Fill Out Your Express Scripts Fax Form
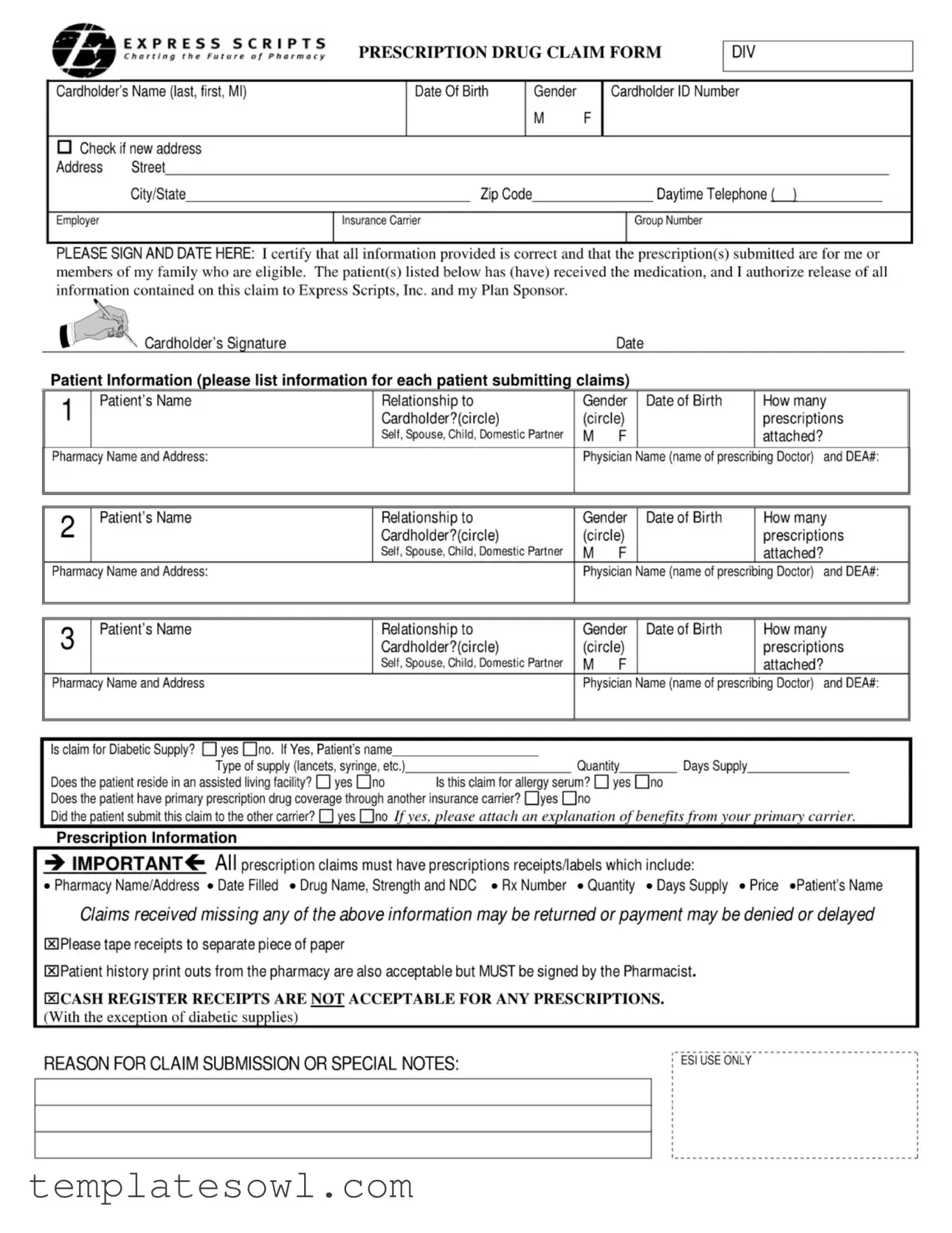
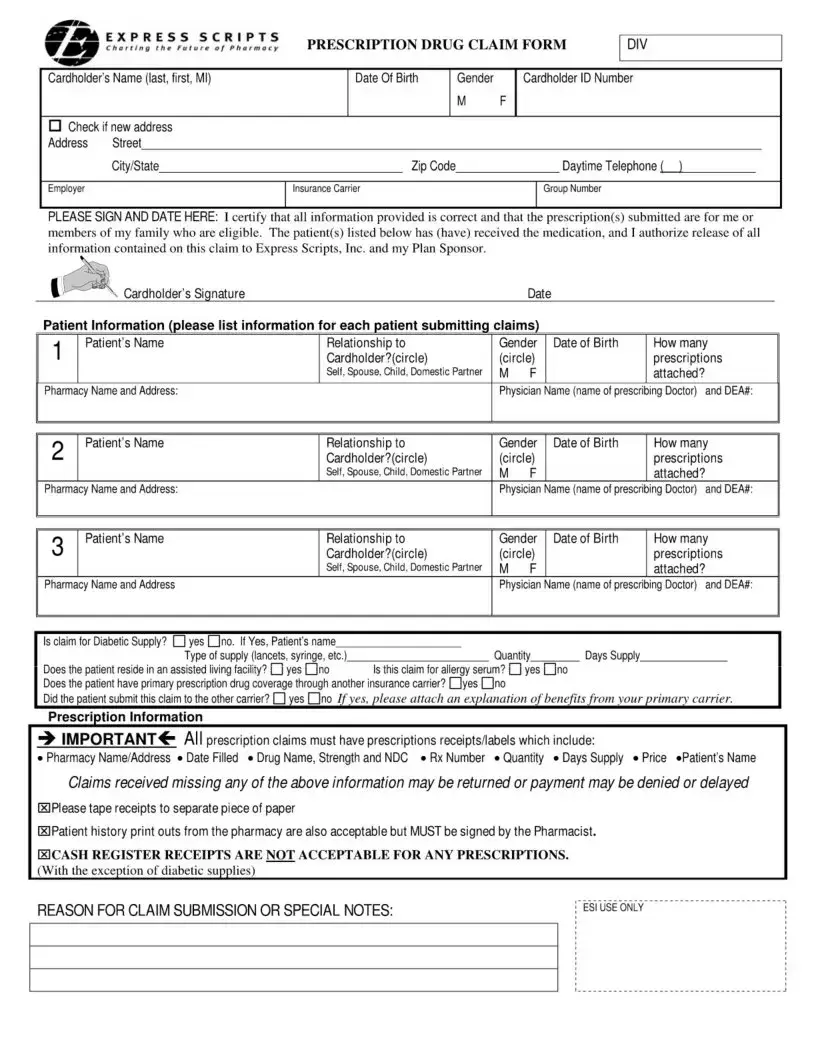
The Express Scripts Fax form serves as a vital tool for cardholders seeking to submit prescription drug claims efficiently. Essential information gathering begins with the cardholder's name, contact details, and insurance specifics, ensuring accurate processing of the claim. Each section requires basic identifiers, including the cardholder's ID number and date of birth, alongside their relationship to the patients for whom prescriptions are being claimed. Furthermore, the form includes spaces for listing the medications and the prescribing physician’s information, crucial elements for successful claim submission. Instructions clearly state that all necessary documentation, such as receipts and labels, must accompany the form to prevent delays or denials. Additionally, designated areas allow for the identification of claims pertaining to diabetic supplies or allergy serums. The form emphasizes the requirement for signatures, highlighting the importance of complete information to adhere to processing standards. By following the outlined steps and providing accurate details, cardholders can streamline their claims submissions with Express Scripts.
Express Scripts Fax Example
сЛГЛ E ?Л.?« СДІЛЛ S |
PRESCRIPTION DRUG CLAIM FORM |
||
Cardholder’s Name (last, first, Ml) |
Date Of Birth |
Gender |
Cardholder ID Number |
|
|
M |
F |
Check if new address |
|
|
|
Address Street |
|
|
|
Citv/State |
Zip Code |
|
Davtime Telephone ( ) |
Employer |
Insurance Carrier |
|
Group Number |
PLEASE SIGN AND DATE HERE: I certify that all information provided is correct and that the prescription(s) submitted are for me or members of my family who are eligible. The patient(s) listed below has (have) received the medication, and I authorize release of all information contained on this claim to Express Scripts, Inc. and my Plan Sponsor.
