Fill Out Your Fim Scale Form
The Functional Independence Measure (FIM) Scale is a vital tool used in assessing an individual's functional abilities following an injury or medical event. It focuses on six key areas of functionality, including self-care, mobility, communication, psychosocial adjustment, and cognitive function. Each area is assessed using a range of 1 to 7, where a score of 7 indicates complete independence and a score of 1 signifies total dependence. The FIM Scale provides a standardized framework that healthcare professionals can use to evaluate the level of assistance an individual may require in daily activities. For instance, self-care items address essential tasks such as feeding, bathing, and dressing, while mobility items evaluate the ease of transferring between different positions and moving within the community. The scale not only enhances communication regarding patient needs among healthcare providers but also serves as a foundation for setting rehabilitation goals and measuring progress over time. By incorporating subjective insights together with objective measures, the FIM Scale aims to offer a comprehensive assessment of functional independence, thereby guiding both treatment plans and patient outcomes.
Fim Scale Example
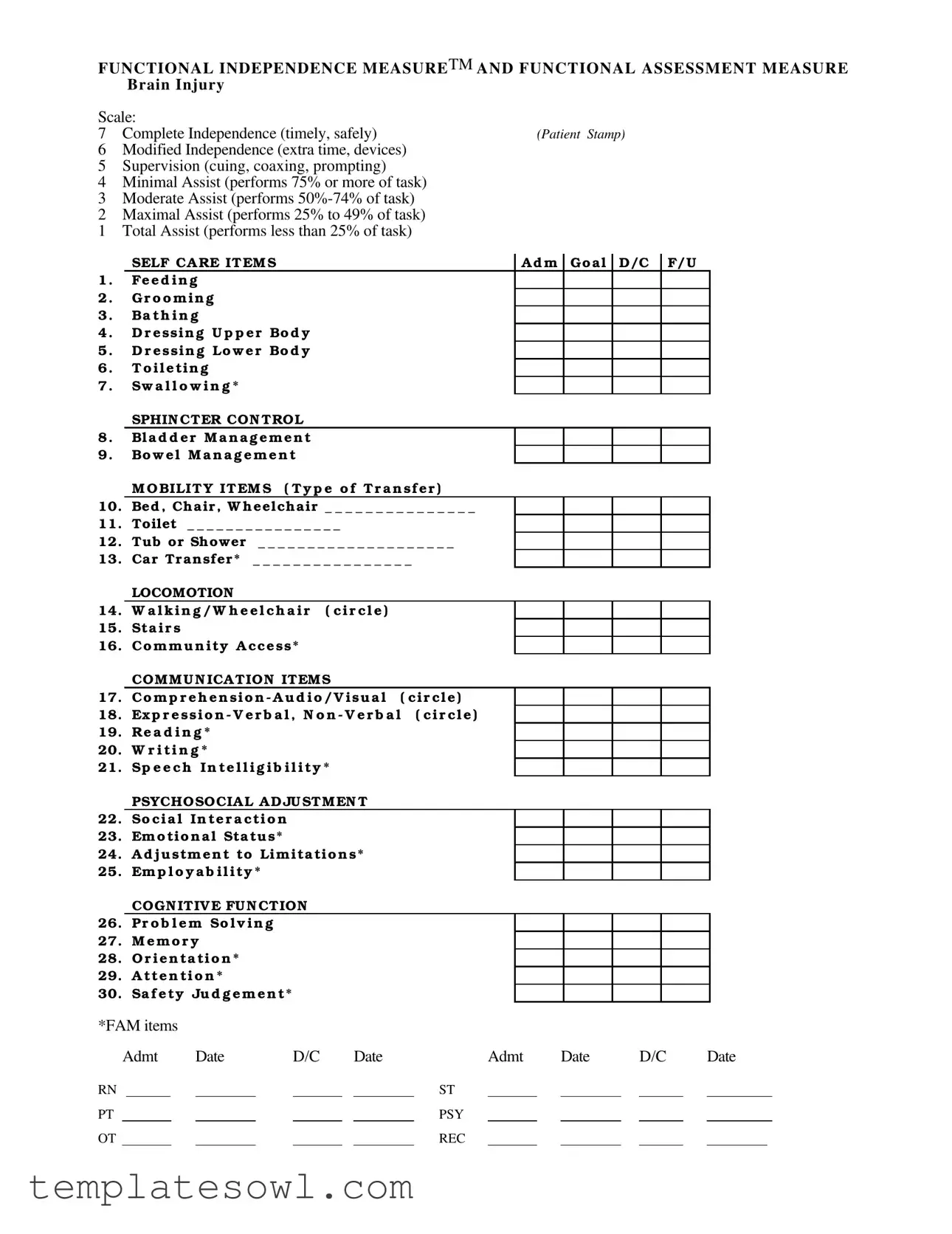
FUNCTIONAL INDEPENDENCE MEASURETM AND FUNCTIONAL ASSESSMENT MEASURE
BRAIN INJURY
Scale: |
|
7 Complete Independence (timely, safely) |
(Patient Stamp) |
6Modified Independence (extra time, devices)
5Supervision (cuing, coaxing, prompting)
4Minimal Assist (performs 75% or more of task)
3Moderate Assist (performs
2Maximal Assist (performs 25% to 49% of task)
1Total Assist (performs less than 25% of task)
|
SELF CA RE IT EM S |
|
A d m |
Go a l |
D/C |
F/U |
|
1 . |
Fe e d i n g |
|
|
|
|
|
|
2 . |
G r o o m i n g |
|
|
|
|
|
|
3 . |
Ba t h i n g |
|
|
|
|
|
|
4 . |
D r e ssin g U p p e r Bo d y |
|
|
|
|
|
|
5 . |
D r e ssi n g Lo w e r Bo d y |
|
|
|
|
|
|
6 . |
T o i l e ti n g |
|
|
|
|
|
|
7 . |
Sw a l l o w i n g * |
|
|
|
|
|
|
|
SPHIN CTER CON TROL |
|
|
|
|
|
|
8 . |
Bl a d d e r M a n a g e m e n t |
|
|
|
|
|
|
9 . |
Bo w e l M a n a g e m e n t |
|
|
|
|
|
|
|
M O BILIT Y IT EM S ( T y p e o f T r a n sf e r ) |
||||||
10. |
Bed , Ch air , W h eelch air _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ |
|
|
|
|
||
11. |
Toilet _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ |
|
|
|
|
||
12. |
Tub or Shower |
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ |
|
|
|
|
|
13. |
Car Tr ansfer * |
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ |
|
|
|
|
|
|
LOCOMOTION |
|
|
|
|
|
|
14. |
W a l k i n g / W h e e l c h a i r |
( c i r c l e ) |
|||||
15.Sta i r s
16.Co m m u n i ty A cce ss*
|
COM M U N ICA TION ITEM S |
17. |
Co m p r e h e n si o n - A u d i o / V i su a l ( ci r cl e ) |
18. |
Ex p r e s s i o n - V e r b a l , N o n - V e r b a l ( ci r cl e ) |
19.Re a d i n g *
20.W r i t i n g *
21.Sp e e c h I n t e l l i g i b i l i t y *
PSYCHOSOCIA L A D JU STM EN T
22.So ci a l In te r a cti o n
23.Em o tio n a l Sta tu s*
24.A d j u stm e n t to Lim ita tio n s*
25.Em p l o y a b i l i ty *
COGN ITIV E FU N CTION
26.Pr o b l e m So l v i n g
27.M e m o r y
28.O r i e n ta ti o n *
29.A tte n ti o n *
30.Sa f e ty Ju d g e m e n t*
*FAM items |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
Admt |
Date |
|
D/C |
|
Date |
|
Admt |
Date |
|
D/C |
|
Date |
|||||
RN |
|
|
|
|
|
|
|
ST |
|
|
|
|
|
|
|
|
||
PT |
|
|
|
|
|
|
|
PSY |
|
|
|
|
|
|
|
|
||
OT |
|
|
|
|
|
|
|
REC |
|
|
|
|
|
|
|
|
||
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The FIM Scale is designed to assess an individual's level of functional independence following a brain injury. |
| Scale Levels | The scale consists of 7 levels, ranging from total assist (1) to complete independence (7). |
| Self-Care Items | The FIM Scale includes various self-care items such as feeding, grooming, bathing, and toileting. |
| Mobility Assessment | Mobility items cover transfers between a bed, chair, wheelchair, and toilet, along with locomotion activities. |
| Communication Items | There are communication-related items that evaluate comprehension, expression, reading, writing, and speech intelligibility. |
| Psychosocial Adjustment | The scale assesses social interaction, emotional status, adjustment to limitations, and employability. |
| Cognitive Function | It evaluates cognitive functions, including problem-solving, memory, orientation, attention, and safety judgment. |
| Variability | Responses are recorded based on the level of assistance required, varying from complete independence to total assistance. |
| Governing Laws | The governing laws for state-specific forms may include rehabilitation and healthcare statutes, along with patient privacy regulations. |
Guidelines on Utilizing Fim Scale
Filling out the FIM Scale form is an important step in assessing the functional independence of individuals, particularly after brain injuries. This structured approach allows for a comprehensive evaluation of various tasks and skills. By following the steps below, you can ensure the form is completed accurately and efficiently.
