Fill Out Your Express Scripts Prior Authorization Form
The Express Scripts Prior Authorization form is a critical tool for plan members prescribed medications that require approval before the insurance provider covers costs. Initiating this process requires some essential steps. First, the plan member must complete Part A, providing personal and insurance details, along with any relevant information regarding other coverage or patient assistance programs. The prescribing doctor then fills out Part B, which collects rigorous medical information, including the patient's condition, previous therapies, and the specifics of the requested medication. Once both parts are filled out, the completed form can be faxed or mailed to Express Scripts Canada. It's important to note that submitting this form does not guarantee approval, as a review process based on established clinical criteria determines the outcome. Plan members will receive notification regarding the decision, and they retain the option to appeal if denied. This procedural transparency is essential for effective patient advocacy within the healthcare system.
Express Scripts Prior Authorization Example
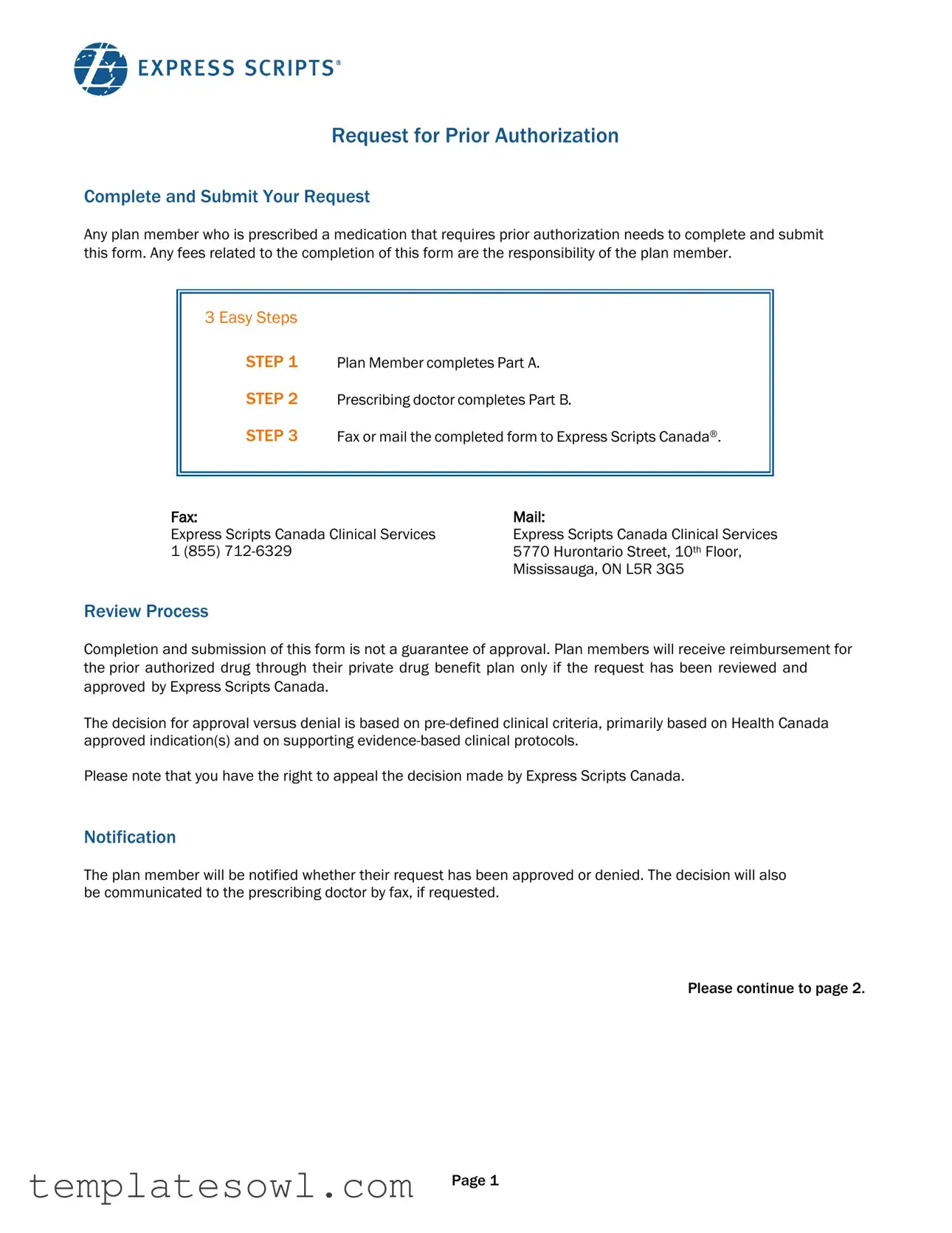
Request for Prior Authorization
Complete and Submit Your Request
Any plan member who is prescribed a medication that requires prior authorization needs to complete and submit this form. Any fees related to the completion of this form are the responsibility of the plan member.