Cardholder’s Signature |
Date |
Patient Information (please list information For each patient submitting claims)
1 |
Patient’s Name |
Relationship to |
Gender Date of Birth |
How many |
|
|
Cardholder?(circle) |
(circle) |
prescriptions |
||
|
|
Self, Spouse, Child, Domestic Partner |
M |
F |
attached? |
Pharmacy Name and Address: |
|
Physician Name (name of prescribing Doctor) and DEA#: |
|||
2 |
Patient’s Name |
Relationship to |
|
Cardholder?(circle) |
|
|
|
Self, Spouse, Child, Domestic Partner |
Pharmacy Name and Address: |
|
|
3 |
Patient's Name |
Relationship to |
|
Cardholder?(circle) |
|
Self, Spouse, Child, Domestic Partner
Pharmacy Name and Address
Gender Date of Birth |
How many |
|
(circle) |
prescriptions |
|
M |
F |
attached? |
Physician Name (name of prescribing Doctor) and DEA#:
Gender Date of Birth |
How many |
|
(circle) |
prescriptions |
|
M |
F |
attached? |
Physician Name (name of prescribing Doctor) and DEA#:
Is claim for Diabetic Supply? □yesdno. If Yes, Patient's name |
|
|
|
|
Type of supply (lancets, syringe, etc.) |
Quantity |
Days Supply |
||
Does the patient reside in an assisted living facility? |
yes EJno |
Is this claim for allergy serum? |
yes dno |
|
Does the patient have primary prescription drug coverage through another insurance carrier? dyes dno
Prescription Information
■» IMPORTANT^- All prescription claims must have prescriptions receipts/labels which include:
• Pharmacy Name/Address • Date Filled • Drug Name, Strength and NDC • Rx Number • Quantity • Days Supply • Price «Patient’s Name
Claims received missing any of the above information may be returned or payment may be denied or delayed
ИPlease tape receipts to separate piece of paper
(3 Patient history print outs from the pharmacy are also acceptable but MUST be signed by the Pharmacist.
ECASH REGISTER RECEIPTS ARE NOT ACCEPTABLE FOR ANY PRESCRIPTIONS.
(With the exception of diabetic supplies)
REASON FOR CLAIM SUBMISSION OR SPECIAL NOTES: |
L esi Use only |
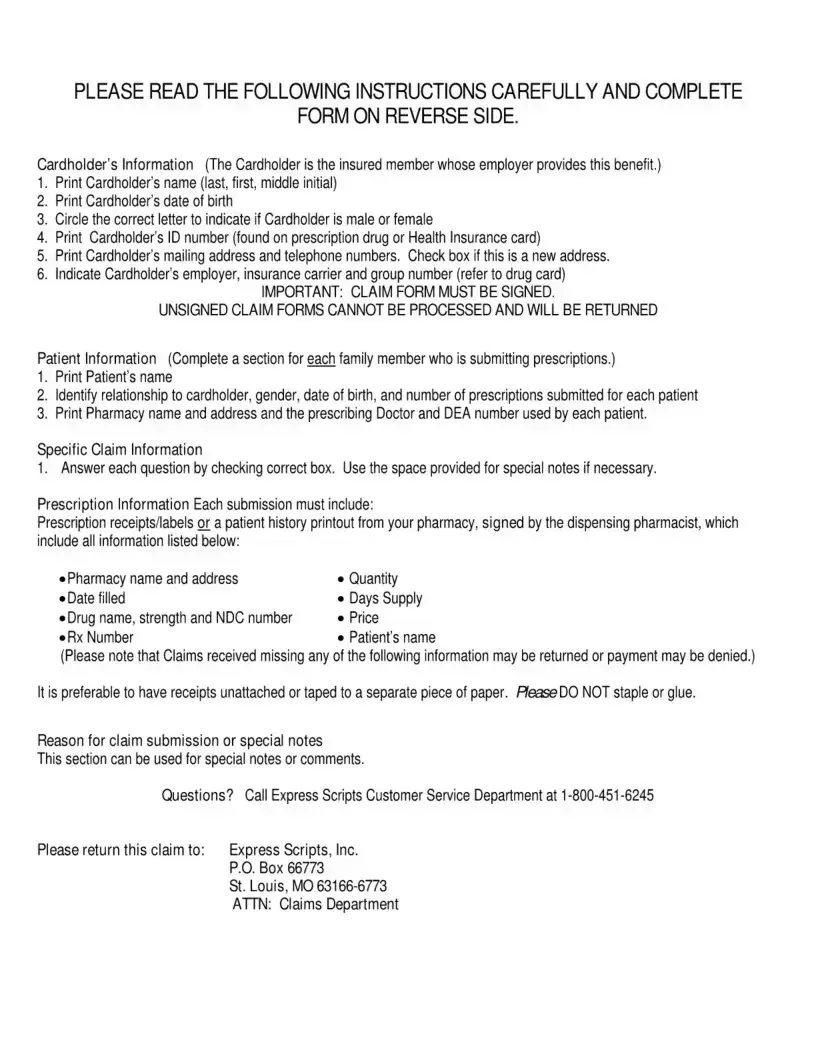
PLEASE READ THE FOLLOWING INSTRUCTIONS CAREFULLY AND COMPLETE
FORM ON REVERSE SIDE.
