Fill Out Your Enrollment Promise Form
The Enrollment Promise form is essential for healthcare providers in Pennsylvania seeking enrollment in the state's Medicaid program. This application ensures that the necessary data about the provider is accurately collected and evaluated. Each application must be completed meticulously, using either a typed format or black ink, as improper submissions will result in rejection. Applicants, whether individuals or facilities, must provide their complete names, details about their services, and unique identifiers, such as their National Provider Identifier (NPI) number. Important steps include specifying whether the application is for initial enrollment, revalidation, or reactivation, along with submitting supporting documents that validate licensing, specialty types, and various tax identification numbers. Applicants must also disclose personal information such as their Social Security number and contact details. Furthermore, the form requires an acknowledgment of participation with Medicare and Medicaid Managed Care Organizations (MCOs), while ensuring compliance with the Americans with Disabilities Act (ADA). Providing a clear and correct service location is crucial, as is confirming the nature of the business. Ultimately, successful completion of the Enrollment Promise form guarantees providers access to reimbursement for care and services rendered to consumers within the Medicaid program, thereby reinforcing their commitment to health service delivery within the community.
Enrollment Promise Example
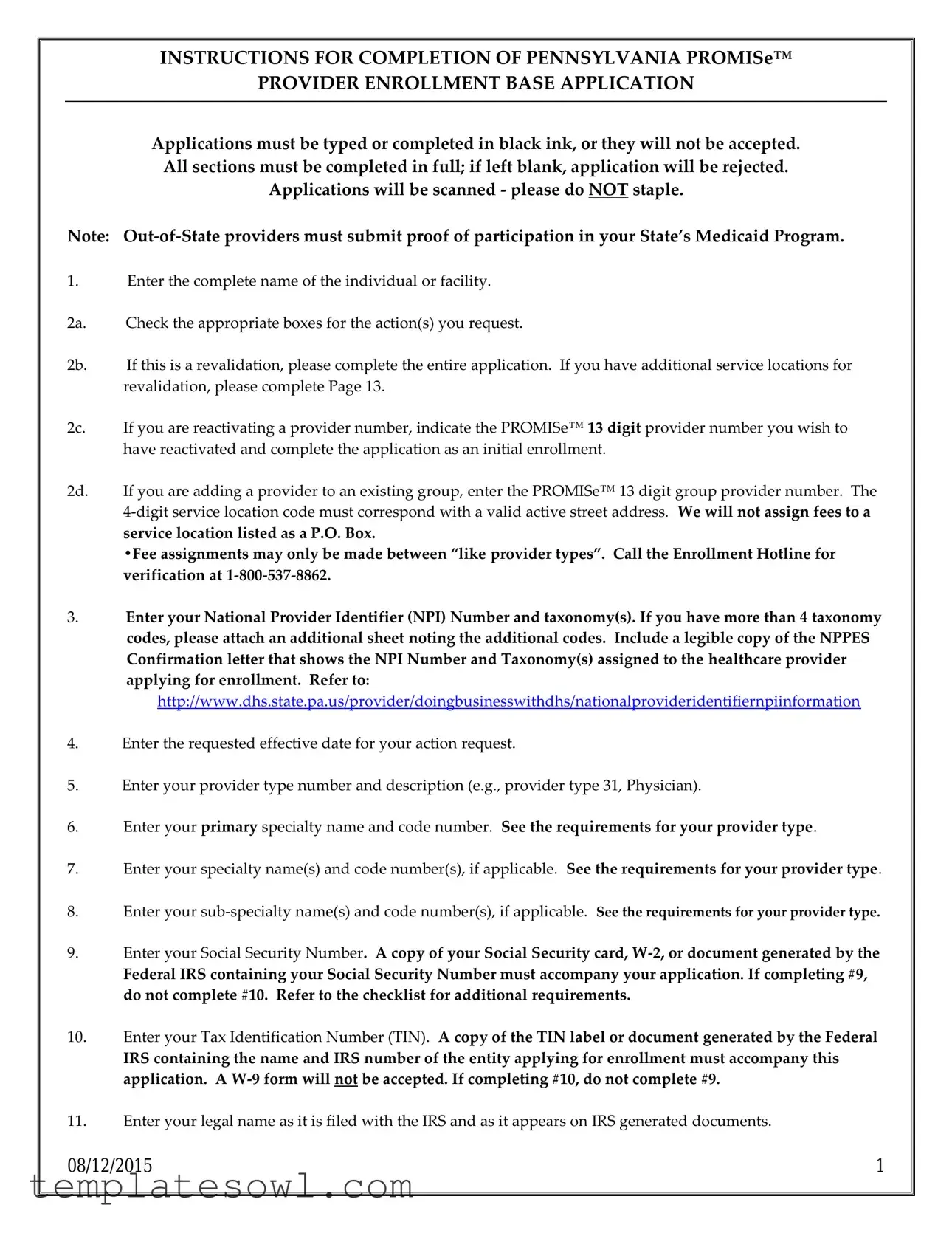
INSTRUCTIONS FOR COMPLETION OF PENNSYLVANIA PROMISe™
PROVIDER ENROLLMENT BASE APPLICATION
Applications must be typed or completed in black ink, or they will not be accepted. All sections must be completed in full; if left blank, application will be rejected.