3 Easy Steps
STEP 1 |
Plan Member completes Part A. |
STEP 2 |
Prescribing doctor completes Part B. |
STEP 3 |
Fax or mail the completed form to Express Scripts Canada®. |
Fax: |
Mail: |
Express Scripts Canada Clinical Services |
Express Scripts Canada Clinical Services |
1 (855) |
5770 Hurontario Street, 10th Floor, |
|
Mississauga, ON L5R 3G5 |
Review Process
Completion and submission of this form is not a guarantee of approval. Plan members will receive reimbursement for the prior authorized drug through their private drug benefit plan only if the request has been reviewed and approved by Express Scripts Canada.
The decision for approval versus denial is based on
Please note that you have the right to appeal the decision made by Express Scripts Canada.
Notification
The plan member will be notified whether their request has been approved or denied. The decision will also be communicated to the prescribing doctor by fax, if requested.
Please continue to page 2.
Page 1
Request for Prior Authorization
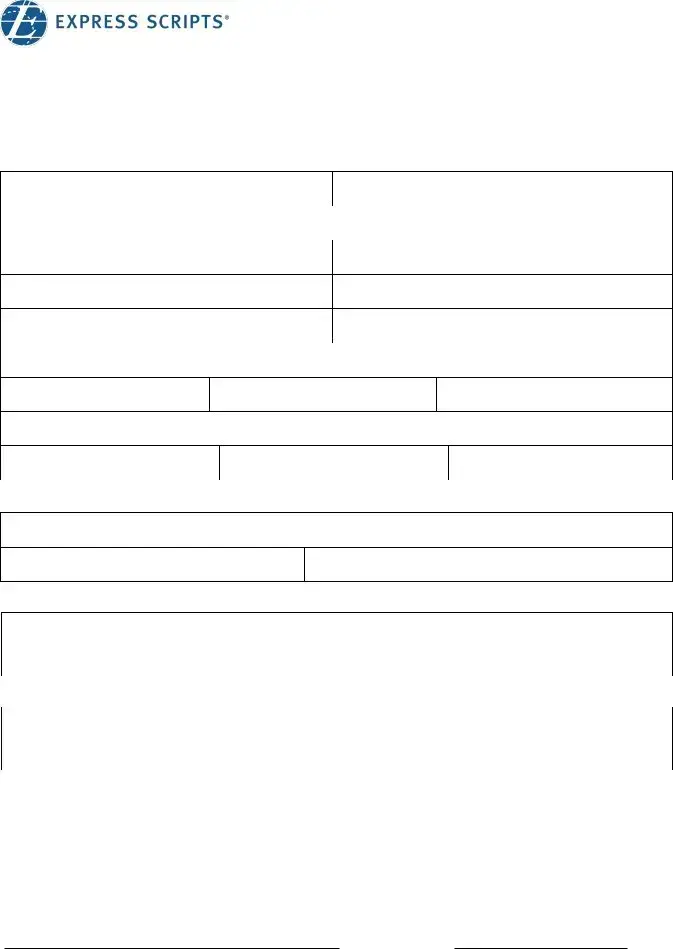
Part A – Patient
Please complete this section and then take the form to your doctor for completion.
