Fill Out Your Fl Provider Application Form
The Florida Medicaid Provider Enrollment Application is an essential tool designed for healthcare providers seeking participation in Medicaid programs. This comprehensive form encapsulates various crucial aspects that ensure providers meet the necessary enrollment criteria. It outlines general information about enrollment qualifications, accuracy of information, and requirements for supporting documentation. The application process is clearly delineated, allowing potential providers to navigate the intricate landscape of Medicaid enrollment more efficiently. Key sections include identification requirements, certification and attestation panels, and detailed stipulations regarding service locations and billing agreements. Additionally, the form addresses critical considerations such as the use of Social Security numbers and the importance of maintaining accurate provider information. Applicants are equipped with helpful resources and application status descriptions, enhancing their understanding of the process from initial submission to confirming enrollment status. This guide aims to streamline the provider enrollment experience, ensuring compliance and facilitating access to Medicaid reimbursement for eligible healthcare services.
Fl Provider Application Example
Florida Medicaid Provider Enrollment
Application Guide
Version 2.0 | April 2021

Florida Medicaid Provider Enrollment Application Guide – Version 2.0 – April 2021
Table of Contents
1 |
Purpose |
1 |
|
2 |
Contents |
1 |
|
|
2.1 |
General Information |
1 |
|
2.2 |
Enrollment Qualifications |
1 |
|
2.3 |
Accuracy of Information |
2 |
|
2.4 |
Notice Regarding Use of Social Security Number |
2 |
|
2.5 |
Supporting Documentation Requirements |
2 |
|
2.6 |
Enrollment Process |
2 |
3 |
Before You Enroll |
2 |
|
4 Submitting a Provider Enrollment Application |
3 |
||
|
4.1 |
Navigation |
3 |
|
4.2 |
Welcome Statement |
3 |
|
4.3 |
Enrollment Type |
3 |
|
4.4 |
Enrollment Type Confirmation |
4 |
|
4.5 |
Application Tips |
4 |
|
4.6 |
Request Type |
5 |
|
4.7 |
Before You Continue |
6 |
|
4.8 |
Identifying Information |
6 |
|
4.9 |
Certification and Attestation Panel |
7 |
|
4.10 |
License & More Identifying Information |
7 |
|
4.11 |
Collaboration Agreement |
8 |
|
4.12 |
Contact Information |
8 |
|
4.13 |
Service Location |
8 |
|
4.14 |
Mailing Address |
9 |
|
4.15 |
Pay To Address |
9 |
|
4.16 |
Home/Corp Office Address |
9 |
|
4.17 |
Xref NPI |
10 |
|
4.18 |
ATN Information |
10 |
|
4.19 |
Member of the Following Groups |
11 |
|
4.20 |
Billing Agent Agreement |
11 |
|
4.21 |
Owners and Operators |
12 |
|
4.22 |
EFT Agreement |
13 |
|
4.23 |
Applicant History |
14 |
|
4.24 |
Supporting Documents |
15 |
|
4.25 |
Certification |
15 |
|
4.26 |
Application Confirmation |
16 |
|
4.27 |
Verifying the Status of an Enrollment Application |
16 |
ii
Copyright © 2021. All rights reserved.

Florida Medicaid Provider Enrollment Application Guide – Version 2.0 – April 2021
4.28 |
Application Status Descriptions |
17 |
4.29 |
Submitting Corrections to a Pending Application |
19 |
4.30 |
Maintaining Provider Information |
20 |
4.31 |
Helpful Resources |
20 |
iii
Copyright © 2021. All rights reserved.

Florida Medicaid Provider Enrollment Application Guide – Version 2.0 – April 2021
This page intentionally left blank.
iv
Copyright © 2021. All rights reserved.