- Start with the patient stamp section at the top of the form. Clearly label the patient's information.
- Begin with the self-care items. For each item listed (feeding, grooming, bathing, dressing upper body, dressing lower body, toileting, swallowing), assess the patient's level of independence and mark it with the corresponding number (1-7).
- For sphincter control, assess and mark both bladder and bowel management using the same independence scale.
- Next, move to the mobility items. Assess the patient’s ability to transfer between surfaces (bed, chair, wheelchair, toilet, tub or shower, and car) and mark the appropriate score.
- Evaluate locomotion by assessing walking/wheelchair use, stair navigation, and community access. Circle the corresponding numbers.
- Then, assess communication. Evaluate comprehension and expression (both verbal and non-verbal), reading, writing, and speech intelligibility. Circle the appropriate scores.
- In the psychosocial adjustment section, assess social interaction, emotional status, adjustment to limitations, and employability. Mark the scores accordingly.
- Finally, evaluate cognitive function by assessing problem-solving, memory, orientation, attention, and safety judgment. Score each appropriately.
- Once all sections are complete, ensure the dates are recorded for admission and discharge, as well as the initials of relevant professionals (RN, ST, PT, PSY, OT, REC) involved in the assessment.
What You Should Know About This Form
What is the FIM Scale form and its purpose?
The FIM Scale form, or Functional Independence Measure, is a standard tool used to assess a patient's level of functional independence in various daily activities following a brain injury. It provides a comprehensive evaluation across multiple domains, including self-care, mobility, communication, psychosocial adjustment, and cognitive function. This assessment helps healthcare professionals create effective rehabilitation plans tailored to each patient's specific needs.
How are patients scored on the FIM Scale?
Patients are scored using a scale that ranges from 1 to 7. A score of 7 indicates complete independence with no assistance required, while a score of 1 reflects total assistance needed from caregivers. Each level assesses the patient's ability to perform specific tasks, such as feeding or dressing, under timely and safe conditions. This scoring system allows for clear communication about a patient's capabilities and progress over time.
What types of activities are evaluated in the FIM Scale?
The FIM Scale evaluates several key areas, including self-care activities like feeding, grooming, and toileting. Mobility tasks such as transfers from bed to wheelchair and walking are also assessed. Additional areas include communication abilities, psychosocial interaction, emotional status, and various cognitive functions like memory and problem-solving. By covering a wide range of activities, the FIM Scale provides a holistic view of a patient's functioning.
How is the FIM Scale used in rehabilitation?
In the rehabilitation process, the FIM Scale informs treatment planning and progress tracking. By assessing a patient's initial functional capabilities, healthcare providers can set relevant goals and select appropriate interventions. Periodic reassessments using the FIM Scale help monitor a patient's improvement, allowing adjustments to the rehabilitation plan as needed. This iterative process promotes patient-centered care and supports optimal recovery paths.
Can FIM Scale results be used for insurance or reporting purposes?
Yes, the results from the FIM Scale can be utilized for insurance purposes and reporting to regulatory bodies. Many insurance providers recognize the FIM Scale as a validated tool for demonstrating the necessity of rehabilitation services. The data collected not only details a patient's level of functioning but also helps justify the care provided, making it useful for billing and compliance requirements.
Who completes the FIM Scale assessment?
The FIM Scale assessment is typically completed by trained healthcare professionals, including nurses, occupational therapists, and physical therapists. These individuals have the expertise necessary to accurately observe and evaluate a patient's performance in various tasks. Their observations, combined with patient input, lead to a reliable assessment that guides the rehabilitation process.
Common mistakes
Individuals often make several common mistakes when completing the FIM Scale form, which can impact the accuracy of the results. One frequent error is inappropriate scoring. For instance, some individuals may not fully understand the criteria for each level of independence. As a result, they might assign a score of 3 or lower when the individual actually performs a greater percentage of the task. This can lead to underreporting the individual's functional capabilities.
Another common mistake is inconsistent terminology. Miscommunication can occur if different staff members use varying terms to describe the same level of assistance. For example, one person might refer to "moderate assist" while another may use "partial assist." This inconsistency can create confusion when evaluating the individual's level of independence.