Cardholder’s Information (The Cardholder is the insured member whose employer provides this benefit.)
1.Print Cardholder's name (last, first, middle initial)
2.Print Cardholder’s date of birth
3.Circle the correct letter to indicate if Cardholder is male or female
4.Print Cardholder’s ID number (found on prescription drug or Health Insurance card)
5.Print Cardholder’s mailing address and telephone numbers. Check box if this is a new address.
6.Indicate Cardholder's employer, insurance carrier and group number (refer to drug card)
IMPORTANT: CLAIM FORM MUST BE SIGNED.
UNSIGNED CLAIM FORMS CANNOT BE PROCESSED AND WILL BE RETURNED
Patient Information (Complete a section for each family member who is submitting prescriptions.)
1.Print Patient’s name
2.Identify relationship to cardholder, gender, date of birth, and number of prescriptions submitted for each patient
3.Print Pharmacy name and address and the prescribing Doctor and DEA number used by each patient.
Specific Claim Information
1.Answer each question by checking correct box. Use the space provided for special notes if necessary.
Prescription Information Each submission must include:
Prescription receipts/labels or a patient history printout from your pharmacy, signed by the dispensing pharmacist, which include all information listed below:
• Pharmacy name and address |
• Quantity |
• Date filled |
«Days Supply |
• Drug name, strength and NDC number |
• Price |
• Rx Number |
• Patient's name |
(Please note that Claims received missing any of the following information may be returned or payment may be denied.)
It is preferable to have receipts unattached or taped to a separate piece of paper. HeaseDO NOT staple or glue.
Reason for claim submission or special notes
This section can be used for special notes or comments.
Questions? Call Express Scripts Customer Service Department at 1
Please return this claim to: |
Express Scripts, Inc. |
|
P.O. Box 66773 |
|
St. Louis, MO |
|
ATTN: Claims Department |
Form Characteristics
| Fact Name | Description |
|---|---|
| Cardholder Information Required | Cardholders must provide their full name, date of birth, gender, ID number, and contact information, including a mailing address. |
| Patient Information Section | A separate section is needed for each patient, detailing their relationship to the cardholder, gender, date of birth, and the number of prescriptions submitted. |
| Prescription Receipts | Evidence of prescriptions must be included. Receipts need to list the pharmacy name, drug details, price, and more to avoid claim rejections. |
| Signature Requirement | The claim form must be signed by the cardholder. Unsigned forms will be returned, causing delays in processing. |
| Diabetic and Allergy Claims | Specific questions regarding diabetic supplies and allergy serum must be answered to process those types of claims. |
| Address Change Notification | If the cardholder has a new address, they should check the box provided on the form to ensure timely communication. |
| Contact for Assistance | If there are questions about the claim process, cardholders can reach out to Express Scripts customer service at 1-800-451-6245. |
| Submission Address | Completed forms should be returned to Express Scripts, Inc., at the specified P.O. box in St. Louis, MO to ensure proper processing. |
Guidelines on Utilizing Express Scripts Fax
Completing the Express Scripts Fax form accurately is essential for the timely processing of prescription claims. Follow these structured steps to ensure that all necessary information is submitted correctly. Your attention to detail will help avoid delays in processing your claims.
- Print the cardholder's name clearly (last, first, middle initial) in the designated box.