Florida Medicaid Provider Enrollment Application Guide – Version 2.0 – April 2021
1 Purpose
The Agency for Health Care Administration (Agency) and its fiscal agent, Gainwell Technologies (Gainwell), have created this comprehensive reference guide to assist applicants with completing the enrollment process using the Florida Medicaid online enrollment wizard. This guide references and ties together provider
2 Contents
General Information
Enrollment Qualifications
Accuracy of Information
Notice Regarding Use of Social Security
Number
Supporting Documentation Requirements
Enrollment Process
Before You Enroll
Submitting a Provider Enrollment Application
Welcome Statement
Enrollment Type
Enrollment Type Confirmation
Application Tips
Request Type
Before You Continue
Identifying Information
Certification and Attestation Panel
License & More Identifying Information
Collaboration Agreement
Contact Information
Service Location
Mailing Address
Pay To Address
Home / Corp Office Address
Xref NPI
ATN Information (ATN is generated at this time)
Member of the Following Groups Billing Agent Agreement Owners and Operators
EFT Agreement
Applicant History Supporting Documents Certification Application Confirmation
Verifying the Status of an Enrollment Application
Application Status Descriptions
Submitting Corrections to a Pending Application
Maintaining Provider Information Helpful Resources
2.1General Information
In order to receive Medicaid reimbursement, a provider must be enrolled in Medicaid and meet all provider requirements at the time the service is rendered. Every entity that provides Medicaid services to recipients and all
2.2Enrollment Qualifications
Providers must meet all provider requirements and qualifications. Practices must be fully operational before they can be enrolled as Medicaid providers. General enrollment requirements are covered in the Medicaid Provider General Handbook. Program specific qualifications for each provider type are listed in the Coverage and Limitations Handbooks. All handbooks are available at https://ahca.myflorida.com/.
1
Copyright © 2021. All rights reserved.
Florida Medicaid Provider Enrollment Application Guide – Version 2.0 – April 2021
2.3Accuracy of Information
All enrollment statements or documents submitted to the Agency for Health Care Administration (Agency) or the Medicaid fiscal agent must be true and accurate. Filing of false information is sufficient cause for denial of an enrollment application or termination from Medicaid participation.
2.4Notice Regarding Use of Social Security Number
As a part of your application for enrollment as a Florida Medicaid provider, all individuals listed as Owner(s) and Operator(s) are required to provide their social security number (SSN) to the Agency pursuant to 26 U.S.C. 6109. Disclosure of your social security number is mandatory. Failure to provide your social security number will be a basis to refuse to enroll you as a Medicaid provider.
Your social security number will be used to secure the proper identification of persons for whom the Agency is responsible for making a return, statement, or other document in accordance with the Internal Revenue Code, and to assist in the administration of the Florida Medicaid program.
2.5Supporting Documentation Requirements
The application process cannot be completed until all required documents as stipulated in the applicable Handbook sections, including an accurately completed Florida Medicaid provider agreement and background screening, are received.
Applicants must include the Application Tracking Number (ATN) provided by the Online Enrollment Wizard when uploading supporting documents.
Please visit the Enrollment Forms page via
2.6Enrollment Process
Most provider enrollment applications will go through the following process:
1.Applicant submits an Enrollment Application via the Florida Medicaid Web Portal Online Enrollment Wizard.
2.The Enrollment Application is evaluated based on the enrollment rules. The Agency completes the credential verification process and site visit, when applicable.
3.The Enrollment Application is finalized. Provider receives a letter containing the final status, whether approved or denied.
4.Once the Enrollment status is Active, the provider receives a Welcome Letter, and Florida Medicaid ID. Full and limited enrolled providers will also receive a PIN Letter, that will be used to create a secure web portal account.
3 Before You Enroll
Before initiating the enrollment process, please follow the instructions listed below:
1.Review the Provider General Handbook, Chapter 2, for general enrollment requirements. The handbook is located on the Agency’s website at http://ahca.myflorida.com.
2.Determine which Enrollment Type will be used.
3.Determine which Provider Type and Specialty will be used. View the Provider Type and Specialty to learn which qualifies for fully enrolled, limited enrolled, or order or referring enrollment.
4.Refer to the Interactive Enrollment Checklist to identify enrollment application requirements based on enrollment type, application type, provider type, and specialty, prior to starting the application process. To access the Interactive Enrollment Checklist, visit mymedicaid- florida.com. From the homepage, hover over the Provider Services tab, and click Enrollment. Once at the Provider Enrollment page, look under the New Medicaid Providers section, and click Interactive Enrollment Checklist.