Patient information |
|
|
|
|
|
|
First Name: |
|
|
|
Last Name: |
|
|
Insurance Carrier Name/Number: |
|
|
|
|
|
|
Group number: |
|
|
|
Client ID: |
|
|
Date of Birth (DD/MM/YYYY): |
/ |
/ |
Relationship: |
□ Employee |
□ Spouse □ Dependent |
|
Language: |
□ English |
□ |
French |
Gender: |
□ Male |
□ Female |
Address: |
|
|
City: |
Province: |
Postal Code: |
Email address: |
|
|
Telephone (home): |
Telephone (cell): |
Telephone (work): |
Patient Assistance Program |
|
|
Is the patient enrolled in any patient support program? ❒ Yes |
❒ No |
|
Contact name: |
Telephone: |
|
Provincial Coverage |
|
|
Has the patient applied for reimbursement under a provincial plan? ❒ Yes ❒ No
What is the coverage decision of the drug? ❒ Approved ❒ Denied **Attach provincial decision letter**
Primary Coverage
If patient has coverage with a primary plan, has a reimbursement request been submitted? ❒ Yes ❒ No ❒ N/A What is the coverage decision of the drug? ❒ Approved ❒ Denied **Attach decision letter **
Authorization
On behalf of myself and my eligible dependents, I authorize my group benefit provider, and its agents, to exchange the personal information contained on this form. I give my consent on the understanding that the information will be used solely for purposes of administration and management of my group benefit plan. This consent shall continue so long as my dependents and I are covered by, or are claiming benefits under the present group contract, or any modification, renewal, or reinstatement thereof.
Plan Member Signature |
Date |
Page 2
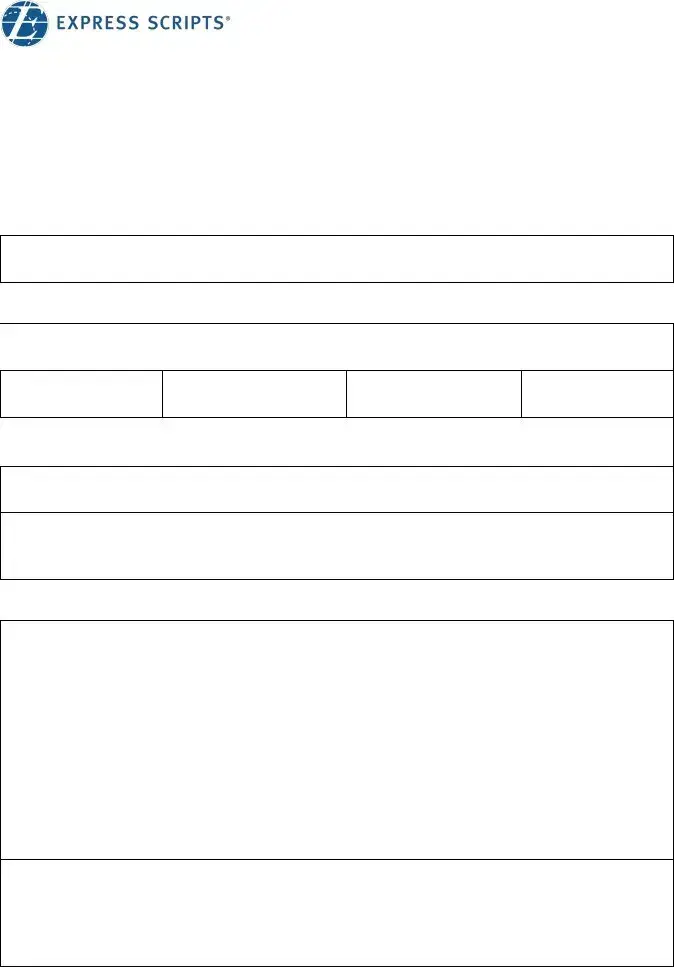
Request for Prior Authorization
Part B – Prescribing Doctor
Drugs in the Prior Authorization Program may be eligible for reimbursement only if the patient uses the drug(s) for Health Canada approved indication(s). Please provide information on your patient's medical condition and drug history, as required by the group benefit provider to reimburse this medication.
