Fill Out Your Express Scripts Androgel Form
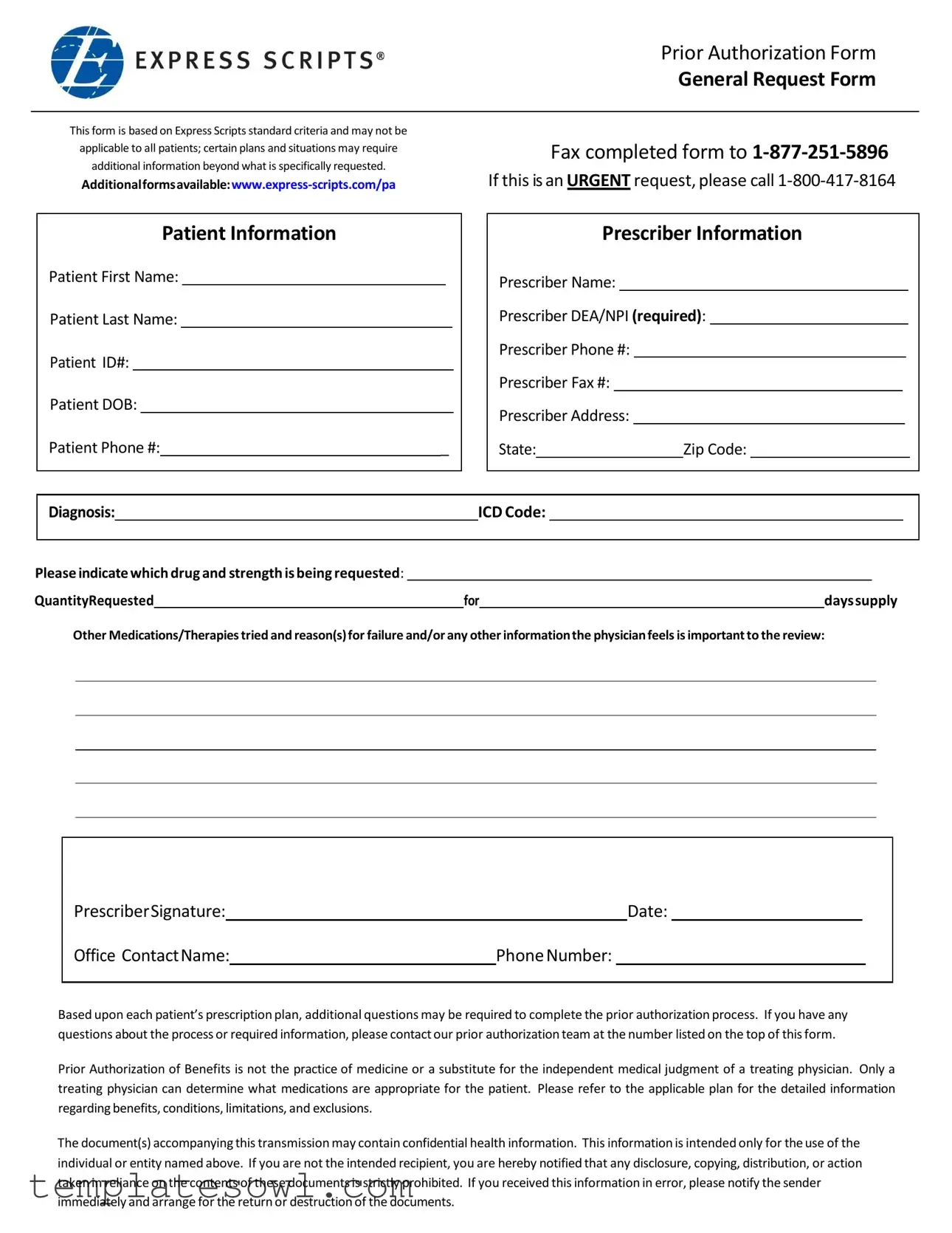
The Express Scripts Androgel prior authorization form serves as an essential tool in the medication approval process for patients requiring testosterone replacement therapy. Designed with standard criteria, this form streamlines the information-gathering process necessary for insurance verification. Each section of the form is carefully structured to ensure that both patient and prescriber details are accurately collected, allowing for a thorough review. Key components include providing patient identification, prescribing details, diagnosis codes, and any previous therapies attempted along with reasons for failure. Patients and prescribers must also indicate the specific drug and dosage being requested, as well as the quantity needed for a given days supply. While the form lays the groundwork for obtaining authorization, it is important to note that further information may be necessary depending on individual insurance plans. As clarification, this process does not replace the medical judgment of a healthcare provider; only a qualified physician can determine the appropriateness of treatment. If there are any questions during the prior authorization process, the support team is readily available to assist. Understanding this form is a vital step in ensuring that patients receive the medications they need without unnecessary delays.