- Input the cardholder’s date of birth.
- Circle the appropriate letter to indicate the cardholder’s gender: male (M) or female (F).
- Enter the cardholder’s ID number found on the prescription or health insurance card.
- Fill in the cardholder’s mailing address, including street, city, state, and zip code. If this is a new address, check the box provided.
- Indicate the cardholder's employer, insurance carrier, and group number as indicated on the drug card.
- Sign and date the form to certify that the information provided is correct.
For each patient submitting claims, fill out the following:
- Print each patient’s name in the designated section.
- Specify the relationship of each patient to the cardholder by circling the appropriate option (Self, Spouse, Child, Domestic Partner).
- Circle the gender of the patient (M or F).
- Input the patient’s date of birth.
- Indicate the number of prescriptions attached for this patient.
- Provide the pharmacy name and address used by the patient.
- List the prescribing physician’s name and DEA number for each patient.
Next, address any specific claim information:
- Answer the questions regarding diabetic supplies, allergy serum claims, and primary drug coverage by checking the correct box.
- Attach precise prescription information, ensuring it includes pharmacy details, drug name, quantity, days' supply, and price. Ensure that all receipts are unattached and do not staple or glue.
- Use the "Reason for Claim Submission or Special Notes" section for any additional comments necessary for processing the claim.
Once the form is complete, return it to Express Scripts, Inc. at the specified address. For assistance, contact the Express Scripts Customer Service Department at 1-800-451-6245.
What You Should Know About This Form
What is the Express Scripts Fax Form?
The Express Scripts Fax Form is a document used to submit prescription drug claims for reimbursement. It allows cardholders to provide necessary information about themselves and their dependents who received medications and ensures that all pertinent details are included for a smooth claims processing experience.
Who should fill out the Express Scripts Fax Form?
The form should be filled out by the individual who holds the prescription drug insurance card, known as the cardholder. This can be the insured individual or a family member submitting claims on their behalf. Each family member who has received prescriptions must be listed on the form, providing relevant details for each patient.
What information is required on the form?
Key information includes the cardholder’s full name, address, date of birth, gender, ID number, and details on any prescriptions. Each patient’s name, relationship to the cardholder, gender, date of birth, and number of prescriptions must also be included. Additionally, pharmacy and prescribing doctor details are necessary, along with any special considerations such as diabetic supplies or whether the patient resides in an assisted living facility.
What documentation do I need to submit with the form?
You must attach the prescription receipts or labels that include specific information like the pharmacy name and address, drug name, strength, quantity, days of supply, NDC number, and the RX number. Patient history printouts signed by the pharmacist are also acceptable. Ensure no staples or glue are used on attachments, and do not include cash register receipts.
How do I submit the completed form?
Once you have completed the form and attached the necessary documentation, send it via fax or mail to Express Scripts, Inc. at the address provided on the form. Ensure that your claim is sent to the Claims Department for processing. For urgent matters, using fax can expedite the submission process.
What happens if I forget to sign the form?
Failure to sign the form will result in your claim being returned and delayed. It is crucial to provide a signature as confirmation that all the information you have submitted is accurate and that the prescriptions are for you or eligible family members.
Are there any exclusions or special considerations I need to be aware of?
Yes, claims may be denied or delayed if the required information is missing. Additionally, claims pertaining to supplies, allergy serums, or those under another primary insurance must be clearly indicated on the form. Be sure to provide any extra notes for special cases in the designated section.
How can I contact Express Scripts if I have questions?
If you need assistance completing the form or have specific questions regarding your claim, contact Express Scripts Customer Service Department at 1-800-451-6245. They can provide guidance to ensure your form is filled out correctly.
What if I have more than three patients to report?
The form has spaces to enter information for three patients. If you need to report claims for more individuals, you can either add additional forms or provide the required information in a separate document. Just ensure that all supporting information is submitted to avoid processing delays.
Common mistakes
When filling out the Express Scripts Fax form, individuals often encounter common pitfalls that can delay or complicate the processing of their prescription claims. Understanding these mistakes can make a significant difference in ensuring a smooth submission process.
One prevalent error is the failure to provide complete personal information. It is essential to fill in all required fields accurately, including the cardholder's name, date of birth, and address. Skipping even a single piece of information can lead to rejected claims, creating unnecessary delays. The importance of double-checking this section cannot be overstated.
