Fill Out Your Envision Rx Prior Auth Form
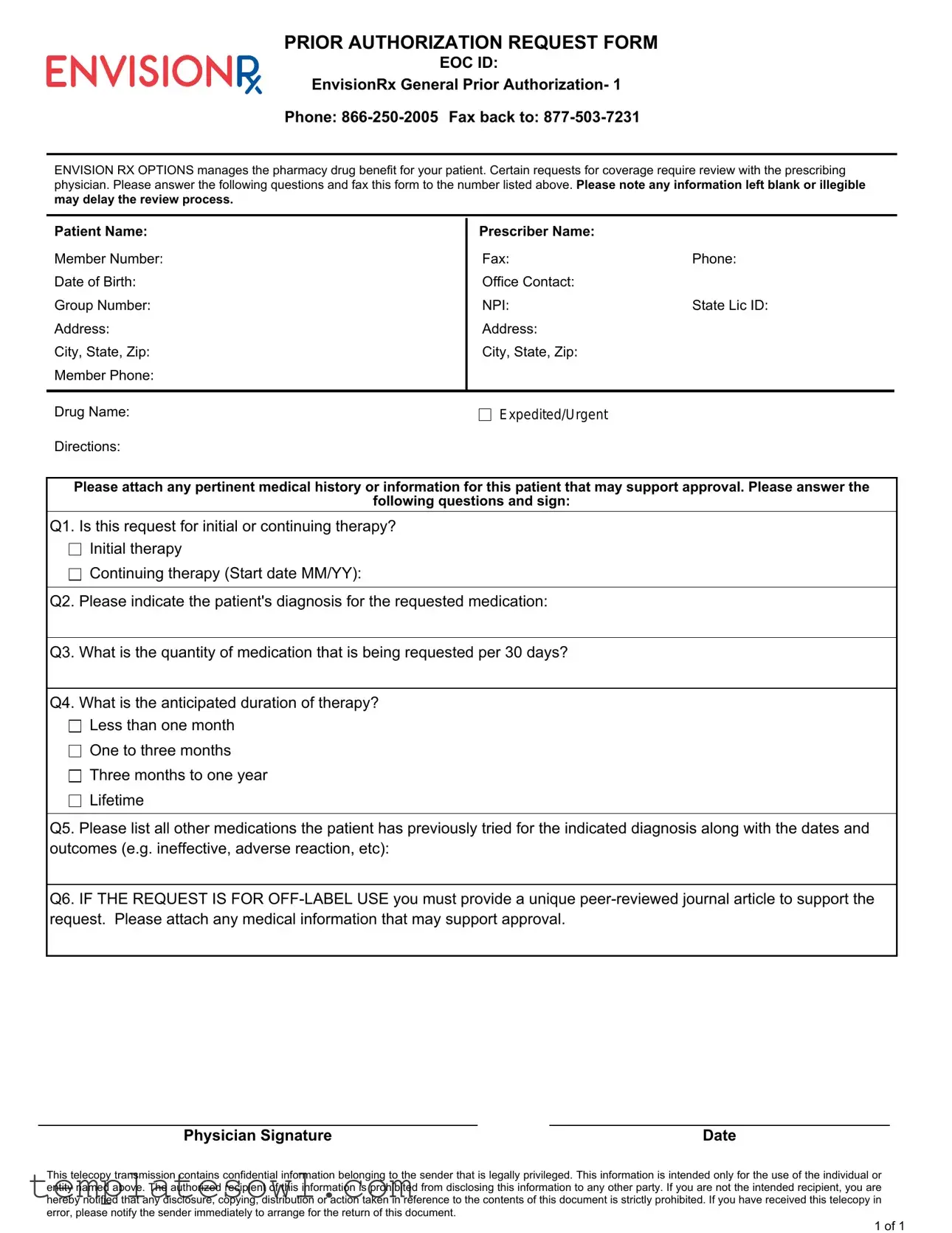
The Envision Rx Prior Authorization Request Form serves as a crucial tool for healthcare providers seeking coverage for specific medications under the EnvisionRx pharmacy drug benefit program. This form necessitates detailed information, requiring the inclusion of essential patient and prescriber identification data such as names, member numbers, addresses, and contact details. It addresses various pivotal aspects of the medication request, including whether the therapy is initial or ongoing, the patient's diagnosis, and the quantity of medication being sought monthly. Furthermore, it obligates providers to enumerate any previous treatments the patient has undergone, noting outcomes to substantiate the need for the requested drug. If the request involves off-label use, the submission of a relevant peer-reviewed journal article is mandatory. Completeness is vital; omitting any information or providing illegible responses can significantly delay the authorization process. This application form must be faxed to the designated number, ensuring all necessary attachments, like pertinent medical history, accompany the request. This structured approach aims to streamline the approval workflow, granting patients access to essential medications while maintaining the integrity of the review process.
