Fill Out Your Physical Exam Form
The Physical Exam form is an essential document that ensures the health and safety of school-age students. This form collects comprehensive information about a student's health history, current medications, allergies, and any existing medical conditions. Parents or guardians are asked to complete the first page before the exam, which includes key details such as the student's name, date of birth, and a checklist of potential health issues ranging from respiratory problems to learning disabilities. The examination section addresses vital signs like height, weight, and blood pressure, while also gathering details on vision, hearing, and musculoskeletal health. Furthermore, immunization history is documented to ensure compliance with school health requirements. Family health history is meticulously considered, as it can spotlight hereditary conditions that may affect the student. This thorough assessment is designed to identify any health concerns that may hinder a student's participation in school activities, thus promoting a safe educational environment.
Physical Exam Example
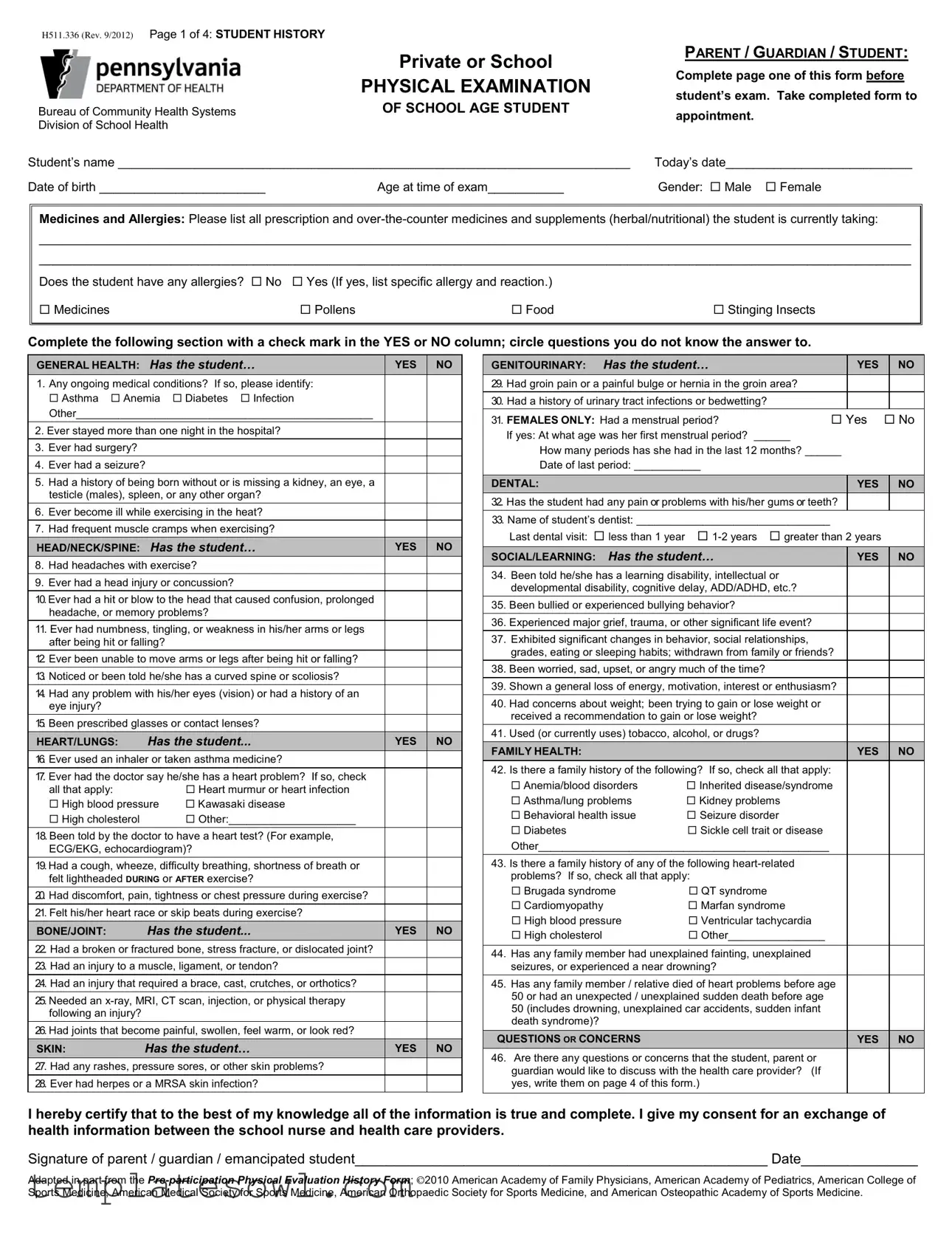
H511.336 (Rev. 9/2012) Page 1 of 4: STUDENT HISTORY
|
Private or School |
|
PHYSICAL EXAMINATION |
Bureau of Community Health Systems |
OF SCHOOL AGE STUDENT |
Division of School Health |
|
Student’s name __________________________________________________________________________
Date of birth ________________________ |
Age at time of exam___________ |
PARENT / GUARDIAN / STUDENT:
Complete page one of this form before student’s exam. Take completed form to
appointment.