Another mistake is neglecting to sign the claim form. An unsigned claim can simply be returned, frustratingly delaying the process. Taking a moment to ensure that you, or the cardholder, have signed and dated the form before submission is crucial. This step confirms the authenticity of the information provided.
Inaccuracies in patient information are also common. Each patient's details—such as their name, date of birth, and relationship to the cardholder—must be entered correctly. Missing or incorrect details about the prescriptions attached can result in a claim being returned, which delays the approval of necessary medications.
Moreover, many people fail to attach the necessary prescription receipts or labels. Clear instructions specify that claims must include vital details like the pharmacy's name and address, the drug's name and strength, and the prescription number. Omitting any of this information can trigger delays or denials. It's advisable to check the requirements thoroughly before submission.
Additionally, some may not utilize the special notes section effectively. This area can clarify details about the claim, particularly regarding unique circumstances. For instance, if a claim is for diabetic supply items, indicating the type of supply and relevant quantities can aid in swift processing.
Finally, failure to consider insurance specifics can lead to complications. If a patient holds primary drug coverage through another insurance carrier, that information must be disclosed. Not doing this may result in complications or denials of claims, revealing the importance of providing complete context surrounding the insurance coverage.
By recognizing these common errors and addressing them before submission, individuals can improve the likelihood of their pharmacy claims being processed swiftly and efficiently.
Documents used along the form
The Express Scripts Fax form is a crucial document for submitting prescription drug claims. Along with this form, several other documents may often be required or helpful in the claims process. Below is a list of those documents, each serving a unique purpose to ensure smooth processing and approval of claims.
- Prescription Label Receipts: These receipts must include key details such as the pharmacy name, date filled, drug name, strength, and quantity. They are essential for verifying the prescription information.
- Patient History Printouts: This document provides a record of the medications dispensed to the patient at the pharmacy. It must be signed by the pharmacist to validate the information provided.
- Provider's DEA Certificate: If the claim involves controlled substances, the prescribing physician's Drug Enforcement Administration (DEA) number must be submitted. This certifies that the doctor is authorized to prescribe such medications.
- Insurance Information Form: This form outlines the patient’s primary insurance details, including any group numbers or policy numbers, which aids in coordinating benefits among multiple insurance plans.
- Authorization to Release Information Form: This document grants permission for sensitive medical information to be shared with relevant parties, ensuring compliance with privacy regulations.
- Claim Reimbursement Request Form: Sometimes a specific reimbursement request is needed. This form provides details about the expenses incurred and justifies why a reimbursement is being claimed.
- Diabetes Supply Order Form: If a claim involves diabetic supplies, this specialized form outlines the quantities and types of supplies required, ensuring all necessary documentation is submitted for those specific items.
Each of these documents facilitates the claims process and helps ensure that all necessary information is available for review. By preparing and submitting the required forms together, claimants can significantly improve their chances of a prompt resolution.
Similar forms
- Health Insurance Claim Form: Similar in purpose, this document is used to submit claims for reimbursements of healthcare services provided by hospitals or healthcare providers. It gathers patient and provider information as well as details regarding treatment received.
- Medicare Prescription Drug Form: This document is intended for Medicare beneficiaries who want to claim prescription drug benefits. Like the Express Scripts form, it requires patient identification, prescription details, and verification of eligibility.
- Dental Claim Form: Used to claim reimbursements for dental services, this form collects patient information, the dentist's information, and specific details about the services rendered, akin to the prescription information section of the Express Scripts form.
- Workers' Compensation Claim Form: This form is utilized when claiming benefits for work-related injuries. It requires details about the injury, treatment received, and patient information, paralleling the structured information gathering from the Express Scripts Fax form.
- Pharmacy Prior Authorization Request: Required for certain medications, this document facilitates the approval process before treatment. Like the Express Scripts form, it includes patient and provider details, ensuring that all necessary information is thoroughly conveyed.
- Flexible Spending Account (FSA) Reimbursement Form: Patients submit this form to receive reimbursements for eligible healthcare expenses. This form also gathers both patient and treatment information, much like the Express Scripts form.