Envision Rx Prior Auth Example
PRIOR AUTHORIZATION REQUEST FORM
EOC ID:
EnvisionRx General Prior Authorization- 1
Phone:
ENVISION RX OPTIONS manages the pharmacy drug benefit for your patient. Certain requests for coverage require review with the prescribing physician. Please answer the following questions and fax this form to the number listed above. Please note any information left blank or illegible may delay the review process.
Patient Name:
Member Number:
Date of Birth:
Group Number:
Address:
City, State, Zip: Member Phone:
Prescriber Name: |
|
Fax: |
Phone: |
Office Contact: |
|
NPI: |
State Lic ID: |
Address: |
|
City, State, Zip: |
|
Drug Name: |
Expedited/Urgent |
Directions:
Please attach any pertinent medical history or information for this patient that may support approval. Please answer the
following questions and sign:
Q1. Is this request for initial or continuing therapy?
Initial therapy
Continuing therapy (Start date MM/YY):
Q2. Please indicate the patient's diagnosis for the requested medication:
Q3. What is the quantity of medication that is being requested per 30 days?
Q4. What is the anticipated duration of therapy?
Less than one month
One to three months
Three months to one year
Lifetime
Q5. Please list all other medications the patient has previously tried for the indicated diagnosis along with the dates and outcomes (e.g. ineffective, adverse reaction, etc):
Q6. IF THE REQUEST IS FOR
Physician Signature |
Date |
This telecopy transmission contains confidential information belonging to the sender that is legally privileged. This information is intended only for the use of the individual or entity named above. The authorized recipient of this information is prohibited from disclosing this information to any other party. If you are not the intended recipient, you are hereby notified that any disclosure, copying, distribution or action taken in reference to the contents of this document is strictly prohibited. If you have received this telecopy in error, please notify the sender immediately to arrange for the return of this document.
1 of 1
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | This Prior Authorization Request Form is used to obtain approval for specific medications managed by Envision Rx Options, ensuring that requests are assessed appropriately by healthcare providers. |
| Contact Information | The form provides essential contact details, including a phone number (866-250-2005) for inquiries and a fax number (877-503-7231) to submit completed forms. |
| Patient Information | Patients must provide personal details, such as their name, date of birth, and contact information, to facilitate accurate processing of their request. |
| Prescriber Details | Healthcare providers must include their professional details, including their name, contact information, and NPI (National Provider Identifier), which helps in identifying them in the system. |
| Required Questions | The form includes critical questions about therapy type, medication quantity, treatment duration, and previous medications tried, allowing a comprehensive review for authorization. |
| Off-Label Use Requirements | If a medication is requested for off-label use, a supportive peer-reviewed journal article must be attached. This requirement helps ensure that off-label prescriptions are clinically justified. |
| Confidentiality Notice | The form includes a confidentiality statement alerting recipients that the content is legally privileged; unauthorized disclosure of the information is prohibited. |
Guidelines on Utilizing Envision Rx Prior Auth
Filling out the Envision Rx Prior Authorization form requires accurate and complete information to ensure a smooth review process. Careful attention to detail will help prevent delays caused by missing or unclear information. Follow these steps to properly complete the form.
- Start with the Patient Information: Enter the patient's name, member number, date of birth, group number, address, city, state, zip code, and member phone number.
- Fill in the Prescriber Information: Include the prescriber's name, fax number, phone number, office contact, NPI (National Provider Identifier), state license ID, address, city, state, and zip code.
- Specify the Drug Name being requested.
- If applicable, indicate if the request is Expedited/Urgent.
- Attach any pertinent medical history or supporting information for the patient.
- Answer Question 1: Select whether this request is for initial or continuing therapy, and include the start date if it is ongoing.
- For Question 2, state the patient's diagnosis related to the requested medication.
- Answer Question 3: Indicate the quantity of medication requested per 30 days.
- Provide information for Question 4: Select the anticipated duration of therapy (less than one month, one to three months, three months to one year, or lifetime).
- List all other medications the patient has previously tried for the indicated diagnosis in Question 5, along with dates and outcomes (e.g., ineffective, adverse reaction).
- If this is an off-label use request, attach a unique peer-reviewed journal article as required and any additional supporting medical information for Question 6.
- Finally, secure the Physician Signature and the date to complete the request.
Once the form is fully filled out, review it for accuracy and completeness before faxing it to the provided number. Proper submission will facilitate a timely review of the authorization request.