Today’s date___________________________
Gender: Male Female
Medicines and Allergies: Please list all prescription and
______________________________________________________________________________________________________________________________
______________________________________________________________________________________________________________________________
Does the student have any allergies? No Yes (If yes, list specific allergy and reaction.)
Medicines |
Pollens |
Food |
Stinging Insects |
|
|
|
|
Complete the following section with a check mark in the YES or NO column; circle questions you do not know the answer to.
|
GENERAL HEALTH: Has the student… |
|
|
|
|
||
|
|
YES |
|
NO |
|||
|
1. Any ongoing medical conditions? If so, please identify: |
|
|
|
|
||
|
Asthma Anemia |
Diabetes Infection |
|
|
|
|
|
|
Other_________________________________________________ |
|
|
|
|
||
|
|
|
|
|
|||
2. Ever stayed more than one night in the hospital? |
|
|
|
|
|||
|
|
|
|
|
|
|
|
3. Ever had surgery? |
|
|
|
|
|
|
|
4. Ever had a seizure? |
|
|
|
|
|
||
|
|
|
|
|
|||
5. Had a history of being born without or is missing a kidney, an eye, a |
|
|
|
|
|||
|
testicle (males), spleen, or any other organ? |
|
|
|
|
||
6. Ever become ill while exercising in the heat? |
|
|
|
|
|||
7. Had frequent muscle cramps when exercising? |
|
|
|
|
|||
|
|
|
|
|
|
||
|
HEAD/NECK/SPINE: Has the student… |
|
YES |
|
NO |
||
8. Had headaches with exercise? |
|
|
|
|
|||
|
|
|
|
|
|||
9. Ever had a head injury or concussion? |
|
|
|
|
|||
|
|
|
|
|
|||
10.Ever had a hit or blow to the head that caused confusion, prolonged |
|
|
|
|
|||
|
headache, or memory problems? |
|
|
|
|
||
11. Ever had numbness, tingling, or weakness in his/her arms or legs |
|
|
|
|
|||
|
after being hit or falling? |
|
|
|
|
|
|
|
|
|
|
|
|||
12. Ever been unable to move arms or legs after being hit or falling? |
|
|
|
|
|||
13. Noticed or been told he/she has a curved spine or scoliosis? |
|
|
|
|
|||
|
|
|
|
|
|||
14. Had any problem with his/her eyes (vision) or had a history of an |
|
|
|
|
|||
|
eye injury? |
|
|
|
|
|
|
15. Been prescribed glasses or contact lenses? |
|
|
|
|
|||
|
HEART/LUNGS: |
Has the student... |
|
YES |
|
NO |
|
16. Ever used an inhaler or taken asthma medicine? |
|
|
|
|
|||
17. Ever had the doctor say he/she has a heart problem? If so, check |
|
|
|
|
|||
|
all that apply: |
|
Heart murmur or heart infection |
|
|
|
|
|
High blood pressure |
Kawasaki disease |
|
|
|
|
|
|
High cholesterol |
|
Other:_____________________ |
|
|
|
|
18. Been told by the doctor to have a heart test? (For example, |
|
|
|
|
|||
|
ECG/EKG, echocardiogram)? |
|
|
|
|
||
|
|
|
|
|
|||
19.Had a cough, wheeze, difficulty breathing, shortness of breath or |
|
|
|
|
|||
|
felt lightheaded DURING or AFTER exercise? |
|
|
|
|
||
|
|
|
|
|
|||
20. Had discomfort, pain, tightness or chest pressure during exercise? |
|
|
|
|
|||
|
|
|
|
|
|||
21. Felt his/her heart race or skip beats during exercise? |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
BONE/JOINT: |
Has the student... |
|
YES |
|
NO |
|
22. Had a broken or fractured bone, stress fracture, or dislocated joint? |
|
|
|
|
|||
|
|
|
|
|
|||
23. Had an injury to a muscle, ligament, or tendon? |
|
|
|
|
|||
24. Had an injury that required a brace, cast, crutches, or orthotics? |
|
|
|
|
|||
|
|
|
|
|
|||
25. Needed an |