Applications will be scanned - please do NOT staple.
Note:
1.Enter the complete name of the individual or facility.
2a. Check the appropriate boxes for the action(s) you request.
2b. If this is a revalidation, please complete the entire application. If you have additional service locations for revalidation, please complete Page 13.
2c. If you are reactivating a provider number, indicate the PROMISe™ 13 digit provider number you wish to have reactivated and complete the application as an initial enrollment.
2d. If you are adding a provider to an existing group, enter the PROMISe™ 13 digit group provider number. The
service location listed as a P.O. Box.
•Fee assignments may only be made between “like provider types”. Call the Enrollment Hotline for verification at
3.Enter your National Provider Identifier (NPI) Number and taxonomy(s). If you have more than 4 taxonomy codes, please attach an additional sheet noting the additional codes. Include a legible copy of the NPPES Confirmation letter that shows the NPI Number and Taxonomy(s) assigned to the healthcare provider applying for enrollment. Refer to:
http://www.dhs.state.pa.us/provider/doingbusinesswithdhs/nationalprovideridentifiernpiinformation
4.Enter the requested effective date for your action request.
5.Enter your provider type number and description (e.g., provider type 31, Physician).
6.Enter your primary specialty name and code number. See the requirements for your provider type.
7.Enter your specialty name(s) and code number(s), if applicable. See the requirements for your provider type.
8.Enter your
9.Enter your Social Security Number. A copy of your Social Security card,
Federal IRS containing your Social Security Number must accompany your application. If completing #9, do not complete #10. Refer to the checklist for additional requirements.
10.Enter your Tax Identification Number (TIN). A copy of the TIN label or document generated by the Federal
IRS containing the name and IRS number of the entity applying for enrollment must accompany this application. A
11.Enter your legal name as it is filed with the IRS and as it appears on IRS generated documents.
08/12/2015 |
1 |
12a. Indicate whether or not you participate with any Pennsylvania Medicaid Managed Care Organizations (MCOs).
12b. Enter the names of any Pennsylvania Medicaid Managed Care Organizations with which you participate.
13a. Indicate whether the provider operates under a fictitious
13b. If applicable, enter the statement/permit number and the name. Attach a legible copy of the
recorded/stamped fictitious business name statement/permit.
14.Enter your date of birth.
15.Enter your gender.
16.Enter the title/degree you currently hold.
17a. Enter your IRS address. This address is where your 1099 tax documents will be sent.
18.Check the appropriate box for the business type of the individual or facility applying for enrollment. Check 1 box only. Include corporation papers from the Department of State Corporation Bureau or a copy of your business partnership agreement, if applicable.
20.Enter your Drug Enforcement Agency (DEA) Number (if applicable).
*A copy of your DEA certificate must be included with the application.
21.If you have a CLIA certificate and a Dept. of Health Laboratory Permit associated with this service location. *A copy of both documents must be included with the application.
22.Enter your CMS number.