Express Scripts Androgel Example
Prior Authorization Form
General Request Form
This form is based on Express Scripts standard criteria and may not be applicable to all patients; certain plans and situations may require additional information beyond what is specifically requested.
Fax completed form to
If this is an URGENT request, please call
Patient Information
Patient First Name:
Patient Last Name:
Patient ID#:
Patient DOB:
Patient Phone #: |
|
_ |
Prescriber Information
Prescriber Name:
Prescriber DEA/NPI (required):
Prescriber Phone #:
Prescriber Fax #:
Prescriber Address:
State: |
|
Zip Code: |
Diagnosis: |
ICD Code: |
|||
|
|
|
|
|
Please indicate which drug and strength is being requested: |
|
|
QuantityRequested |
for |
dayssupply |
Other Medications/Therapies tried and reason(s) for failure and/or any other information the physician feels is important to the review:
PrescriberSignature: |
|
|
|
Date: |
|
|
||
Office ContactName: |
Phone Number: |
|||||||
|
|
|
|
|
|
|
|
|
Based upon each patient’s prescription plan, additional questions may be required to complete the prior authorization process. If you have any questions about the process or required information, please contact our prior authorization team at the number listed on the top of this form.
Prior Authorization of Benefits is not the practice of medicine or a substitute for the independent medical judgment of a treating physician. Only a treating physician can determine what medications are appropriate for the patient. Please refer to the applicable plan for the detailed information regarding benefits, conditions, limitations, and exclusions.
The document(s) accompanying this transmission may contain confidential health information. This information is intended only for the use of the
individual or entity named above. If you are not the intended recipient, you are hereby notified that any disclosure, copying, distribution,08.22.2011or action taken in reliance on the contents of these documents is strictly prohibited. If you received this information in error, please notify the sender
immediately and arrange for the return or destruction of the documents.
Form Characteristics
| Fact Name | Fact Detail |
|---|---|
| Form Type | This is the Express Scripts Androgel Prior Authorization Form. |
| Submission Method | The completed form should be faxed to 1-877-251-5896. |
| Urgent Requests | If urgent, call 1-800-417-8164 for immediate assistance. |
| Patient Information | Details such as name, ID, DOB, and phone number are required. |
| Prescriber Requirements | Prescriber's DEA/NPI number and contact information must be provided. |
| Diagnosis Information | ICD code and diagnosis details need to be included for processing. |
| Confidentiality Notice | The accompanying information is confidential and meant only for the named recipient. |
Guidelines on Utilizing Express Scripts Androgel
Following the completion of the Express Scripts Androgel form, the information will be submitted to the appropriate authority for review. It is essential to ensure accuracy to avoid any delays in processing. Please follow the steps outlined below to fill out the form correctly.
- Patient Information: Enter the following details:
- Patient First Name
- Patient Last Name
- Patient ID Number
- Patient Date of Birth
- Patient Phone Number
- Prescriber Information: Fill in the relevant details for the prescribing doctor:
- Prescriber Name
- Prescriber DEA/NPI (required)
- Prescriber Phone Number
- Prescriber Fax Number
- Prescriber Address
- State
- Zip Code
- Diagnosis: Clearly state the diagnosis and include the corresponding ICD Code.
- Medication Request: Specify the drug and its strength being requested. Also, indicate the desired quantity along with the days’ supply.
- Other Medications: List any other therapies tried, along with the reason for their failure and any additional relevant information.
- Prescriber Signature: Ensure the prescriber signs and dates the form.
- Office Contact: Provide the name and phone number of an office contact in case further information is needed.
After completing the form, fax it to 1-877-251-5896. For urgent requests, call 1-800-417-8164. If any additional questions or clarifications are required regarding this process, reaching out to the prior authorization team is recommended.
What You Should Know About This Form
What is the purpose of the Express Scripts Androgel Prior Authorization Form?
The Express Scripts Androgel Prior Authorization Form is designed to facilitate the approval process for Androgel prescriptions. Prior authorization helps ensure that patients meet specific criteria set by their insurance plans before they gain access to the medication. This process can help manage costs and promote the use of appropriate treatments based on each patient's individual needs.