|
|
|
|
|||
|
following an injury? |
|
|
|
|
|
|
|
|
|
|
|
|||
26. Had joints that become painful, swollen, feel warm, or look red? |
|
|
|
|
|||
|
SKIN: |
Has the student… |
|
YES |
|
NO |
|
27. Had any rashes, pressure sores, or other skin problems? |
|
|
|
|
|||
28. Ever had herpes or a MRSA skin infection? |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
Has the student… |
|
|
|
|
|
|
|
|
||
|
GENITOURINARY: |
|
|
YES |
|
|
|
NO |
|
|||
|
29. Had groin pain or a painful bulge or hernia in the groin area? |
|
|
|
|
|
|
|
|
|||
|
30. Had a history of urinary tract infections or bedwetting? |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|||||||
|
31. FEMALES ONLY: Had a menstrual period? |
Yes |
No |
|||||||||
|
|
If yes: At what age was her first menstrual period? ______ |
|
|
|
|
|
|
|
|
||
|
|
How many periods has she had in the last 12 months? ______ |
|
|
|
|
||||||
|
|
Date of last period: ___________ |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|||
|
DENTAL: |
|
|
|
|
YES |
|
|
NO |
|||
|
32. Has the student had any pain or problems with his/her gums or teeth? |
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|||
|
33. Name of student’s dentist: ________________________________ |
|
|
|
|
|
|
|
|
|||
|
|
Last dental visit: less than 1 year |
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
||||
|
SOCIAL/LEARNING: |
Has the student… |
|
|
YES |
|
|
NO |
||||
34. |
Been told he/she has a learning disability, intellectual or |
|
|
|
|
|
|
|
|
|||
|
|
developmental disability, cognitive delay, ADD/ADHD, etc.? |
|
|
|
|
|
|
|
|
||
35. |
Been bullied or experienced bullying behavior? |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|||
36. |
Experienced major grief, trauma, or other significant life event? |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|||
37. |
Exhibited significant changes in behavior, social relationships, |
|
|
|
|
|
|
|
|
|||
|
|
grades, eating or sleeping habits; withdrawn from family or friends? |
|
|
|
|
|
|||||
38. |
Been worried, sad, upset, or angry much of the time? |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
||||||
39. |
Shown a general loss of energy, motivation, interest or enthusiasm? |
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|||
40. |
Had concerns about weight; been trying to gain or lose weight or |
|
|
|
|
|
|
|
|
|||
|
|
received a recommendation to gain or lose weight? |
|
|
|
|
|
|
|
|
||
41. |
Used (or currently uses) tobacco, alcohol, or drugs? |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|||
|
FAMILY HEALTH: |
|
|
|
|
YES |
|
|
|
NO |
|
|
42. |
Is there a family history of the following? If so, check all that apply: |
|
|
|
|
|
|
|
|
|||
|
|
Anemia/blood disorders |
Inherited disease/syndrome |
|
|
|
|
|
||||
|
|
Asthma/lung problems |
Kidney problems |
|
|
|
|
|
|
|
|
|
|
|
Behavioral health issue |
Seizure disorder |
|
|
|
|
|
|
|
|
|
|
|
Diabetes |
|
Sickle cell trait or disease |
|
|
|
|
|
|
|
|
|
Other________________________________________________ |
|
|
|
|
|
|
|
|
|||
43. |
Is there a family history of any of the following |
|
|
|
|
|
|
|
|
|||
|
|
problems? If so, check all that apply: |
|
|
|
|
|
|
|
|
||
|
Brugada syndrome |
QT syndrome |
|
|
|
|
|
|
|
|
||
|
|
Cardiomyopathy |
|
Marfan syndrome |
|
|
|
|
|
|
|
|
|
|
High blood pressure |
Ventricular tachycardia |
|
|
|
|
|
|
|
|
|
|
|
High cholesterol |