23a. Enter a valid service location address. The address must be a physical location, not a post office box. The zip code must contain 9 digits and the phone number must be for the service location. Refer to block #27 of the application to list an additional address (es) for
Please indicate if the physical address is handicap accessible Please indicate if the physical address is an FQHC or RHC location
Please indicate if the physical address has been screened by one of the listed entities
NOTE* you can sign up for the Electronic Funds Transfer Direct Deposit Option by following the link below:
http://www.dhs.state.pa.us/provider/doingbusinesswithdhs/electronicfundstransferdirectdepositinformation
23b. Answer question, if yes, enter your
23c. If you wish Medicare claims to crossover to this service location check this box. Note: This crossover can be
added to only one service location.
08/12/2015 |
2 |
23h. Indicate whether you or your staff is able to communicate with patients in any language other than English.
23i. If applicable, list the additional languages in which you or your staff can communicate.
23j. Enter the appropriate Provider Eligibility Program(s) (PEP(s)). Refer to the PEP Descriptions and the
requirements for your provider type.
If you answer “Yes” to any of the questions, you must provide a detailed explanation (on a separate piece of paper) and attach it to your application. (Refer to the Confidential Information sheet).
25.Sign the application and print your name, title, and date (The signature should be that of the individual applying for enrollment or someone able to represent the facility applying for enrollment). Use black ink.
26. This page, beginning with block #26, may be used to add a
previously defined service location address listed in 23a. This sheet cannot be used to add a service location.
26a. Enter the corresponding
26b. Indicate whether you are adding a
26c. Enter the
•Use page 13 to add additional service locations upon the INITIAL ENROLLMENT OF AN INDIVIDUAL.
•Facilities must complete a new base application to add additional service locations to their file.
•The individual applying for enrollment or a representative of the facility applying for enrollment must complete the Provider Agreement included with the application.
When completed, review the “Did You Remember…” Checklist included with the application.
Return your application and other documentation to the address listed on the requirements for your specific provider type.
If no address is listed on the requirements for your specific provider type/specialty, please submit to:
DHS Provider Enrollment
PO Box 8045
Harrisburg, PA
- or -
Fax: (717)
- or -
Email:
08/12/2015 |
3 |
ATTENTION
Fax completed application to ODP- ID @
Office of Developmental Programs - ID
Room 413 Health and Welfare Building
Harrisburg, PA 17101
Attn: Provider Enrollment
ATTENTION OLTL PROVIDERS: Mail completed applications to:
Office of Long Term Living
Bureau of Quality and Provider Management
Division of Provider and Operations Management
555 Walnut Street
P.O. Box 8025
Harrisburg, PA
THIS SPACE INTENTIONALLY LEFT BLANK
08/12/2015 |
4 |
Provider Eligibility Program (PEP) Descriptions
A Provider Eligibility Program code identifies a program for which a provider may apply. A provider must be approved in that program to be reimbursed for services to beneficiaries of that program. Providers should use the following PEP codes when enrolling in Medical Assistance (MA). Providers should use the descriptions in this document to determine which PEP code to use when enrolling in MA.
ACT 150 Program
Office of Long Term Living - (800)
This program provides services to eligible persons with physical disabilities in order to prevent institutionalization and allows them to remain as independent as possible. The ACT 150 Program is operated only with State funds.
Eligibility:
Recipients either do not meet the level of care for a federally supported waiver or do not meet the financial limitations for the Attendant Care Waiver.
Services:
Personal Assistance Services
Personal Emergency Response System
Service Coordination
Adult Autism Waiver (AAW)
Bureau of Autism Services - (866)
The AAW is designed to provide
Eligibility:
Recipients must be 21 or older and have a diagnosis of ASD and meet certain diagnostic, functional and financial eligibility criteria.
Services:
Assistive Technology
Behavioral Specialist
Community Inclusion and Community Transition
Counseling
Day Habilitation
Environmental Modifications
Family Counseling and Family Training
Job Assessment and Job Finding
Nutritional Consultation
Occupational Therapy
Residential Habilitation
Respite
Speech Therapy
Supported Employment
Supports Coordination
Temporary Crisis Services
Transitional Work Services
08/12/2015 |
5 |
Aging Waiver (formerly PDA Waiver/Bridge Program)
Office of Long Term Living - (800)
This program provides services to eligible persons over the age of 60 in order to prevent institutionalization and allows them to remain as independent as possible.