What information is required to fill out the form?
The form requests essential details about both the patient and the prescriber. For the patient, you will need their first name, last name, identification number, date of birth, and phone number. The prescriber’s information is also necessary, including their name, DEA or NPI number, phone number, fax number, and address. Additionally, you must provide the patient's diagnosis, ICD code, and details about the specific drug being requested, including dosage and quantity. Any past medications or therapies attempted and reasons for their failure should also be included for the review process.
How do I submit the completed form?
You can submit the completed Prior Authorization Form via fax to the designated number, which is 1-877-251-5896. If you have an urgent request, it is advisable to call the dedicated line at 1-800-417-8164 for immediate assistance. Ensuring that all required fields are completed accurately will help expedite the review process.
What happens after the form is submitted?
Once the form is submitted, the prior authorization team will review the information provided. They may reach out for additional details if needed based on the specific requirements of the patient's insurance plan. After the review, you will receive a determination regarding the authorization of Androgel. This process is separate from the actual prescribing and treatment decisions made by a healthcare provider.
Is there any other information I should be aware of?
Common mistakes
Submitting the Express Scripts Androgel form can seem straightforward, yet many individuals encounter pitfalls that delay the approval process. One common mistake is failing to provide complete patient information. It is essential to include the patient's first name, last name, ID number, date of birth, and contact number. Omitting even one detail may lead to unnecessary delays in processing the request.
Another frequent error involves neglecting to fill out the prescriber information completely. The prescriber’s name, DEA or NPI number, and contact details must be accurate and clear. If these pieces of information are missing or incorrect, it may hinder the ability of the pharmacy to contact the prescriber, further complicating the authorization process.
Providing an unclear diagnosis or forgetting to include the ICD code is also an issue. The diagnosis is critical, as it informs the decision-making process for approval. If the ICD code is not specified or is incorrectly listed, it could result in a denial of the authorization request. Always double-check that this section is filled in accurately.
Another mistake often observed is improperly indicating which drug and strength is being requested. It might seem trivial, but clarity in this section is paramount. Clarity helps eliminate confusion for those reviewing the form, speeding up the review process during authorization.
Sometimes, individuals fail to specify the quantity requested and the days supply. This oversight can result in questions from the pharmacy about the appropriateness of the dosage requested. Avoid ambiguity by ensuring that the quantity and duration are clearly listed.
Neglecting to mention other medications or therapies that have been tried, along with the reasons for their failure, is yet another mistake. This information is crucial for demonstrating to the reviewer why the requested medication is necessary. Be thorough in detailing this section to illustrate the patient’s treatment history.
Many also forget to include the prescriber’s signature and date. An incomplete signature can threaten the validity of the request, leading to processing delays. Always confirm that both the signature and date are provided before submission.
Finally, failing to contact the prior authorization team for clarification if unsure about any part of the process can lead to frustration. Reaching out for guidance can help ensure that the form is completed correctly and expedites the approval process. Taking these steps might prevent complications and ensure efficient handling of the request.
Documents used along the form
The Express Scripts Androgel form is part of an essential process for patients needing specific medications. Alongside this form, several other documents often come into play, contributing to the overall authorization and treatment process. Below, you'll find an overview of these related forms.
- Prior Authorization Request Form: This form provides details required for a request to determine whether a medication will be covered by insurance. It generally requires patient information, medical history, and information on the prescribed treatment. It ensures that healthcare providers can supply the right treatment while adhering to insurance policies.
- General Request Form: Used to address various requests to the insurance provider outside standard prescriptions. This form covers information that may include inquiries about coverage, benefits, and eligibility for different medications and services.
- Medication History Form: This document helps healthcare providers collect past prescription information about a patient. It includes any drugs or therapies previously taken, the reason for their discontinuation, and how they interacted with the patient. It can aid in determining the best course of treatment moving forward.
- Prescriber’s Notes or Recommendations: Often included alongside the primary forms, these notes provide personalized insights from the prescribing physician. They may elaborate on why a specific treatment is necessary, offer explanations about medication choices, and detail any unique patient circumstances that warrant special consideration.
Understanding these documents can help patients navigate the often complex healthcare landscape. They are designed to ensure that necessary treatments are approved and provided in a manner that is both efficient and compliant with insurance regulations. Each form plays a critical role in securing access to essential medications like Androgel.