|
Other________________ |
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|||
44. |
Has any family member had unexplained fainting, unexplained |
|
|
|
|
|
|
|
|
|||
|
|
seizures, or experienced a near drowning? |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
||||||
45. |
Has any family member / relative died of heart problems before age |
|
|
|
|
|
||||||
|
|
50 or had an unexpected / unexplained sudden death before age |
|
|
|
|
|
|
|
|
||
|
|
50 (includes drowning, unexplained car accidents, sudden infant |
|
|
|
|
|
|
|
|
||
|
|
death syndrome)? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
QUESTIONS OR CONCERNS |
|
|
|
YES |
|
|
|
NO |
|
||
46. |
Are there any questions or concerns that the student, parent or |
|
|
|
|
|
|
|
|
|||
|
|
guardian would like to discuss with the health care provider? (If |
|
|
|
|
|
|
|
|
||
|
|
yes, write them on page 4 of this form.) |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
I hereby certify that to the best of my knowledge all of the information is true and complete. I give my consent for an exchange of health information between the school nurse and health care providers.
Signature of parent / guardian / emancipated student_____________________________________________________ Date_______________
Adapted in part from the
Page 2 of 4: PHYSICAL EXAM
STUDENT’S HEALTH HISTORY (page 1 of this form) REVIEWED PRIOR TO PERFOMING EXAMINATION: Yes |
No |
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CHECK ONE |
|
|
|
||
Physical exam for grade: |
|
|
|
|
|
|
|
|||
|
NORMAL |
*ABNORMAL |
DEFER |
|
|
|
||||
K/1 6 11 |
Other |
*ABNORMAL FINDINGS / RECOMMENDATIONS / REFERRALS |
|
|||||||
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
Height: |
( |
|
) inches |
|
|
|
|
|
|
|
Weight: |
( |
|
) pounds |
|
|
|
|
|
|
|
BMI: |
( |
|
) |
|
|
|
|
|
|
|
|
) % |
|
|
|
|
|
|
|||
Pulse: |
( |
|
) |
|
|
|
|
|
|
|
Blood Pressure: |
( |
/ |
) |
|
|
|
|
|
|
|
Hair/Scalp |
|
|
|
|
|
|
|
|
|
|
Skin |
|
|
|
|
|
|
|
|
|
|
Eyes/Vision |
Corrected |
|
|
|
|
|
|
|||
Ears/Hearing |
|
|
|
|
|
|
|
|
|
|
Nose and Throat |
|
|
|
|
|
|
|
|
|
|
Teeth and Gingiva |
|
|
|
|
|
|
|
|
||
Lymph Glands |
|
|
|
|
|
|
|
|
|
|
Heart |
|
|
|
|
|
|
|
|
|
|
Lungs |
|
|
|
|
|
|
|
|
|
|
Abdomen |
|
|
|
|
|
|
|
|
|
|
Genitourinary |
|
|
|
|
|
|
|
|
|
|
Neuromuscular System |
|
|
|
|
|
|
|
|
||
Extremities |
|
|
|
|
|
|
|
|
|
|
Spine (Scoliosis) |
|
|
|
|
|
|
|
|
|
|
Other |
|
|
|
|
|
|
|
|
|
|
|
|
TUBERCULIN TEST |
DATE APPLIED |
|
|
DATE READ
MEDICAL CONDITIONS OR CHRONIC DISEASES WHICH REQUIRE MEDICATION, RESTRICTION OF ACTIVITY, OR WHICH MAY AFFECT EDUCATION
(Additional space on page 4)
Parent/guardian present during exam: Yes |
No |
|
|
Physical exam performed at: Personal Health Care Provider’s Office |
School |
Date of exam______________20______ |
|
Print name of examiner _______________________________________________________________________________________________________
Print examiner’s office address___________________________________________________________________ Phone_______________________
Signature of examiner______________________________________________________________________ MD DO PAC CRNP
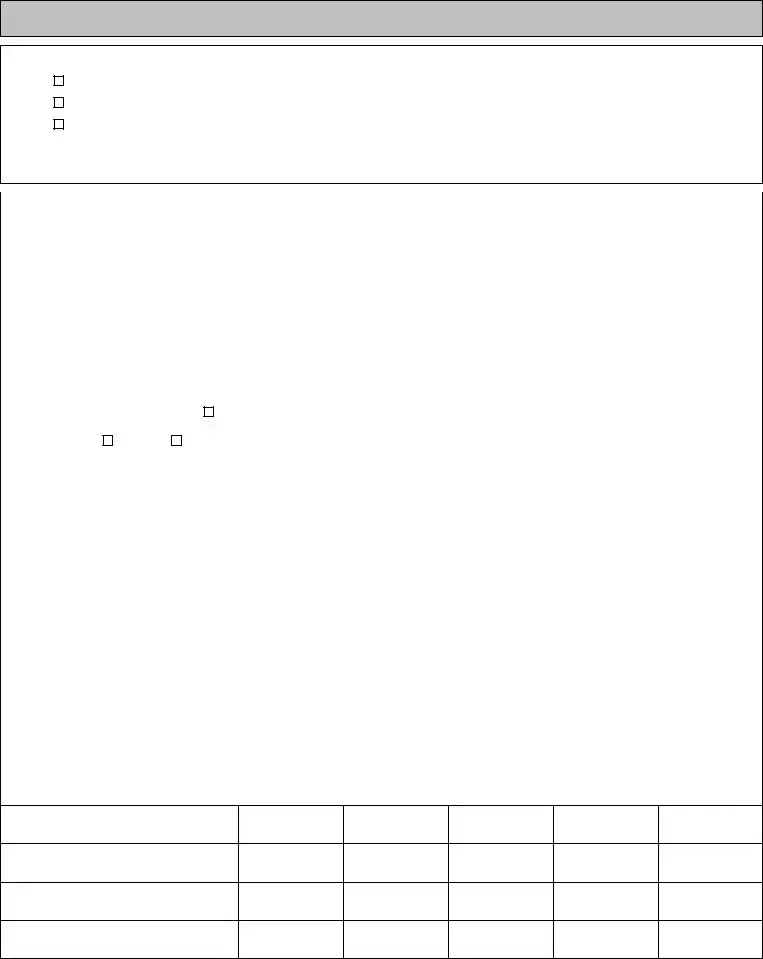
Page 3 of 4: IMMUNIZATION HISTORY
HEALTH CARE PROVIDERS: Please photocopy immunization history from student’s record – OR – insert information below.