5.Before the application can be submitted, all supporting documentation must be uploaded.
2
Copyright © 2021. All rights reserved.
Florida Medicaid Provider Enrollment Application Guide – Version 2.0 – April 2021
4 Submitting a Provider Enrollment Application
The Florida Medicaid Provider Enrollment Application gathers information related to the applicant’s eligibility to enroll in Florida Medicaid. Providers use this page to complete an enrollment application to become a participating provider in the Florida Medicaid program.
The following provides guidance for accurately reporting the elements of the application. By logging into the secure Web Portal at
The online enrollment application cannot be used if applying for Out of State Enrollment or Additional Location Codes.
4.1Navigation
|
Button |
|
|
Description |
|
|
|
|
|
||
|
New application |
|
Click to create a new application. |
||
|
|
|
|
||
|
Continue application |
|
Click to continue an application that was previously saved and |
||
|
|
|
|
assigned an ATN (Application Tracking Number). |
|
|
Save and continue |
|
Click to save changes made to the current panel and proceed to the |
||
|
|
|
|
next. |
|
|
|
|
|
Note: Enrollment information is only temporarily stored in the |
|
|
|
|
|
Enrollment Wizard until you have reached the stage where an ATN |
|
|
|
|
|
has been created. |
|
|
Previous |
|
Click to return to the previous panel. |
||
|
|
|
|
||
|
Exit |
|
Click to exit from the Online Enrollment Wizard. |
||
? |
|
|
Click to access contextual page help. |
||
|
Delete |
|
Click to delete the selected row. |
||
|
|
|
|
||
|
Refresh session |
|
Click to extend the Online Enrollment Wizard session expiration |
||
|
|
|
|
time. |
|
|
|
|
|
Note: By default, the session will expire after 60 minutes. All |
|
|
|
|
|
unsaved information will be lost. |
|
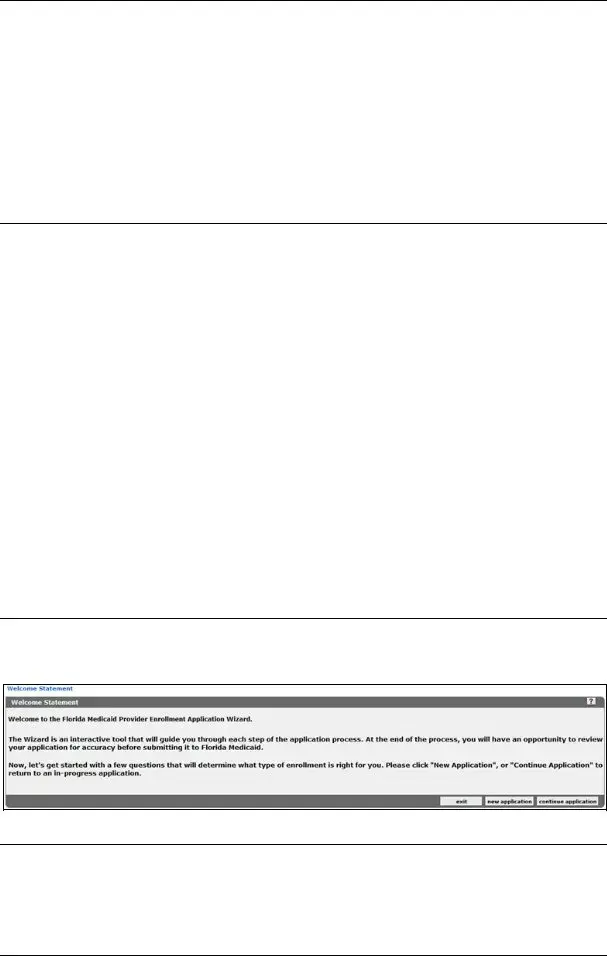
4.2Welcome Statement
Upon launching the Florida Medicaid Enrollment Application Wizard, applicants will be greeted with a Welcome Statement panel, and will have the option to create a new application or access on that was previously started.