Similar forms
The Express Scripts Androgel form is very similar to several other documents used in the healthcare system. Here's a quick overview of seven other documents you might encounter in similar situations:
- Prior Authorization Request Form: Just like the Androgel form, this document collects patient and prescriber information. It’s used to determine if a particular medication is covered under a patient’s insurance plan.
- Medication Request Form: This form is for requesting approval for specific medications. It includes details about the patient, the requested medication, and any previous therapies tried, resembling the structure of the Androgel form.
- Insurance Claim Form: Similar in its need for detailed patient and provider information, this form submits a request for payment or coverage for medical services provided to the patient.
- Time Sensitive Request Form: Just like the urgent request section on the Androgel form, this document is used when immediate action is needed. It requires thorough patient information and a clear explanation of urgency.
- Follow-Up Request Form: This form is an extension of the initial request. It also gathers patient data but focuses on additional information since the first submission may not have sufficed.
- Clinical Summary Form: Healthcare providers fill this out to summarize a patient’s medical history, current medications, and treatment plan, paralleling the information required in the Androgel form.
- Patient Consent Form: This document, while primarily focused on obtaining permission for treatment, also necessitates patient and prescriber details, aligning with the data collection purpose of the Androgel form.
Understanding these similarities can help in navigating healthcare processes more effectively. Each document plays a crucial role in ensuring appropriate medication management and patient care.
Dos and Don'ts
When filling out the Express Scripts Androgel form, it is important to adhere to certain practices. Below are guidelines to follow and avoid.
- Do: Read the form carefully before starting.
- Do: Ensure all patient information is accurate and complete.
- Do: Provide the prescriber’s DEA/NPI number as it is required.
- Do: Indicate the exact drug and dosage being requested.
- Do: Fax the completed form to the correct number, 1-877-251-5896.
- Don't: Leave any sections blank; fill in all necessary details.
- Don't: Use outdated or incorrect patient information.
- Don't: Ignore the request for additional information if prompted by the plan.
- Don't: Assume prior authorization equates to medical advice.
Misconceptions
When it comes to the Express Scripts Androgel form, misconceptions can lead to confusion and unnecessary delays in treatment. Here are six common misconceptions:
- Myth 1: The form is the same for all patients.
- Myth 2: Submitting the form guarantees approval.
- Myth 3: All medications require prior authorization.
- Myth 4: There’s no need for additional information.
- Myth 5: The prescriber signature is optional.
- Myth 6: Prior authorization is the same as medical advice.
Reality: The Express Scripts Androgel form is based on standard criteria but may not apply to every patient. Certain plans or situations may require additional information beyond what is specifically requested.
Reality: Just because the form is submitted does not guarantee that the medication will be approved. The approval process depends on the specifics of each patient's situation and the requirements of their insurance plan.
Reality: While many medications may require prior authorization, not every medication does. The requirement varies with different insurance plans and specific medications.
Reality: Depending on the patient’s prescription plan, additional questions may need to be answered to complete the prior authorization process. Providing comprehensive information is crucial.
Reality: A prescriber signature is required for the form to be valid. Without it, the prior authorization request cannot be processed.
Reality: Prior authorization is not a substitute for the independent medical judgment of a treating physician. Only a medical professional can determine what medications are appropriate for a patient.
Understanding these misconceptions can help ensure a smoother process when obtaining Androgel through Express Scripts. For specific questions about your situation, contacting the prior authorization team can be beneficial.
Key takeaways
When filling out and using the Express Scripts Androgel form, keep these key takeaways in mind:
- Complete Patient Information: Ensure all patient details, including first name, last name, ID number, date of birth, and phone number, are accurately filled out.
- Prescriber Details are Crucial: Include the prescriber’s name, DEA/NPI number, phone, fax, and address, as this information is mandatory.
- Clear Diagnosis and Treatment History: Provide a specific diagnosis with the ICD code, and detail any other medications or therapies attempted, along with reasons for failure.
- Urgent Requests: If the request is urgent, do not hesitate to call the dedicated number for immediate assistance.
- Confidentiality Matters: Handle the form carefully, as it contains sensitive health information meant only for the intended recipient.
Taking these steps will help streamline the process and ensure that all necessary information is provided for a timely review.
Browse Other Templates
Renew Cna License Texas - Understanding the submission guidelines is critical for facilities with multiple nurse aides.
Alabama Form A-1 - Form 96 is applicable for the calendar year end reporting.