All information requested below is mandatory for the approval process, any fields left blank will result in an automatic denial. Please fill any
❒First time Prior Authorization application for this drug *Fill sections 1, 2 and 4*
❒Prior AuthorizationRenewal for this drug *Fill sections 1, 3 and 4*
SECTION 1 – DRUG REQUESTED
 Drug name:
Drug name:
Dose Administration (ex: oral, IV, etc) FrequencyDuration
 Medical condition:
Medical condition:
Will this drug be used according to its Health Canada approved indication(s)? |
❒ Yes ❒ No |
Site of drug administration: |
|
❒ Home ❒ Doctor office/Infusion clinic ❒ Hospital (outpatient) |
❒ Hospital (inpatient) |
SECTION 2 –
Any relevant information of the patient’s condition including the severity/stage/type of condition
Example: monthly frequency and duration for migraines, fibrosis status for Hepatitis C patient, lab values such as LDL and IgE levels, BMI, symptoms etc. (please do not provide genetic test information or results)
Therapies
Page 3
Request for Prior Authorization
Section 2 - Continued
Please list previously tried therapies
|
Duration of therapy |
Reason for cessation |
||
Drug |
Dosage and |
|
Inadequate/ |
Allergy/ |
|
administration |
|
||
|
From |
To |
Suboptimal |
Drug |
|
response |
Intolerance |
||
|
|
|
||
|
|
|
❒ |
❒ |
|
|
|
❒ |
❒ |
|
|
|
❒ |
❒ |
|
|
|
❒ |
❒ |
|
|
|
❒ |
❒ |
SECTION 3 – RENEWAL INFORMATION
 Date of treatment initiation:
Date of treatment initiation:
Details on clinical response to requested drug
Example: PASI/BASDAI, laboratory tests, etc. (please do not provide genetic test information or results)
If prior approval was not authorized by Express Script Canada, please attach a copy of the approval letter.
SECTION 4 – PRESCRIBER INFORMATION
Physician’s Name: |
|
Address: |
|
Tel: |
Fax: |
License No.: |
Specialty: |
Physician Signature: |
Date: |
Page 4
Form Characteristics
| Fact Name | Description |
|---|---|
| Who Completes the Form | The form must be completed by the plan member and the prescribing doctor in two parts. The plan member fills out Part A, while Part B is completed by the prescribing doctor. |
| Submission Process | After filling out both parts, the completed form can be submitted via fax or mail to Express Scripts Canada. The fax number is 1 (855) 712-6329, and the mailing address is 5770 Hurontario Street, 10th Floor, Mississauga, ON L5R 3G5. |
| Review Outcome | Completion of the form does not guarantee that the request will be approved. Approval depends on the review of the submission based on established clinical criteria. |
| Right to Appeal | If the request is denied, the plan member has the right to appeal the decision made by Express Scripts Canada. |
Guidelines on Utilizing Express Scripts Prior Authorization
Completing the Express Scripts Prior Authorization form is an important step for plan members seeking approval for specific medications. After you submit the completed form, Express Scripts Canada will review the request based on clinical criteria. You will eventually receive a notification regarding the outcome of your submission.
- Part A - Patient Information: As a plan member, fill out all required fields including your name, date of birth, and insurance details. Make sure to indicate your relationship to the insurance plan, your preferred language, and any relevant contact information.
- Patient Assistance Program: Indicate if you are enrolled in any patient support program and provide the necessary contact information if applicable.