What You Should Know About This Form
What is the purpose of the Envision Rx Prior Authorization form?
The Envision Rx Prior Authorization form is necessary for managing certain pharmacy drug benefits. When a physician prescribes a medication that requires prior approval, this form helps facilitate that review process. By gathering relevant patient information and details about the medication request, it allows Envision Rx to make informed decisions about coverage. This ensures that patients receive appropriate medications based on their specific needs.
How should I complete the Envision Rx Prior Authorization form?
Completing the form involves several key steps. Start by filling in the patient's information, such as their name, member number, and date of birth. Next, provide details about the prescribing physician, including their contact information and NPI number. Make sure to indicate whether this request is for initial or continuing therapy and clearly state the patient's diagnosis. Additionally, specify the quantity of medication requested and its anticipated duration. Remember to attach any relevant medical history that could support the request, as this information is crucial for a smooth review process.
What happens if I leave information blank on the form?
If any sections of the form are left blank or the writing is illegible, the review process may be delayed. Incomplete information can hinder Envision Rx from making an accurate assessment of the request. To ensure timely processing, it’s important to double-check that all required fields are filled out clearly and accurately before submitting the form.
What if my request is for off-label use of a medication?
In cases where the medication is being requested for off-label use, additional documentation is required. Specifically, you must provide a unique peer-reviewed journal article that supports the use of the medication in a way that is not approved by the FDA. Alongside this article, it’s beneficial to attach any pertinent medical information that supports the request. Providing strong evidence will greatly assist in the approval process.
How and where should I send the completed form?
Once you have completed the Envision Rx Prior Authorization form, send it via fax to the number listed at the top of the form, which is 877-503-7231. Make sure to keep a copy for your records. If you have any questions during the process, you can call Envision Rx at 866-250-2005 for assistance. Prompt submission of the form is essential to prevent any delays in medication coverage for the patient.
Common mistakes
When filling out the Envision Rx Prior Authorization Request Form, many individuals make simple mistakes that can lead to delays in processing. One common error is leaving information blank. Every section of the form requires attention, including patient details, prescriber information, and medication requests. An empty field can lead to confusion and slow down the approval process. It is crucial to review the form thoroughly before submission to ensure that all necessary information is provided.
Another frequent mistake is providing illegible handwriting. If the form is hard to read, the review team may struggle to process the request. This issue is particularly problematic with critical information such as medical history or dosage requests. To avoid this, consider typing the information or writing clearly in ink. Clarity in communication can significantly improve the chances of a prompt review.
Patients sometimes overlook the significance of listing all prior medications tried. Failing to provide this information can hinder the approval process for a requested medication. The form requires a detailed account of past treatments, including dates and outcomes. By providing complete and accurate information about previous medications, prescribers can better advocate for their patients.
Finally, the requirement for supporting documentation can be easily forgotten. If the request involves off-label use, it is critical to attach a peer-reviewed journal article that justifies the proposed treatment. Neglecting to provide this documentation can result in automatic denials. Ensuring that all supporting materials are included with the submission will help to facilitate a smoother review process.
Documents used along the form
In order to facilitate the prior authorization process with Envision Rx, several additional documents and forms are typically required. Each of these plays a vital role in ensuring that the request is complete and that the necessary information is provided for review. Here’s an overview of commonly used documents in conjunction with the Envision Rx Prior Authorization form.
- Prescription Record: This document provides a history of the patient's prescriptions, detailing medications that have been prescribed, dosages, and any changes made in the therapy over time.
- Medical History Records: A comprehensive summary of a patient's medical background is crucial. This might include previous diagnoses, treatments, hospitalizations, and any other relevant health information.
- Specialist Notes: If a patient has seen a specialist regarding their condition, attaching notes or reports from these visits can bolster the prior authorization request, providing insight into the rationale for prescribing the requested medication.
- Lab Results: Recent lab results that support the medical necessity of the treatment being requested can be essential. These results demonstrate the current state of the patient's health and inform the appropriateness of the medication.
- Peer-Reviewed Journal Article: If the medication is being requested for off-label use, a relevant and credible article from a peer-reviewed journal must be submitted to substantiate its efficacy for the specific diagnosis.
- Patient Consent Form: This form is required to confirm that the patient consents to the release of their medical information to support the prior authorization process.
- Insurance Policy Details: A copy of the patient’s insurance card or details regarding their policy can clarify the patient’s coverage and benefits relating to the requested medication.
- Provider Credentialing Information: This includes information about the prescribing physician's qualifications and credentials, ensuring they are eligible to make the requests for the specific medication.