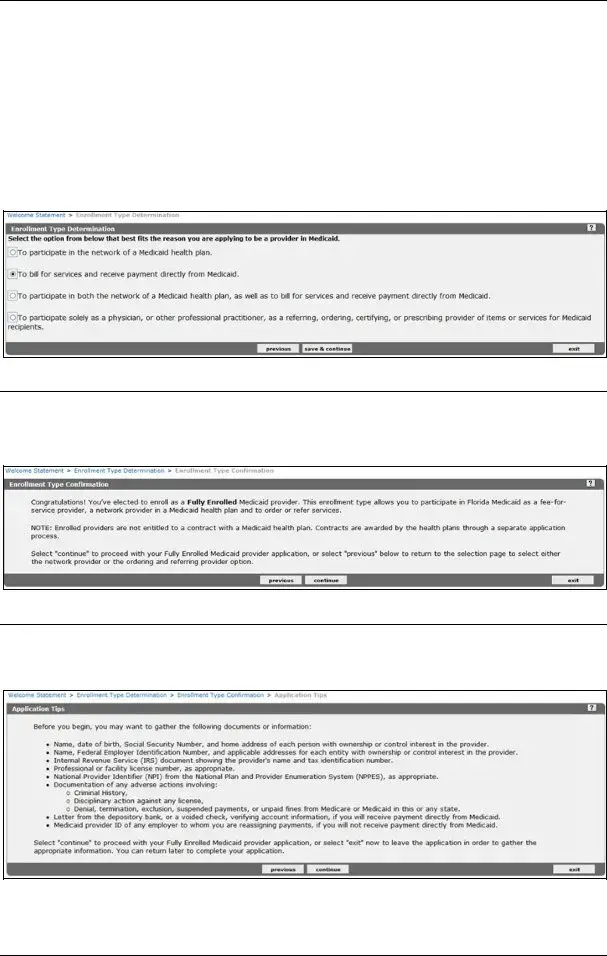
4.3Enrollment Type
The Enrollment Type Determination panel will ask the applicant to choose the option that most accurately describes the reason they are applying to be a Medicaid provider. The selection made on this panel will determine all of the steps that will follow in the application.
Provider must enroll as one of the following:
3
Copyright © 2021. All rights reserved.
Florida Medicaid Provider Enrollment Application Guide – Version 2.0 – April 2021
Fully Enrolled allows providers to:
•Bill for services and receive payment directly from Medicaid.
•Participate in both the network of a Medicaid health plan as well as to bill for services and receive payment directly from Medicaid.
Limited Enrolled allows providers to:
•Participate in the network of a Medicaid health plan.
Ordering or Referring will allow providers to:
•Participate solely as a physician, or other professional practitioner, as a referring, ordering, certifying, or prescribing provider of items or services for Medicaid recipients.
4.4Enrollment Type Confirmation
After selecting the desired enrollment type determination response, providers will reach the Enrollment Type Confirmation panel that will confirm the selection made on the previous screen.
If a choice was made incorrectly, providers can click previous or if correct, click continue.
4.5Application Tips
Providers are encouraged to obtain all necessary documents or information, before proceeding with the application. The Application Tips panel lists details that may be necessary to complete application processing.
4
Copyright © 2021. All rights reserved.
