2. It is purely a checklist with no significance. While it provides a structured checklist, each item is critical in ensuring comprehensive patient assessment and management.
- 3. Completing the form guarantees perfect care. The form aids in systematic assessment, but successful patient care ultimately depends on the EMT's experience and decision-making skills.
- 4. It does not change based on patient condition. The assessment is flexible and should adapt to the individual patient's needs and situation encountered.
- 5. Only physical injuries are assessed. The form encourages assessment of physical and vital signs, as well as neurological status and history for a holistic evaluation.
- 6. Reassessment is optional. Reassessing the patient is a crucial step, as conditions may deteriorate, requiring timely intervention.
- 7. Documentation can be done later. Accurate and timely documentation is essential and should be completed thoroughly at the time of assessment.
- 8. The assessment does not need to be communicated to other responders. Effective communication is vital. Sharing findings with additional responders ensures continuity of care.
- 9. The form is rarely used in real-life scenarios. In fact, the EMT Trauma Assessment form is a fundamental tool used frequently in emergency situations to guide assessment and management.
Each misconception reflects a misunderstanding of the role this form plays in ensuring patient safety and quality care. By addressing these myths, those in the medical field can better appreciate the importance and applicability of the EMT Trauma Assessment form in real-world scenarios.
Key takeaways
Filling out the Emergency Medical Technician (EMT) Trauma Assessment form is a critical task that supports effective patient evaluation and management. Here are key takeaways for EMTs to consider:
- Scene Size-Up: Always begin with a thorough assessment of the scene. Ensuring that the environment is safe is essential before proceeding with patient care.
- PPE Precautions: The use of personal protective equipment (PPE) is crucial for both the EMT and the patient. Verbalizing and demonstrating the use of appropriate PPE is a fundamental first step.
- Primary Survey Importance: Conduct a primary survey to identify life-threatening conditions. Assessing airway, breathing, and circulation must be completed swiftly and efficiently.
- Vital Signs: Obtaining baseline vital signs is necessary for effective patient assessment. This data, which includes blood pressure, pulse, and respiration rate, guides treatment decisions.
- Secondary Assessment: Perform a detailed secondary assessment for additional injuries. This assessment covers multiple body areas and includes visual inspections and palpations to identify problems that may not be immediately apparent.
- Reassessment Protocol: Conduct subsequent reassessments as needed. Being able to monitor the patient’s condition over time is essential to adapting care plans appropriately.
In summary, the EMT Trauma Assessment form is structured to enhance the efficiency and effectiveness of patient care. Following these takeaways promotes thorough evaluation and improves outcomes for trauma patients.
Browse Other Templates
Public Authority San Bernardino - Remember to print everything legibly on the form.
Llc in Tennessee Cost - Proper completion of this form facilitates accurate state records regarding business entities.
How Do I Find Out How Much I Owe the Ohio Attorney General - Individuals or businesses must provide consent for information regarding debts certified for collection by the Attorney General.