IMMUNIZATION EXEMPTION(S):
Medical |
Date Issued:___________ |
Reason: __________________________________________________ |
Date Rescinded:___________ |
Medical |
Date Issued:___________ |
Reason: __________________________________________________ |
Date Rescinded:___________ |
Medical |
Date Issued:___________ |
Reason: __________________________________________________ |
Date Rescinded:___________ |
NOTE: The parent/guardian must provide a written request to the school for a religious or philosophical exemption.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
VACCINE |
|
|
|
DOCUMENT: (1) Type of vaccine; (2) Date (month/day/year) for each immunization |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Diphtheria/Tetanus/Pertussis (child) |
|
|
|
|
|
|
|
|
|
||
|
Type: DTaP, DTP or DT |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Diphtheria/Tetanus/Pertussis |
|
1 |
|
2 |
3 |
4 |
5 |
|
|||
|
|
|
|
|
|
|
|
|
|
|||
|
(adolescent/adult) |
|
|
|
|
|
|
|
|
|
|
|
|
Type: Tdap or Td |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Polio |
|
|
|
|
|
|
|
|
|
|
|
|
Type: OPV or IPV |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Hepatitis B |
(HepB) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Measles/Mumps/Rubella (MMR) |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|||
|
Mumps disease diagnosed by physician |
|
|
Date:__________ |
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Varicella: |
Vaccine |
Disease |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Serology: (Identify Antigen/Date/POS or NEG) |
|
|
|
|
|
|
|
|
|
||
|
i.e. Hep B, Measles, Rubella, Varicella |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Meningococcal Conjugate Vaccine (MCV4) |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Human Papilloma Virus (HPV) |
|
|
|
|
|
|
|
|
|
||
|
Type: HPV2 or HPV4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Influenza |
|
|
|
6 |
|
7 |
8 |
9 |
10 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Type: TIV (injected) |
|
|
|
|
|
|
|
|
|
|
|
|
LAIV (nasal) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
11 |
|
12 |
13 |
14 |
15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Haemophilus Influenzae Type b (Hib) |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Pneumococcal Conjugate Vaccine (PCV) |
|
|
|
|
|
|
|
|
|
||
|
Type: 7 or 13 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Hepatitis A (HepA) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
2 |
3 |
4 |
5 |
|
|
|
Rotavirus |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Other Vaccines: (Type and Date)
Page 4 of 4: ADDITIONAL COMMENTS (PARENT / GUARDIAN / STUDENT / HEALTH CARE PROVIDER)
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of the Physical Exam Form | The Physical Exam form is designed to gather comprehensive health information about students to ensure they are fit for school activities. It helps identify any potential health issues that may affect their participation in sports or other physical activities. |
| Completion Requirement | Parents, guardians, or emancipated students must complete the first page of this form before the examination. It should be presented at the healthcare appointment to ensure that the provider has all necessary background information. |