Having these documents ready and ensuring they are completed accurately can facilitate a smoother and quicker approval process for the medication in question. A well-prepared prior authorization package not only enhances the likelihood of approval but also supports better patient care.
Similar forms
- Medicare Prior Authorization Form: Like the Envision Rx Prior Auth form, this document is used to obtain approval for certain treatments based on a patient's eligibility. Both forms require patient and provider information and detail the medical necessity for the prescribed medication.
- Medicaid Prior Authorization Request: Similar in purpose to the Envision Rx form, the Medicaid version seeks to confirm whether a medication is covered under a state’s Medicaid program. Both require specific patient information, the drug in question, and a rationale for why it’s needed.
- Insurance Prior Authorization Form: This document is used to request pre-approval for certain medications or services from private insurance companies. Both forms collect similar patient and prescriber details, and both require information on prior treatments that failed.
- Clinical Trial Authorization Form: This form requests permission for a patient to access experimental medications or treatments. Like the Envision Rx form, it focuses on the patient’s medical history and condition, but may also require additional details about the clinical trial protocol.
- Appeal for Drug Denial Form: When a medication is not initially approved, this document is used to appeal the decision. Both require detailed patient information and a clear explanation of why the medication is necessary, addressing previous treatments as needed.
- Request for Medical Necessity Form: This document is intended to demonstrate the clinical need for a specific treatment. It parallels the Envision Rx Prior Auth form in outlining the patient’s history, diagnosis, and the justification for the requested therapy.
Dos and Don'ts
When filling out the Envision Rx Prior Authorization form, consider the following do's and don'ts to ensure a smooth process.
- Do provide clear and accurate patient information, including name, date of birth, and member number.
- Do attach relevant medical documentation that supports the request for authorization.
- Do indicate whether the request is for initial or continuing therapy.
- Don't leave any questions blank; missing information can delay the review process.
- Don't submit the form without obtaining a physician's signature and date.
- Don't forget to include peer-reviewed articles if requesting off-label use.
Misconceptions
Misconceptions can often lead to misunderstandings, especially when it comes to crucial forms like the Envision Rx Prior Authorization form. Here are eight common misconceptions, along with clarifications for each.
- All requests for medication are automatically approved. Many people believe that submitting a prior authorization form guarantees medication coverage. In reality, each request undergoes a review process to determine medical necessity.
- Only the prescribing physician needs to fill out the form. This is a common belief. However, the form requires detailed information from both the patient and the prescribing physician to ensure a comprehensive review.
- No supporting documents are necessary. Some assume that a simple request suffices. In truth, attaching relevant medical history or additional supporting documentation can significantly aid in the review process.
- Off-label use does not require additional justification. This is not accurate. If the request is for off-label use, a unique peer-reviewed journal article must be provided to support that request.
- Requests for continuing therapy are less scrutinized. There is a perception that requests for ongoing treatment are treated more leniently. However, these requests still require a thorough review, just like initial therapy requests.
- The form is only relevant for certain medications. Many believe that prior authorization only applies to specialty drugs. In reality, various medications, regardless of classification, may require prior approval.
- Patient information can be left blank if it is not applicable. Some people assume that incomplete forms do not affect the review. This is misleading; any unfilled sections can delay the review process.
- There is no follow-up needed after submitting the form. It is a misconception that after the form is submitted, the process is entirely out of the hands of the patient or physician. Follow-ups are encouraged to track the status of the request and address any potential issues.
By addressing these misconceptions, individuals can navigate the Envision Rx Prior Authorization process more effectively, ensuring timely and appropriate access to necessary medications.
Key takeaways
Completing the Envision Rx Prior Authorization form requires careful attention to detail. Below are key takeaways to help streamline the process:
- Ensure all patient information, including name, member number, and date of birth, is complete and accurate.
- Provide details about the prescriber, including their name, contact information, and NPI number.
- Clearly indicate whether the request is for initial or continuing therapy.
- Include the patient’s diagnosis related to the requested medication.
- State the quantity of medication requested per 30 days and the anticipated duration of therapy.
- List all previous medications attempted by the patient, along with outcomes.
- For off-label use requests, attach a peer-reviewed journal article supporting the request.
- Attach any relevant medical information that may bolster the chances of approval.
- Ensure the form is signed and dated by the prescribing physician before faxing.
Attention to these points can help in avoiding delays in the review process. Always double-check your entries for clarity and legibility.
Browse Other Templates
Export Value Declaration Form - Exporting carriers and ports of export must be identified to facilitate tracking.
Illinois Llc Involuntary Dissolution Reinstatement - Specific instructions regarding where to return the form are included on the document.
Usa Draft - The letter can serve as a reference point for future inquiries about registration.