Eligibility:
Recipients must be 60 years of age or older, meet the level of care needs for a Skilled Nursing Facility, and meet the financial requirements as determined by the County Assistance Office (CAO).
Services:
Accessibility Adaptation
Adult Daily Living
Community Transition Services
Home Delivered Meals
Home Health
Personal Assistance Services
Personal Emergency Response System
Respite
Service Coordination
Specialized Medical Equipment and Supplies
Telecare Services
Therapeutic and Counseling Services
Transition Service Coordination
AIDS Waiver
Office of Long Term Living - (800)
This is a federally approved special program which allows the Commonwealth of Pennsylvania to provide certain home and
Eligibility:
Categorically and medically needy recipients may be eligible if they are diagnosed as having AIDS or symptomatic HIV disease, are certified by a physician and recipient as needing an intermediate or higher level of care and the cost of services under the waiver does not exceed alternative care under the regular MA Program.
MA recipients who are enrolled in a managed care organization (MCO) or an MA Hospice Program are not eligible to participate in this home and
Services:
Homemaker services
Nutritional consultations by registered dietitians
Supplemental skilled nursing visits
Supplemental home health aide visits
Supplies not covered by the State Plan
Attendant Care Waiver
Office of Long Term Living - (800)
This program provides services to eligible persons with physical disabilities in order to prevent institutionalization and allows them to remain as independent as possible.
Eligibility:
Recipients must be between the ages
08/12/2015 |
6 |
Services:
Community Transition Services
Personal Assistance Services
Personal Emergency Response System
Service Coordination
Transition Service Coordination
Behavioral Health HealthChoices (Beh Hlth HC)
Office of Mental Health and Substance Abuse Services - (800)
This PEP is used to identify providers who are approved to serve recipients enrolled exclusively in HealthChoices.
Eligibility:
Recipients are HealthChoices only eligible;
Provider must contract with the contracted County or Contracted Behavioral Health Managed Care Organization
Licensed/certified/approved service description and credentialed by the contracted County or
Requires written
Used exclusively by OMHSAS
Services:
Alternative treatment services which are discretionary,
Contact contracted County or
Community Care Waiver (COMMCARE)
Office of Long Term Living - (800)
This program was designed to prevent institutionalization of individuals with traumatic brain injury (TBI) and to allow them to remain as independent as possible.
Eligibility:
Pennsylvania residents age 21 and older who experience a medically determinable diagnosis of traumatic brain injury and require a Special Rehabilitative Facility (SRF) level of care. Traumatic brain injury is defined as a sudden insult to the brain or its coverings, not of a degenerative, congenital or
Services:
Accessibility Adaptations
Adult Daily Living
Community Integration
Community Transition Services
Home Health
Personal Assistance Services
Personal Emergency Response System
Prevocational Services
Residential Habilitation
Respite
Service Coordination
Specialized Medical Equipment and Supplies
Structured Day
Supported Employment
Therapeutic and Counseling Services
Transition Service Coordination
08/12/2015 |
7 |

Consolidated Community Reporting Initiative Performance Outcome Management System (EPOMS)
Office of Mental Health and Substance Abuse Services - (800)
This PEP is used to identify providers who are approved to serve county
Eligibility:
Recipients are
Providers do not receive payment through the MMIS (encounter data reporting only);
The PEP can be added to an independent service location; in conjunction with a Beh Hlth HC or FFS PEP;
Provider must contract with the County Mental Health Office;
Licensed/certified/service description and approved by the County Mental Health Office;
Requires written
Used exclusively by OMHSAS
Services:
All county funded providers must enroll at the appropriate service location for the county rendered service;
Contact contracted County Mental Health Office for definition of services
Consolidated Waiver
Office of Developmental Programs - (866)
The Consolidated Waiver is a Home and
The Pennsylvania Consolidated Waiver is designed to help individuals with an intellectual disability to live more independently in their homes and communities and to provide a variety of services that promote community living, including
Services:
Assistive technology
Behavioral support
Companion
Education support
Home accessibility adaptations
Home and community habilitation (unlicensed)
Homemaker/chore
Licensed day habilitation
Nursing
Prevocational
(Licensed) residential habilitation
(Unlicensed) residential habilitation
Respite
Specialized supplies
Supported employment
Supports broker
Supports coordination
Therapy (physical, occupational, visual/mobility, behavioral and speech and language)
Transitional work
Transportation
Vehicle accessibility adaptations
08/12/2015 |
8 |
Early Intervention (WAV15)
Office of Child Development and Early Learning - (717)
Eligibility:
Infants and toddlers age birth to age 3 who have a 25% delay in one or more areas of development when compared to other children of the same age, or a physical disability such as hearing or vision loss, or informed clinical opinion that the child has a delay or the child has known physical or mental conditions which have high probability for development delays. Infants and toddlers also meet the Medical Assistance requirements.