Florida Medicaid Provider Enrollment Application Guide – Version 2.0 – April 2021
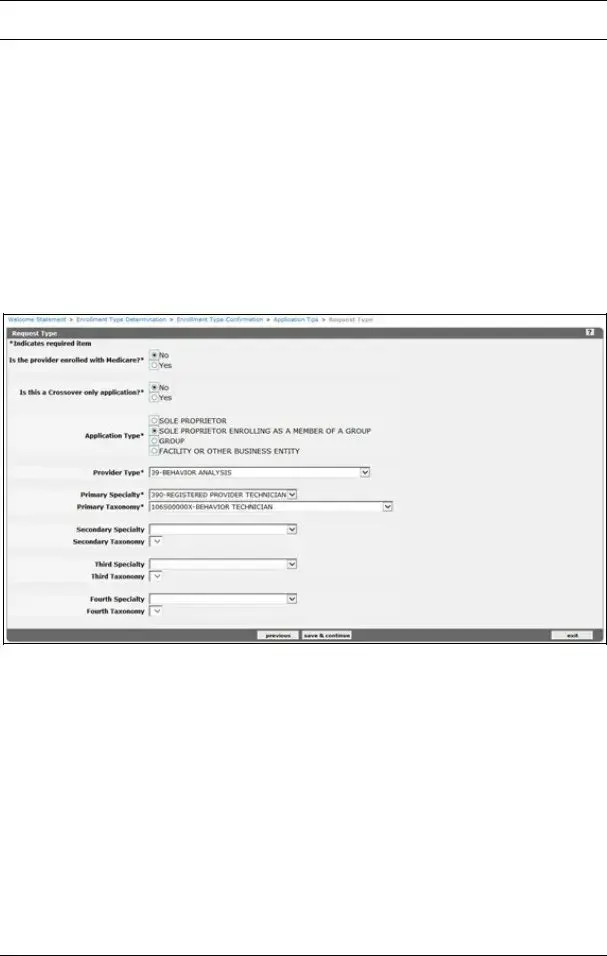
4.6Request Type
The information presented in the Request Type panel results may vary. The information displayed is contingent on the enrollment type selected in the previous panel. Applicants will only be presented with provider type and specialty selections that are available for the enrollment type selected, as well as taxonomies that align to the specialties chosen. Applicants may view the Provider Type and Specialty crosswalk to learn which qualifies for fully enrolled, limited enrolled, or ordering or referring enrollment.
Applicants must also select an Application Type within the panel.
A Sole Proprietor is an individual who plans to bill Medicaid directly. This option should be selected if you are individual that plans to submit claims to Medicaid and receive payments directly.
A Sole Proprietor Enrolling as a Member of a Group is an individual who plans to bill solely through a group membership and will not submit claims or receive payment directly from Medicaid.
Group should be selected if there is more than one member.
A Facility or Other Business Entity should be selected if the applicant is an entity that is formed and administered in accordance with commercial laws in order to engage in business activities
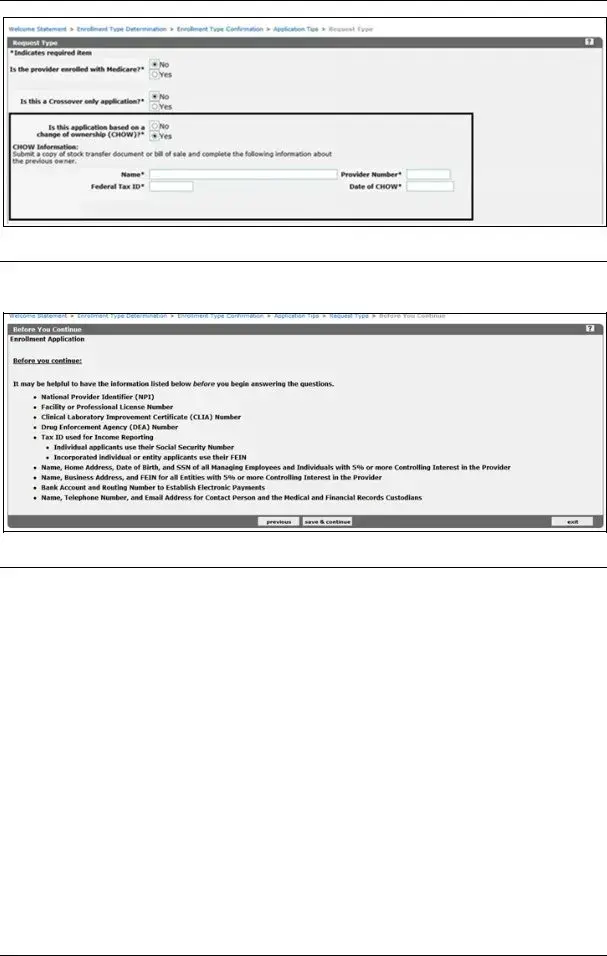
4.6.1 Change of Ownership Application
If the applicant is seeking to submit a CHOW application, they can visit the CHOW page on the public Web Portal for more information.
If the application is based on a change of ownership (CHOW) providers applying for full enrollment should select Yes to the CHOW question and enter the previous owner’s information such as the Name, Provider Number, Federal Tax ID, and Date of CHOW into the required fields. They must also upload the supporting documentation for the CHOW.