- Durable Medical Equipment (DME) Claim Form: Used when patients claim medical supplies like wheelchairs or pain management devices, similar patient and provider data is documented, focusing on the usage context and amount requested, similar to prescription claims.
- Vision Claim Form: Patients complete this for reimbursements for vision-related services. It typically requires patient demographic information and service details, closely mirroring the information structure found in the Express Scripts form.
- Out-of-Network Claim Form: For services rendered by providers not covered under a patient’s insurance plan, this form collects comprehensive details about the treatment and provider, resembling the thorough documentation needed for prescription claims.
- Medication Therapy Management (MTM) Documentation: This form is used in various medication review programs and requires patient consent and treatment history, similar to the structured patient information necessary on the Express Scripts Fax form.
Dos and Don'ts
When filling out the Express Scripts Fax form, attention to detail is essential. Adhering to guidelines can streamline the processing of your claim. Here are key things to do and avoid:
- Do: Ensure all patient information is complete and accurate for each member submitting claims.
- Do: Include prescription receipts or pharmacy history printouts signed by the pharmacist, as this documentation is critical.
- Do: Review the completed form for signatures to avoid delays; unsigned forms will be returned.
- Do: Check that all information adheres to the requirements listed, such as pharmacy details and drug specifics.
- Don't: Staple or glue receipts; they should be unattached or taped to a separate page.
- Don't: Forget to indicate if the claim is for diabetic supplies or allergy serum, as this information is necessary.
- Don't: Submit claims missing any required information, such as patient details or prescription specifics, as this could lead to denial.
- Don't: Use cash register receipts; these are not acceptable for prescription claims.
Misconceptions
Misconceptions about the Express Scripts Fax Form often arise due to a lack of clarity regarding its requirements and procedures. Here are six common misunderstandings:
- Misconception 1: The form can be submitted without a signature.
- Misconception 2: Any record of a prescription will suffice.
- Misconception 3: Only new prescriptions require this form.
- Misconception 4: The form is only for one family member.
- Misconception 5: All insurance queries are resolved with the submission.
- Misconception 6: Attachments can be stapled to the form.
Many people believe that they can send the form without signing it. However, an unsigned claim form cannot be processed and will be returned. It is crucial to check that the form is signed before submission.
Some individuals think that just any receipt will do for their claims. In reality, each submission must include specific details like the pharmacy name, drug name, and other vital information. Failing to provide these details may result in delayed or denied claims.
It is a common belief that this form is only for new prescriptions. In fact, it can be used for various types of claims, including refills, as long as the necessary documentation is provided.
Some may think that the fax form can only accommodate claims for a single individual. However, the form allows for multiple patients to be included, making it easier for families to submit their claims in one go.
Individuals sometimes assume that submitting the form will address all questions related to their insurance coverage. While the form helps process claims, any issues regarding insurance eligibility or other queries must be addressed directly with the insurance provider.
A frequent error is the belief that attaching documents via staples is acceptable. It is critical to remember that receipts should remain unattached or taped to a separate piece of paper, as stapling can hinder processing.
Key takeaways
When filling out the Express Scripts Fax form, it’s essential to be thorough and accurate. Here are key takeaways to consider:
- Complete Information: Fill out all required fields for the cardholder and each patient with precise details.
- Signature Required: Ensure you sign and date the form; unsigned forms will be returned.
- Dependent Claims: Specify the relationship of each patient to the cardholder to confirm eligibility.
- Prescription Receipts: Include all necessary pharmacy receipts or labels. They must contain required details like drug name, quantity, and price.
- No Staples: Attach receipts without staples. Tape them to a separate sheet of paper for submission.
- Special Notes: Utilize the special notes section for any additional comments or clarification regarding the claim.
- Check Insurance: Confirm if the patient has existing coverage with another insurance carrier, which can affect the claim.
- Avoid Common Mistakes: Ensure all prescriptions are attached and that all required information is included to prevent delays.
- Contact Information: If questions arise, reach out to Express Scripts Customer Service at 1-800-451-6245 for assistance.
Following these guidelines will simplify the process and help ensure timely processing of your claims.
Browse Other Templates
Choices Opwdd - Evaluating provided information before submission is crucial to ensure compliance.
Health Insurance Payment - The DHCS 9061 helps clarify eligibility requirements for receiving reimbursement under HIPP.