Services:
Early Intervention supports and services are designed to meet the developmental needs of children with a disability as well as the needs of the family related to enhancing the child’s development in one or more of the following areas:
Physical development, including vision and hearing
Cognitive development
Communication development
Social or emotional development
Adaptive development
EI Base Funds (WAV16)
Office of Child Development and Early Learning - (717)
Eligibility:
Infants and toddlers age birth to age 3 who have a 25% delay in one or more areas of development when compared to other children of the same age, or a physical disability such as hearing or vision loss, or informed clinical opinion that the child has a delay or the child has known physical or mental conditions which have high probability for development delays.
Services:
Early Intervention supports and services are designed to meet the developmental needs of children with a disability as well as the needs of the family related to enhancing the child’s development in one or more of the following areas:
Physical development, including vision and hearing
Cognitive development
Communication development
Social or emotional development
Adaptive development
Office of Medical Assistance Programs - (800)
The traditional delivery system of the Medical Assistance (MA) program which provides payment on a
Eligibility:
All MA Recipients.
Services:
Behavioral health services
Inpatient services
Outpatient services
Physical health services
08/12/2015 |
9 |
Healthy Beginnings Plus
Office of Medical Assistance Programs - (800)
Healthy Beginnings Plus is Pennsylvania’s effort to assist
Eligibility:
Pregnant women who elect to participate in Healthy Beginnings Plus.
Services:
Childbirth and parenting classes
Home health services
Nutritional and psychosocial counseling
Other individualized client services
Smoking cessation counseling
Independence Waiver
Office of Long Term Living - (800)
This program provides services to eligible persons with physical disabilities in order to prevent institutionalization and allows them to remain as independent as possible.
Eligibility:
Recipients must be 18 years of age and older, suffer from severe physical disability which is likely to continue indefinitely and results in substantial functional limitations in three or more major life activities. Recipients must be eligible for nursing facility services, the primary diagnosis cannot be a mental health diagnosis or mental retardation, and the recipients cannot be ventilator dependent.
Services:
Accessibility Adaptation
Adult Daily Living
Community Integration
Community Transition Services
Home Health
Personal Assistance Services
Personal Emergency Response System
Respite
Service Coordination
Specialized Medical Equipment and Supplies
Supported Employment
Therapeutic and Counseling Services
Transition Service Coordination
08/12/2015 |
10 |
Form Characteristics
| Fact Name | Description |
|---|---|
| Application Format | Applications must be typed or completed in black ink. Any other formats will not be accepted. |
| Participation Verification | Out-of-state providers must provide proof of participation in their state's Medicaid Program to be eligible. |
| Provider Number Reactivation | If reactivating a provider number, include the 13-digit PROMISe™ provider number on your application. |
| NPI Requirements | Enter your National Provider Identifier (NPI) Number and taxonomy codes. Attach the NPPES confirmation letter for verification. |
| Social Security Number | Provide a Social Security Number and include documentation like a card or W-2. Do not complete the TIN section if this is included. |
| Legal Name Requirement | Your legal name must match how it is filed with the IRS and must be presented on IRS-generated documents. |
| Business Type Indication | The application requires you to check the appropriate box to indicate the business type applying for enrollment. |
| Provider Eligibility Programs | Providers can enroll in specific Provider Eligibility Programs (PEPs). Approval in a PEP is necessary for reimbursement. |
Guidelines on Utilizing Enrollment Promise
Once the Enrollment Promise form is filled out completely, it must be submitted for processing. Be sure to gather any necessary documents to accompany the form. This includes identification numbers, licenses, and other required paperwork. After the submission, the relevant authorities will review the application.