Many people also overlook the importance of documenting specific situations. The FIM Scale requires specific examples to justify the chosen scores. Without clear documentation, it may be difficult for others to understand the reasons behind the scoring. This oversight can lead to misinterpretation of the individual's abilities.
Another frequent mistake is answering questions based on assumptions. For instance, some respondents may answer based on what they believe the patient's abilities are rather than directly observing their actual performance. This can result in scoring that does not accurately reflect the individual's true level of functional independence.
Failing to consider different environments can also lead to inaccuracies. An individual may perform well in a controlled clinical setting but struggle in a home environment. It's essential to evaluate the individual in various contexts to get a complete picture of their functional abilities.
Many people neglect to consult with other team members. Collaboration among rehabilitation team members is crucial when filling out the FIM Scale form. Each professional may have insights into the patient's abilities that can contribute to a more accurate assessment. Without this input, the document may not fully represent the needs of the individual.
Inadequate training can be another significant factor. Staff members unfamiliar with the scoring system may struggle to accurately assess the individual's performance. This can lead to inconsistencies and potentially skewed results on the FIM Scale form.
Lastly, individuals sometimes rush through the form without thorough consideration. This hasty completion can result in incomplete answers, missing items, or inaccurate scores. Taking the time to carefully assess each item is vital for ensuring the form's effectiveness in assessing functional independence.
Documents used along the form
The Functional Independence Measure (FIM) Scale form is an essential tool in assessing an individual's functional status, especially in relation to brain injuries. It focuses on measuring a person's ability to perform daily activities. Along with the FIM Scale, various other forms and documents assist in comprehensive evaluation and planning for patient care. Below is a list of commonly used documents that complement the FIM Scale.
- Clinical Progress Notes: These notes provide detailed information about a patient's condition, treatment, and response to interventions. Clinicians document daily observations, ensuring a clear record of the patient's journey toward recovery.
- Rehabilitation Goals Plan: This document outlines specific, measurable goals for the patient’s rehabilitation journey. It serves as a roadmap, guiding the treatment process and helping both patients and healthcare providers track progress over time.
- Patient Intake Form: The intake form gathers essential background information about the patient, including medical history, medications, and previous treatments. It helps healthcare professionals understand the patient's overall health status and tailor their care accordingly.
- Discharge Summary: This document is created when a patient is ready to leave a rehabilitation facility. It summarizes the patient’s progress, care provided, and recommendations for ongoing treatment or follow-up care, ensuring continuity in the patient's journey.
- Assessment Tools: Various standardized tools may be used in addition to the FIM Scale to assess specific areas such as communication skills, cognitive function, and emotional status. These tools offer a more comprehensive view of a patient’s abilities and needs.
- Family Education Materials: These resources provide information to family members about the patient's condition, rehabilitation process, and ways to support recovery. They are crucial for involving the family in the care process and equipping them with knowledge for better engagement.
Using the FIM Scale along with these documents ensures a well-rounded approach to patient care. Proper documentation is vital in achieving successful rehabilitation outcomes and maintaining a clear record of the patient’s progress.
Similar forms
The Functional Independence Measure (FIM) Scale is a widely recognized tool used to assess an individual's functional independence. Several other documents and assessment tools serve similar purposes. Below is a list of nine documents comparable to the FIM Scale, along with brief explanations of their similarities:
- Barthel Index - This is a widely used scale that measures performance in activities of daily living (ADLs). Like the FIM, it helps gauge the degree of independence in mobility and personal care.
- Katz Index of Independence in Activities of Daily Living - This tool assesses an individual’s ability to perform basic self-care tasks. Similar to the FIM, it incorporates a scoring system based on independence levels.
- Frenchay Activities Index - Focusing on social and leisure activities, this index evaluates the extent of engagement. Both the Frenchay Activities Index and the FIM Scale aim to provide insights into functional capabilities.
- Activities of Daily Living (ADL) Questionnaire - This questionnaire helps determine an individual’s self-care capabilities. It reflects similar gradations of assistance as found in the FIM Scale.
- Functional Assessment Inventory - This tool assesses a wide range of functional activities, including social and cognitive functions. The FIM Scale and the Functional Assessment Inventory both provide structured ways to identify support needs.
- Mobility Assessment Tool - This tool focuses specifically on mobility issues faced by individuals. Like the FIM, it categorizes levels of assistance required for moving independently and safely.
- Performance Assessment of Self-care Skills (PASS) - This document evaluates self-care tasks in a real-world setting. Both the PASS and FIM Scale help healthcare providers understand a patient’s functional abilities and challenges.