- Provincial Coverage: Answer if you have applied for reimbursement under a provincial plan and detail the coverage decision, attaching any necessary documentation like the provincial decision letter.
- Primary Coverage: If applicable, indicate whether a reimbursement request has been submitted under your primary plan. Also supply the coverage decision along with the decision letter if necessary.
- Authorization: Sign and date the authorization section to allow your benefit provider to share your personal information for administrative purposes.
- Part B - Prescribing Doctor Information: Provide this form to your prescribing doctor to complete. They will need to fill out sections regarding the drug requested, including its name, dosage, administration details, frequency, and the medical condition it’s treating.
- First-Time Application or Renewal: The doctor must indicate if this is a first-time application or a renewal for the drug and fill out the corresponding fields accordingly.
- Section 1 - Drug Requested: Ensure the doctor includes details about the drug, its administration site, and whether it will be used according to its approved indications.
- Section 2 - First-Time Application: Provide details about the patient’s condition, any therapies being used, and previously tried therapies, if applicable. This information is critical for the approval process.
- Section 3 - Renewal Information: If this is a renewal, document the date of treatment initiation and any details regarding the clinical response to the drug.
- Section 4 - Prescriber Information: The prescriber must complete their information, including name, address, telephone, and signature to validate the form.
Once both parts are completed, fax or mail the entire form to Express Scripts Canada. Make sure to keep a copy for your records.
What You Should Know About This Form
What is the Express Scripts Prior Authorization form used for?
The Express Scripts Prior Authorization form is utilized when a plan member is prescribed a medication that requires prior authorization. This process helps ensure that the medication is covered under the plan member's drug benefit plan by verifying its appropriateness based on clinical criteria. The form must be completed in order to initiate a review for potential coverage of the prescribed medication.
How do I complete the Prior Authorization form?
Completing the form involves three straightforward steps. First, the plan member fills out Part A, providing necessary personal information. Next, the prescribing doctor completes Part B, which requires detailed information about the medical condition and the requested drug. Once completed, the form can be faxed or mailed to Express Scripts Canada using the provided contact information.
What happens after I submit the Prior Authorization form?
After submission, the request is reviewed by Express Scripts Canada. However, it's important to note that submitting the form does not guarantee approval. The review process is based on clinical criteria and supporting evidence to determine if the medication is necessary and appropriate for treatment. Both the plan member and the prescribing doctor will be notified of the decision.
What should I do if my Prior Authorization request is denied?
If the Prior Authorization request is denied, the plan member has the right to appeal the decision. This process typically involves reviewing the information submitted, and possibly providing additional evidence or documentation to support the request. Clear guidelines will often accompany the denial notification, indicating how to proceed with the appeal.
Are there any costs associated with completing the Prior Authorization form?
Any fees related to the completion and submission of the Prior Authorization form are the responsibility of the plan member. It is advisable to check with your insurance provider about any potential costs that may arise from this process to avoid unexpected expenses.
What information is required from the prescribing doctor?
The prescribing doctor needs to fill out Part B of the form, which includes mandatory information about the patient's medical condition, treatment history, and the specific drug being requested. Incomplete sections may result in automatic denial of the request, so precise and comprehensive details are crucial for a successful submission.
Common mistakes
Filling out the Express Scripts Prior Authorization form can be a daunting task. Many individuals make common mistakes that can lead to delays or denials of their medication requests. Understanding these missteps can help ensure a smoother process and potentially expedite approval.
One significant error is not completing all sections of the form. Both the patient and the prescribing doctor must provide detailed information. Omitting any mandatory fields, especially in Part B, can automatically result in denial. It is critical to take the time to fill out every section thoroughly. When faced with non-applicable fields, be sure to indicate this by writing ‘N/A’ to avoid any assumption that those sections were overlooked.
Another frequent oversight occurs in the patient history section. Providing vague or incomplete information about past therapies can negatively impact the evaluation. Specifics matter. It’s important to detail any previous medications tried, the duration, and the reasons for discontinuation. This type of information provides context that can bolster the case for the requested medication.