- Start by entering the complete name of the individual or facility.
- Check the boxes corresponding to the actions you are requesting on the form.
- If revalidating, complete the entire form. For additional service locations, refer to Page 13.
- If reactivating a provider number, provide the 13-digit PROMISe™ provider number and fill out the application as if it’s an initial enrollment.
- If adding a provider to an existing group, enter the PROMISe™ group provider number and ensure the 4-digit service location code matches an active street address—P.O. Box addresses are not allowed for fees.
- Enter your National Provider Identifier (NPI) Number and taxonomy(s). If you have more than four taxonomy codes, include an extra sheet with these details.
- Attach a clear copy of the NPPES Confirmation letter showing your NPI Number and Taxonomy(s).
- Provide the requested effective date for the action.
- Add your provider type number and description.
- Enter your primary specialty name and code number.
- If applicable, enter any additional specialty and sub-specialty names and code numbers.
- Provide your Social Security Number. Include a copy of your Social Security card, W-2, or another IRS-generated document along with your application.
- Enter your Tax Identification Number (TIN) and include a document from the IRS showing this number. Do not use a W-9 form.
- Write your legal name as it appears on IRS filings.
- Indicate if you participate with any Pennsylvania Medicaid Managed Care Organizations (MCOs) and provide their names if applicable.
- State whether you operate under a fictitious business name and provide any required documentation.
- Provide your date of birth and gender.
- Indicate the title or degree you hold.
- Enter your IRS address where 1099 tax documents will be sent.
- Add your contact information associated with the IRS address.
- Check the appropriate box for your business type and include any applicable corporation or partnership documents.
- Enter your license number, issuing state, issue date, and expiration date if necessary. Attach a copy of your license.
- If applicable, enter your Drug Enforcement Agency (DEA) Number and include a copy of your DEA certificate.
- If you have a CLIA certificate and a Dept. of Health Laboratory Permit, attach copies of these documents.
- Provide your CMS number and attach your CMS certification.
- Enter a valid service location address, ensuring it is not a P.O. Box. Include the 9-digit zip code and service location phone number.
- Provide your email address if applicable, and note if you wish for Medicare claims to crossover to this service location.
- Fill in additional contact information as needed.
- State if you or your staff can communicate with patients in other languages and list these languages if so.
- Complete the questions regarding the Americans with Disabilities Act (ADA).
- Identify any Provider Eligibility Program(s) (PEP) you’re applying for.
- Indicate if you retain managing employees or agents and complete the necessary attachment if applicable.
- Answer all confidential information questions thoroughly, including any necessary explanations.
- Sign the application using black ink and print your name, title, and date.
- Use Page 27 to include any additional mail-to, pay-to, or home office addresses if needed.
- Complete the Provider Agreement included with the application.
- Review the "Did You Remember…" checklist and gather all required documentation.
- Finally, send the completed application and supporting documents to the specified address for your provider type.
What You Should Know About This Form
What is the Enrollment Promise form?
The Enrollment Promise form is a base application used for enrolling providers in Pennsylvania's PROMISe™ system. This system enables healthcare providers to participate in the Medicaid program and receive reimbursements for services rendered to eligible clients. Completing this form accurately and thoroughly is essential for successful enrollment.
Who needs to complete the Enrollment Promise form?
Any individual or facility that wishes to become a Medicaid provider in Pennsylvania must complete this form. This includes healthcare practitioners, group practices, and organizations that provide services covered by Medicaid. If you are reactivating a provider number or adding a provider to an existing group, you will also need to submit this form.
What information do I need to provide on the form?
The form requires detailed information about the applicant and the services to be provided. Key details include your legal name, National Provider Identifier (NPI) number, social security number, business type, and service location address. You will also need to provide documentation, such as copies of licenses and certifications, depending on your provider type.
How should I fill out the Enrollment Promise form?
It's crucial to complete the Enrollment Promise form in black ink or by typing to ensure it can be scanned properly. Avoid using staples, as it may hinder processing. Follow the instructions carefully and make sure to check all required boxes. If necessary, attach additional sheets for any extra information, such as taxonomy codes or additional service locations.