Note: Once an application is submitted, the CHOW response cannot be changed and a new application will be required if updates are needed.
5
Copyright © 2021. All rights reserved.
Florida Medicaid Provider Enrollment Application Guide – Version 2.0 – April 2021
4.7Before You Continue
Providers should obtain the information below before proceeding with the remainder of the application.
4.8Identifying Information
4.8.1 Provider Name
This is the legal name by which you are known to the Internal Revenue Service. Enter the name of the entity or the last name, first name, and middle initial of an individual. The name must also match the name listed on the provider’s license.
4.8.2 Doing Business As (D/B/A)
This is for individual or entity applicants doing business under a trade or company name. Individual providers doing business under his/her own name should leave this section blank.
4.8.3 Tax Identification Number (TIN)
•Social Security Number (SSN) - Individual providers who are not personally incorporated will enter their SSN and supply a copy of their Social Security card.
Note: Individual providers may not use their employer’s Tax ID on their individual provider file.
•Federal Employer Identification Number (FEIN) - Enter your FEIN if you are an entity or are individually incorporated. Attach a legible copy of proof of Tax ID such as an IRS Form
6
Copyright © 2021. All rights reserved.
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | This guide assists applicants in completing the Florida Medicaid Provider Enrollment process. |
| Governing Bodies | Managed by the Agency for Health Care Administration and Gainwell Technologies. |
| Enrollment Requirement | Providers must be enrolled in Medicaid to receive reimbursement for services rendered. |
| General Requirements | Providers must meet qualifications and be fully operational prior to enrollment. |
| Supporting Documentation | Applicants must provide necessary supporting documents along with their application. |
| Application Submission | Applications can be submitted online via the Florida Medicaid Web Portal. |
| Status Verification | Applicants can verify the status of their enrollment application through the online portal. |
Guidelines on Utilizing Fl Provider Application
Once you have gathered the necessary information and documentation, you are ready to fill out the Florida Provider Application form. This application process is essential for those wishing to engage with the Florida Medicaid program. The following steps will guide you through completing the form efficiently.
- Access the Florida Medicaid Web Portal at www.mymedicaid-florida.com.
- Locate the Provider Enrollment Application section within the portal.
- Begin by reading the Welcome Statement provided on the application.
- Select your Enrollment Type based on the services you intend to provide.
- Confirm your selected Enrollment Type when prompted.
- Review Application Tips that may help you during the process.
- Choose the Request Type that corresponds to your situation.
- Proceed only after confirming you meet the prerequisites listed on the “Before You Continue” page.
- Enter your Identifying Information accurately, including your name and address details.
- Complete the Certification and Attestation Panel, confirming the provided information is correct.
- Input any necessary License & More Identifying Information as required.
- Attach any Collaboration Agreements if applicable.
- Fill out your Contact Information for follow-ups.
- Detail the Service Location where services will be rendered.
- Provide your Mailing Address, ensuring accuracy for correspondence.
- Submit your Pay To Address, where payments should be directed.
- Input your Home/Corp Office Address and any relevant details.
- Include your Xref NPI if you have one.
- Fill out the ATN Information; this will be generated automatically.
- Indicate if you are a Member of the Following Groups, if applicable.
- If you’re using a Billing Agent, provide details regarding the Billing Agent Agreement.
- List any Owners and Operators associated with your practice.
- Complete the EFT Agreement for electronic payments.
- Outline your Applicant History as required.
- Upload any Supporting Documents that are necessary for your application.
- Review and complete the Certification section to affirm all information is true.
- Submit the Application Confirmation when ready, ensuring all provided information is completed.
- Finally, monitor your application by Verifying the Status of your Enrollment Application regularly.
What You Should Know About This Form
What is the purpose of the Florida Medicaid Provider Enrollment Application?
The Florida Medicaid Provider Enrollment Application serves as a formal procedure for healthcare providers seeking to receive reimbursement for services provided under Medicaid. It outlines the necessary steps to enroll, ensuring that all regulations and requirements are met before a provider can bill Medicaid for their services. This process guarantees that enrolled providers have received the appropriate training and qualifications, enabling them to provide safe and effective care to Medicaid recipients.