Some plan members fail to attach required documentation. If the form requests letters of approval or denial from provincial coverage or primary insurance, these documents should be included. Not doing so can lead to increased processing times or outright denials. Always check to ensure that any relevant decision letters are included before submission.
Additionally, neglecting to keep a copy of the submitted form is a mistake that can be easily avoided. Keeping a copy provides a reference point should you need to follow up. If questions arise later regarding the submission, having a detailed record can clarify any miscommunications and expedite resolution.
Another common pitfall involves the authorization section. Many individuals do not fully understand what they are consenting to. It’s crucial to read through the consent carefully and ensure that it is signed properly. Any discrepancies in signatures or dates can lead to further complications. Being meticulous in this area can prevent unnecessary back-and-forth communication.
Lastly, patients often underestimate the importance of timely submission. Delaying the request can lead to unnecessary interruptions in medication access. Submitting the form as soon as it is completed ensures that the process begins without unnecessary delay. Time is of the essence, especially when managing serious health conditions.
By recognizing these common mistakes, plan members can better prepare themselves for successful navigation of the Express Scripts Prior Authorization process. Attention to detail, complete information, and timely submissions are key to securing the necessary medication.
Documents used along the form
When seeking prior authorization for a medication through the Express Scripts form, several other documents and forms are often needed to supplement the request. Each of these plays a vital role in ensuring that the prior authorization process runs smoothly.
- Patient Medical History Form: This form outlines the patient's medical history, including previous medications, treatments, and any underlying health conditions that may affect the authorization request.
- Insurance Information Form: This document contains details about the patient's insurance plan, including coverage limits, exclusions, and maximum benefits, which are essential for determining eligibility.
- Doctor's Letter of Medical Necessity: A personalized letter from the prescribing doctor explaining why the specific medication is necessary for the patient's condition, often supporting the prior authorization request.
- Provincial Drug Coverage Decision Letter: If applicable, this letter provides the decision regarding the drug’s coverage under provincial plans, including whether it is approved or denied.
- Clinical Support Documentation: Additional documents such as lab results, imaging, or test results that provide further evidence supporting the medical need for the medication.
- Medication History Form: This form details past medications the patient has tried for their condition, including reasons for discontinuation, which helps illustrate the need for the new drug.
- Appeal Form: In cases of denial, this form is used to formally challenge the decision, providing reasons and additional evidence for reconsideration.
- Patient Consent Form: This document is signed by the patient, allowing their medical information to be shared with relevant parties involved in the prior authorization process.
- Prescription Record: A copy of the prescription that initiated the request, which must align with the medication being submitted for prior authorization.
Gathering and submitting these documents alongside the Express Scripts Prior Authorization form enhances the chances of a successful review and ultimately helps get the necessary medication delivered to the patient effectively.
Similar forms
The Express Scripts Prior Authorization form shares similarities with several other healthcare documents that facilitate approval processes for insurance coverage or medication reimbursement. Below is a list detailing five documents that serve a similar purpose:
- Medicare Prior Authorization Form: Like the Express Scripts form, this document requires both the patient and the prescribing physician to provide detailed information. It outlines the medical necessity for treatment and adheres to specific requirements set by Medicare for medication approval.
- Insurance Reimbursement Request Form: This form is used by patients to request reimbursement for out-of-pocket medical expenses. It necessitates the submission of supporting documentation, similar to how the prior authorization form requires clinical justification for medication use.
- Drug Claim Form: Much like the Express Scripts Prior Authorization form, a drug claim form requires patients to list their prescribed medications and relevant details. It also serves as a request for approval from the insurance company before the medication can be reimbursed.
- Appeal Letter for Denied Claims: Following a denial, patients can submit an appeal letter. This process mirrors the rights of patients to appeal decisions made through the prior authorization process, wherein additional information might be provided to support their case.