- Mini-Mental State Examination (MMSE) - While primarily a cognitive assessment, the MMSE gives insight into functional capabilities related to cognition. Both tools are often employed together to create a fuller picture of an individual’s independence.
- Reinventing the Wheel (RTW) Assessment - This assessment tool focuses on occupational aspects affecting daily life. Like the FIM, it recognizes that various elements contribute to overall functional independence.
Understanding how these documents relate to the FIM Scale can help professionals better evaluate an individual’s functional capabilities and tailor their support accordingly.
Dos and Don'ts
Filling out the FIM Scale form can seem daunting, but it’s crucial for assessing a patient’s functional independence. Here are important things to keep in mind to ensure accuracy and clarity:
- Do read each item carefully before making a selection. Understanding the requirements will help provide the best possible information.
- Don’t rush through the form. Taking your time prevents errors that could affect patient care.
- Do use precise language and details when describing a patient’s capabilities. Clear descriptions provide valuable context.
- Don’t guess if you’re unsure about a patient’s abilities. It’s better to leave an item blank than to misrepresent their skills.
- Do consult with colleagues or healthcare professionals if you have questions. Collaborative input can improve accuracy.
- Don’t ignore the instructions provided for each section. Each part of the form is tailored to gather specific information that is essential for care planning.
By following these guidelines, the process of completing the FIM Scale form can be both straightforward and effective. Your diligence now will contribute to better patient support and outcomes in the future.
Misconceptions
Misconceptions about the Functional Independence Measure (FIM) Scale can lead to misunderstandings regarding its purpose and usage. Here are six common misconceptions:
- The FIM Scale measures only physical abilities. The FIM Scale evaluates a range of functions, including cognitive, psychosocial, and communication skills. It provides a comprehensive view of a patient's overall independence.
- People with severe disabilities cannot score above a certain level. Even individuals with significant challenges in daily activities can demonstrate modified independence or receive assistance in certain tasks, thereby scoring above the lowest level.
- The FIM Scale is only for use with brain injury patients. While it is commonly used for assessing brain injury recovery, the FIM Scale can apply to anyone needing assistance due to various medical conditions, including strokes and neurological disorders.
- A higher score on the FIM Scale guarantees complete recovery. A higher score indicates greater independence, but it does not necessarily mean that the individual has fully recovered. Many factors influence overall recovery, including the nature of the injury and additional support needed.
- Scoring on the FIM Scale is subjective and unreliable. The FIM Scale incorporates standardized guidelines and trained assessors to ensure accurate and consistent scoring. While some subjectivity exists, it is minimized through these established procedures.
- Once assessed, a patient's score remains constant. The FIM Scale is designed for periodic re-assessment. A patient's condition may improve or decline over time, necessitating updates to their score to reflect current abilities accurately.
Understanding these misconceptions can help clarify the significance of the FIM Scale and its role in patient care and rehabilitation.
Key takeaways
The Functional Independence Measure (FIM) Scale form is a key tool for assessing a patient’s ability to perform daily activities after a brain injury. Here are seven essential takeaways about using this form:
- Understand the Scale: The FIM Scale measures a patient's level of independence from 1 to 7, where 1 indicates total assistance and 7 indicates complete independence.
- Focus on Specific Tasks: The form includes various self-care items such as feeding, grooming, bathing, and toileting that are critical for daily living.
- Mobility Assessment: Mobility items assess different types of transfers and locomotion, allowing for a comprehensive view of a patient’s physical capabilities.
- Communication Factors: The communication section evaluates comprehension and expression, essential for overall functional independence.
- Psycho-Social and Cognitive Evaluations: Items related to emotional status, social interaction, problem-solving, and safety judgment are included to address the psychological and cognitive aspects of recovery.
- Accurate Scoring: Each task should be scored based on the level of assistance the patient requires, which directly influences their treatment plan.
- Document Thoroughly: Ensure all relevant dates and professional assessments (e.g., nursing, speech therapy) are documented to track patient progress over time.
Browse Other Templates
Firearm Registration Application,NFA Firearm Manufacturing Application,Application for Firearm Creation,NFA Firearm Registration Request,Form for Firearm Production and Registration,Firearm Maker's Application Form,Application to Construct a Firearm, - It must be filed in duplicate without staples.
How to Write a Treatment Plan - Each Treatment Planner is continuously updated based on the latest research in the field of psychotherapy.
It Support Ventura - Your date of birth is necessary for processing your request.