| Confidentiality of Information | The information provided on this form is confidential and will only be shared with the appropriate school personnel and healthcare providers as necessary for the student’s well-being. |
| Governing Laws | This form is governed by state-specific requirements for school health services, including laws such as the Individuals with Disabilities Education Act (IDEA) and state-specific legislation related to student health assessments. |
Guidelines on Utilizing Physical Exam
Completing the Physical Exam form is an essential step in ensuring the well-being of a student before their medical examination. This process involves gathering vital health information that will assist healthcare professionals in understanding the student's medical history and current status. After filling out the form, it should be taken to the appointment where the student will undergo the physical exam.
- Write the student's name at the top of the form.
- Fill in the date of birth and age at the time of the exam.
- Indicate today's date.
- Select the student's gender by marking either "Male" or "Female."
- List all prescription and over-the-counter medications, vitamins, and supplements currently being taken by the student.
- Answer the allergy question by checking "No" or "Yes." If yes, specify the type of allergy and the associated reaction.
- For the general health section, check "YES" or "NO" for each item. Circle any questions where the answer is unknown.
- Proceed to the head/neck/spine, heart/lungs, bone/joint, skin, genitourinary, dental, social/learning, and family health sections. Again, check "YES" or "NO" for each statement, circling if unsure.
- In the questions or concerns section, note any specific questions or issues to discuss with the healthcare provider.
- Lastly, ensure the parent or guardian signs the form to certify the accuracy of the information provided and the consent for necessary communications with health care providers.
What You Should Know About This Form
What is a Physical Exam form and why is it necessary?
A Physical Exam form is a document that captures important health information about a student prior to their physical examination. This form is vital as it helps healthcare providers understand the student's medical history, ongoing health issues, and any potential risks associated with physical activities. Schools often require this form to ensure that students are fit to participate in sports or physical education classes safely.
How should I fill out the Physical Exam form?
To fill out the Physical Exam form, begin by providing accurate details about the student, including their name, date of birth, and age. Next, disclose any current medications or allergies. Complete the sections regarding general health, head/neck/spine, heart/lungs, and other relevant areas by checking "YES" or "NO" and circling any questions that you may not know the answers to. Ensure you have all necessary information before taking the form to the health care appointment.
What should I do if my child has a pre-existing medical condition?
If your child has a pre-existing medical condition, it is essential to indicate this on the form. Be specific about the condition and any ongoing treatments or medications. This information is crucial for the health care provider to make appropriate recommendations and ensure your child's safety during any physical activities.
How is the information from the Physical Exam form used?