- Patient Assistance Program Application: This form is designed for patients seeking financial help with medication costs. Similar to the prior authorization, it requires personal and medical information to assess eligibility for support, ensuring the patient qualifies based on specific criteria.
Dos and Don'ts
When filling out the Express Scripts Prior Authorization form, certain practices can enhance the likelihood of a smooth approval process. Here are six important dos and don'ts to consider:
- Do complete all the required sections accurately. Incomplete forms may lead to automatic denial.
- Do attach any relevant documents, such as the provincial decision letter and previous approval letters, to support your request.
- Do consult with your prescribing doctor to ensure that all necessary medical information is provided.
- Do submit your form through the specified method, either by faxing or mailing it directly to Express Scripts Canada.
- Don't leave any fields blank. If a field isn't applicable, write 'N/A' to avoid misunderstandings.
- Don't assume that submission guarantees approval; ensure that you understand the criteria used for review.
By following these guidelines, you can help facilitate a more efficient review process for your Prior Authorization request.
Misconceptions
Misunderstandings about the Express Scripts Prior Authorization form can lead to frustration and delays. Here are ten common misconceptions:
- The form guarantees approval. Many assume submitting the form guarantees that the medication will be approved. However, the completion and submission do not ensure reimbursement. Approval is based on specific clinical criteria.
- Only physicians need to be involved. Some believe that the physician is solely responsible for the process. In reality, the plan member also has significant responsibilities. They must complete Part A of the form themselves.
- The process is only for new medications. It is a common misconception that prior authorization is required only for new prescriptions. In fact, renewal requests for medications already being taken can also require prior authorization.
- There are no fees associated with the form. Many people think that completing the form comes at no cost. However, any associated fees, such as those for obtaining medical records or consultations, fall on the plan member.
- Only insurance companies determine approval. Some may think that only the insurance provider makes the decision. The approval process also heavily relies on guidelines and criteria established by Express Scripts Canada, which must be followed.
- Appealing a denial is not possible. A denial can feel final to some, leading them to think there are no recourse options. However, plan members have the right to appeal decisions made by Express Scripts Canada.
- Only English-language submissions are accepted. While many might assume that English is the only language for the form, an option for French is also provided, increasing accessibility for more people.
- A faxed form is not valid. Some may believe that faxed submissions lack legitimacy. In fact, Express Scripts Canada accepts faxed forms as valid for their records and processing.
- There is no personal information consent required. Many overlook the importance of giving consent for personal information exchange. The form requires that plan members authorize this exchange to facilitate handling their request.
- The doctor must fill out the form from scratch. Some may think that the prescribing doctor must rewrite everything. However, if the medication has been used before, certain information can be reused from previous applications if relevant.
Understanding these misconceptions can help pave the way for a smoother experience with the prior authorization process.
Key takeaways
Plan members must complete and submit the Prior Authorization form when prescribed medication requiring prior approval.
The responsibility for any fees associated with completing the form falls on the plan member.
The process includes three steps:
- Plan member completes Part A.
- Prescribing doctor completes Part B.
- Form is faxed or mailed to Express Scripts Canada.
The completed form can be faxed to 1 (855) 712-6329 or mailed to Express Scripts Canada at their designated address.
Submission of the form does not guarantee approval; requests will be reviewed based on clinical criteria.
Only if approved by Express Scripts Canada, will the plan member receive reimbursement for the prescribed medication.
Plan members have the right to appeal a denial decision made by Express Scripts Canada.
Plan members will receive notification regarding the approval or denial of their request.
If requested, the prescribing doctor will also be informed of the decision via fax.
All information requested on the form is mandatory; incomplete forms may lead to an automatic denial.
Browse Other Templates
Vehicle Inspection Pdf - The form collects inspector qualifications, ensuring that only trained individuals conduct safety assessments.
Incident Form in Hospital - This report enhances accountability for medication administration within childcare facilities.
Pennsylvania Llc Filing Requirements - The application for an FEIN can be an immediate step following form completion.