What should I do if I have questions while filling out the form?
If you have questions as you complete the form, you can call the Enrollment Hotline at 1-800-537-8862 for verification and support. They can help clarify any uncertainties regarding specific sections or requirements, ensuring that your application is filled out correctly.
What happens after I submit the Enrollment Promise form?
After submitting the Enrollment Promise form along with any required documentation, your application will be reviewed by the appropriate authorities. You will receive confirmation of your enrollment status. Depending on your provider type and the accuracy of your submission, this process may take some time, so patience is appreciated.
Common mistakes
Filling out the Enrollment Promise form can be a daunting task, and many applicants make mistakes that could delay their enrollment or result in a denial. Here are six common pitfalls to watch out for when completing this important document.
One major mistake is not using the proper writing method. The instructions state that applications must be typed or completed in black ink. Failure to follow this directive could lead to rejection of the application. It's a small detail, but it’s critical for the scanning process that comes next.
Another frequent error involves the service location address. Many individuals mistakenly list a P.O. Box instead of a physical address, which is explicitly against the rules. The application needs a valid street address corresponding to a service location, as the form will not recognize fees assigned to a P.O. Box. Double-checking this detail can save a lot of trouble down the line.
Inadequate documentation often leads to applications being sent back. For instance, if you enter your Social Security Number, you must also provide a copy of your Social Security card, W-2, or other IRS documents. If this documentation is omitted, it will result in delays while the application is reviewed or resubmitted.
Many applicants also forget to enter their National Provider Identifier (NPI) Number and taxonomy codes. If you have more than four taxonomy codes, ensure that you attach an additional sheet clearly listing those codes, along with a legible copy of your NPPES Confirmation letter. Omitting even one of these pieces could halt progress.
It’s also easy to overlook your effective date, which many people skip. Entering a requested effective date is not just a formality; it directly affects when your services can begin. Providing a clear and accurate date could mean the difference between getting started quickly or having to wait substantially longer.
Finally, many applicants underestimate the importance of the signature. This application must be signed in black ink by the individual applying for enrollment or an authorized representative from the facility. An unsigned application leads to automatic rejection, making it one of the simplest yet most costly mistakes to make. Taking the time to review the application before submission can help ensure that it is filled out correctly and completely.
Documents used along the form
The Enrollment Promise form is a crucial document for healthcare providers looking to enroll in Pennsylvania's Medicaid program. However, several other documents support the enrollment process and provide additional information or verification. Understanding these documents can streamline the enrollment journey, ensuring that all necessary information is readily available.
- NPPES Confirmation Letter: This letter is proof of the provider's National Provider Identifier (NPI) number and taxonomy codes. It is essential to confirm that the healthcare provider is registered with the National Plan and Provider Enumeration System and holds an appropriate classification to provide services.
- Social Security Documentation: To validate identity, a copy of the Social Security card, W-2 form, or federal IRS document containing the Social Security Number is required. This documentation ensures that the individual's identity can be verified accurately through official channels.
- Tax Identification Number (TIN) Documentation: Providers must submit a document generated by the IRS that confirms their TIN, ensuring compliance with federal tax regulations. A W-9 form is not acceptable, emphasizing the need for specific documentation to accompany the application.
- Fictitious Business Name Statement: If a provider operates under a name different from their legal name, they must include a legible copy of the recorded or stamped fictitious business name statement. This document clarifies the provider's identity in relation to the services offered.
Collectively, these supporting documents enhance the completeness of the Enrollment Promise form, facilitating a smoother enrollment process in Pennsylvania's Medicaid program. By preparing these documents ahead of time, providers can reduce delays and ensure that they meet all eligibility criteria.
Similar forms
- Provider Enrollment Application: Similar to the Enrollment Promise form, this application also requires detailed personal and professional information from healthcare providers to establish their eligibility to participate in Medicaid and related programs. Both forms ask for certifications and licenses, ensuring that providers meet necessary standards.
- Medicaid Provider Agreement: This document outlines the terms and conditions under which a provider will participate in the Medicaid program. Like the Enrollment Promise form, it includes sections that must be filled out accurately and may require accompanying documents like W-9 forms and licenses.