The information collected from the Physical Exam form is reviewed by healthcare providers to assess the student’s health status before the examination. It aids in identifying any restrictions or modifications needed to accommodate the student’s health needs in physical activities. Additionally, it may be shared with school nurses and teachers to ensure a comprehensive understanding of the student's health for their wellbeing during school activities.
What if my child requires accommodations due to a medical condition?
If your child requires accommodations, it is important to discuss these needs with the health care provider during the examination. The form is designed to identify any medical issues that could warrant such accommodations. Based on the findings, healthcare providers can offer recommendations to the school about necessary adjustments, whether it's related to physical education or other activities.
Is it necessary to provide a signature on the Physical Exam form?
Yes, signing the Physical Exam form is a crucial step. The signature certifies that the information you provided is accurate to the best of your knowledge. It also gives consent for the exchange of health information between the school nurse and health care providers, which is important for ensuring that everyone involved in the student's care has access to relevant health information.
Common mistakes
Completing the Physical Exam form accurately is essential for ensuring the well-being of the student. However, several common mistakes can hinder this process. One frequent error is failing to provide complete and detailed information regarding the student’s medical history. Omitting important details, such as past surgeries or ongoing medical conditions, could lead health care providers to misunderstand the student’s current health situation. It is vital to be thorough and precise when detailing these aspects.
Another often overlooked area is the section pertaining to medications and allergies. Parents or guardians may forget to list over-the-counter medicines or supplements that the student might be taking. This oversight is critical, as many medications can interact with each other or exacerbate existing health issues. Additionally, if a student has allergies, it is imperative to provide complete information—merely checking "yes" without specifying the allergens or reactions can leave healthcare providers ill-prepared for potential emergencies.
The use of check marks in the general health section also requires careful attention. Miscommunication can occur if a parent checks "no" for a health issue that they are unsure about. For instance, failing to mark a family history of certain conditions could lead to missed opportunities for early intervention or monitoring. Health history forms are designed to provide insight, and this information should always be approached with honesty and clarity.
When it comes to family health history, another common mistake is not checking all relevant health issues. Many parents may assume that since they or their partners are healthy, there is no need to include potential genetic predispositions to certain diseases. This approach can overlook important connections pertinent to the student’s future health care needs. Listing all known family health problems fosters a more comprehensive understanding of risk factors.
Another challenge arises from the ability to remember dates accurately. For instance, noting the date of the last dental visit or the date when certain vaccinations were administered may be difficult. If these details are misremembered or left blank, it can complicate the follow-up process for preventive care and other necessary health measures.
Finally, one must emphasize the importance of ensuring all sections of the form are completed. Leaving questions unanswered or blank may lead to assumptions or additional follow-up, which can create delays in receiving care. A well-prepared form not only aids in providing immediate care but also strengthens the long-term health monitoring of the student.
Documents used along the form
The Physical Exam form is an essential document used in the healthcare process for school-aged students. However, several other forms accompany it to ensure a comprehensive understanding of the student's health and history. Here is a brief overview of five forms commonly used alongside the Physical Exam form.
- Immunization Record: This form provides proof of vaccinations that the student has received. It is critical for assessing the student’s immunity to certain diseases and ensuring compliance with school health regulations.
- Health History Questionnaire: Parents or guardians complete this document to provide detailed information about the student’s medical history. It usually covers past illnesses, surgeries, and any chronic conditions that could impact the student’s health.
- Medication Administration Form: This form allows parents to authorize school staff to administer medications to their child during school hours. It specifies the medication, dosage, and administration schedule to ensure the child’s safety and well-being.
- Consent for Treatment Form: Parents or guardians must sign this form to give healthcare providers permission to perform medical examinations and treatments on their child. It is especially important in emergency situations.
- Emergency Contact Form: This form lists individuals to contact in case of a medical emergency involving the student. Having this information readily available helps ensure swift action and communication during critical times.
These forms collectively support the health and safety of students, promoting an environment conducive to learning and growth. Ensuring that all necessary documentation is completed and filed will help facilitate any required healthcare interventions.
Similar forms
The Physical Exam form shares similarities with several other important documents that capture health and medical information. Each document serves a unique purpose but often overlaps in the type of information collected. The following list outlines these comparable documents:
- Health History Questionnaire: This document gathers comprehensive background information about an individual's medical history, including past illnesses, surgeries, and family health concerns. Like the Physical Exam form, it aims to assess ongoing health issues relevant to future medical care.
- Immunization Record: Tracking vaccinations is crucial for student health, much like the Physical Exam form. It details specific immunizations received, dates administered, and any exemptions. Both documents play essential roles in school health requirements.
- Emergency Health Information Form: This document is designed to provide critical health details in case of emergencies. It includes allergies, medical conditions, and emergency contacts, mirroring the Physical Exam form's emphasis on health-related information.
- Consent Form for Medical Treatment: This form indicates a parent or guardian's approval for medical procedures or treatments for their child. Similar to the Physical Exam form, it highlights the importance of informed consent in healthcare.
- Pre-Participation Physical Evaluation History Form: Used primarily in sports, this document assesses an individual’s readiness to participate in athletic activities. Like the Physical Exam form, it screens for medical conditions that might affect participation.
- Chronic Illness Management Plan: Designed for students with ongoing health issues, this document outlines management strategies and accommodations necessary for their care. Both forms ensure that healthcare providers understand the student’s health status and needs.
- Behavioral Health Screening Form: This document evaluates mental health conditions and psychological well-being. Similar to the Physical Exam form, it addresses components of health that can impact overall student performance and functioning.
Dos and Don'ts
Things to Do:
- Fill out all relevant sections completely.
- Provide accurate information about medications and allergies.
- Check all applicable health conditions honestly.
- Bring the completed form to the appointment.
- Verbalize any questions or concerns to the healthcare provider.
- Ensure the form is dated and signed where required.
- Ask for clarification on any section that is unclear.
Things to Avoid:
- Do not leave any mandatory fields blank.
- Avoid ambiguous answers; be as specific as possible.
- Do not forget to include a family health history if applicable.
- Refrain from providing outdated medical information.
- Do not ignore sections that pertain to mental health.
- Do not hesitate to ask for help if needed.
- Never assume the healthcare provider has access to prior records.
Misconceptions
- Misconception 1: The Physical Exam form is only for sports participation.
- Misconception 2: Parents don’t need to fill out the form before the exam.
- Misconception 3: Allergies are not important to disclose.
- Misconception 4: Only serious medical conditions need to be reported.
- Misconception 5: The form does not affect school health policies.
- Misconception 6: Completing the physical exam form takes too much time.
- Misconception 7: The form is only for new students.
This form is not exclusively for sports. It serves as a comprehensive health assessment for school-age students, covering various health areas that influence overall well-being and ability to learn.
It is crucial for parents or guardians to complete the first page of the form before the appointment. This information helps the healthcare provider understand the student’s health status and medical history.
Disclosing any allergies is vital. Knowing a student’s allergies helps the healthcare provider take necessary precautions during the exam and ensures the safety of the student.
All medical conditions, even minor ones, should be reported. This provides a complete picture of the student’s health and can help identify potential risks during physical activities.
The information collected can influence school health policies and individual accommodations for students. Accurate and complete details help schools cater to the needs of their students effectively.
While it may seem lengthy, many sections can be completed quickly, especially if parents have the necessary information at hand. The time spent is trivial compared to the benefits of having a health assessment for the student.
The Physical Exam form is for all students, regardless of whether they are new or returning. Regular updates on health information are important for ongoing monitoring of each student's well-being.
Key takeaways
Ensure that the first page of the form is completed by the parent, guardian, or student before the physical exam. This includes providing personal details like the student’s name, date of birth, and medications.
Clearly indicate any current medications or allergies. Use the designated sections to specify prescription drugs, over-the-counter products, and known allergies.
Answer all health history questions honestly. This includes ongoing medical conditions, previous hospitalizations, and any relevant family health history.
Bring the completed form to the examination appointment. This ensures that the healthcare provider has all necessary information prior to performing the exam.
Review and discuss any concerns in the designated section of the form. Communication with the healthcare provider can address important issues that may affect the student’s health and educational experience.
Browse Other Templates
Dog Adoption Paperwork - We look forward to bringing joy into your home.
Uc-44fr - Communication between inspectors and licensees will play a key role in compliance.