- National Provider Identifier (NPI) Application: Providers must complete this application to obtain their unique NPI number. Similar to the Enrollment Promise form, it collects identifying information and serves as a prerequisite for participating in health programs.
- CLIA Certificate Application: This application is necessary for laboratories providing testing services. Both forms emphasize the need for proper documentation and proof of compliance with various regulatory requirements.
- DEA Registration Form: Providers must complete this form to handle controlled substances. Just as with the Enrollment Promise, detailed identifying information is required, along with supporting documentation for compliance purposes.
- Provider Revalidation Application: This is used when a provider must confirm their information periodically. It, too, mirrors the Enrollment Promise in terms of the comprehensive detail required for continued participation in Medicaid programs.
- Home and Community-Based Services (HCBS) Waiver Application: This form is for providers wishing to offer services under specific waivers. Just like the Enrollment Promise, it asks for extensive service details along with proof of qualifications.
- Managed Care Organization (MCO) Participation Agreement: Similar in function to the Enrollment Promise form, this agreement allows providers to deliver services to beneficiaries of specific MCOs, ensuring compliance and service standards are met.
- Pennsylvania Medicaid Managed Care Enrollment Packet: This packet collects similar information regarding provider qualifications, required documentation, and specific service offerings, focusing on Medicaid’s managed care format.
Dos and Don'ts
- Do: Ensure that your application is typed or filled out in black ink. Applications completed in other colors will be rejected.
- Do: Include all necessary documents, like the Social Security card and tax identification number, with your application.
- Do: Provide the complete legal name as it appears on IRS documents.
- Do: Review the Did You Remember… Checklist to verify that you have completed all parts of the application.
- Don’t: Staple any documents together, as applications will be scanned and staple marks could interfere with that process.
- Don’t: Enter a post office box as your service location address. A physical address is required.
- Don’t: Submit a W-9 form as your Tax Identification Number documentation. Only IRS-generated documents will be accepted.
- Don’t: Forget to sign and date your application before submission; signatures must be in black ink.
Misconceptions
Many individuals have misunderstandings about the Enrollment Promise form used for Pennsylvania PROMISe™ provider enrollment. Here are some of the common misconceptions along with clarifications:
- All providers can apply without any prerequisites. In reality, out-of-state providers must provide proof of participation in their own state’s Medicaid Program before completing the form.
- It is acceptable to submit applications that are hand-written. Applications must be typed or filled out in black ink. Failure to do so will result in rejection of the application.
- You can staple documents together when submitting your application. Stapling is not allowed as applications will be scanned. Documents should be submitted flat, without any fasteners.
- There is no need to include supporting documents with the application. Supporting documents, such as a copy of your Social Security card or your license, must accompany the application to ensure it is complete.
- All service locations can be listed as P.O. Box addresses. A physical street address is required. Applications listing a P.O. Box will not be accepted.
- Once submitted, there is no way to modify the application. If changes are needed, it is essential to follow up accordingly. The process allows further communication to correct any details with the application.
Key takeaways
Here are some key takeaways about filling out and using the Enrollment Promise form:
- Complete and Clear Information: Always fill out your application with complete details. Use black ink, and avoid stapling the application.
- Out-of-State Providers: If you're from outside Pennsylvania, remember to include proof of participation in your home state’s Medicaid Program.
- Application Actions: Be specific when indicating the actions you request, such as revalidation or adding new service locations. Fill out all relevant pages according to your situation.
- Documentation Requirements: Attach required documents like your Social Security card, Tax Identification Number documentation, and any licenses or certifications that apply.
- Physical Address Needed: Ensure that the service location address is a valid physical address. P.O. Boxes are not acceptable.
- Specialty Codes: Provide your specialty and sub-specialty codes when applicable, following the specific requirements for your provider type.
- Review Before Submission: Use the included checklist to confirm that you have provided all the necessary information and documents before sending your application.
Browse Other Templates
10-1 Areas of Parallelograms and Triangles Worksheet Answers - Working through these exercises will build a solid foundation in geometry.
Da3078 - This form is prevalent in various branches of the military, ensuring uniform clothing standards are maintained.
Patent Application Form Pdf - The electronic filing system allows for efficient submission of the ADS.