What are the enrollment qualifications for providers?
To enroll as a Medicaid provider, certain qualifications must be fulfilled. Providers must be fully operational, which means they should have all necessary licenses and certifications that pertain to their specific field. Each provider type may have distinct qualifications detailed in the Coverage and Limitations Handbooks. It is crucial to review these documents to ensure compliance with all state requirements before applying, as non-compliance can delay or prevent enrollment.
How can I verify the status of my enrollment application?
Once you submit your application, it’s important to keep track of its status. You can verify your application's status through the Florida Medicaid Web Portal. Simply log in using your credentials and navigate to the appropriate section for application status inquiries. This feature allows providers to remain informed throughout the review process, ensuring that any issues can be addressed promptly.
What supporting documentation is required when submitting the application?
Supporting documentation is critical for ensuring your application is processed smoothly. Requirements may include proof of licensure, collaboration agreements, and any additional certifications specific to your practice. Be sure to check the guidelines provided in the Medicaid Provider Enrollment Application Guide for a comprehensive list of needed documents. Submitting complete and accurate documentation helps avoid delays in your application review.
Common mistakes
Filling out the Florida Provider Application form can be a daunting task. Many applicants make mistakes that can delay their enrollment. Understanding these common errors can help streamline the process.
One major mistake involves incomplete sections. Some applicants fail to fill out every required field, believing that optional information is sufficient. This can lead to the application being returned or denied, as missing data can trigger questions about eligibility.
Another frequent error is providing inaccurate information. This includes misspellings, incorrect social security numbers, or outdated contact details. Accuracy is essential, as discrepancies may raise flags that complicate the review process.
Additionally, many do not carefully review the supporting documentation requirements. Each application must be accompanied by specific documents such as licenses and proof of qualifications. Failing to include these items can result in immediate rejection, requiring the applicant to restart the process.
The application process may also be hindered when people overlook the importance of the certification and attestation panel. Applicants sometimes neglect to sign or incorrectly complete this panel, which is crucial to affirm that the information provided is truthful and complete.
Moreover, failure to confirm one's enrollment type can lead to complications. Applicants should be clear on whether they are applying as an individual provider or as part of an organization. Mixing these categories can create confusion and lead to substantial delays.
Finally, not double-checking contact information can prevent communications from reaching the applicant. If the Medicaid office cannot reach the provider due to incorrect contact details, critical updates regarding the application status may be missed.
By being aware of these common mistakes, applicants can improve their chances of successful enrollment and avoid unnecessary setbacks in the application process.
Documents used along the form
When applying for Medicaid enrollment in Florida, several key forms and documents are required alongside the Florida Medicaid Provider Application form. Each of these documents serves a specific purpose in ensuring a complete application package. Make sure to gather and prepare these documents promptly to avoid delays in your enrollment process.
- Supporting Documentation Requirements: This document outlines all necessary supporting documents that must be submitted with your application. It provides clarity on the types of documentation required to prove your credentials and operational status as a Medicaid provider.
- Collaboration Agreement: If you will be working with other medical practitioners or organizations, this agreement details the collaborative arrangements. It’s essential for demonstrating how services will be coordinated among providers.
- Billing Agent Agreement: This form is necessary if a billing agent will be submitting claims on your behalf. It clarifies the relationship between the provider and the billing agent, ensuring transparency and compliance with Medicaid regulations.
- EFT Agreement: The Electronic Funds Transfer (EFT) agreement allows for direct deposit of Medicaid payments into your bank account. Completing this form is crucial for ensuring timely and secure payment for services rendered.
- Applicant History: This document requires information about your professional history and any prior participation in Medicaid programs. It helps the reviewing agency assess your eligibility and compliance with Medicaid requirements.
- Certification and Attestation Panel: This section of the application requires your affirmation that the information provided is accurate and that you meet all Medicaid eligibility criteria. It serves as a formal declaration of compliance.
As you prepare your application for Medicaid enrollment, please ensure that all forms, including the additional documents listed, are completed accurately. Timeliness and attention to detail will help facilitate a smooth enrollment process.
Similar forms
-
Medicare Provider Enrollment Application: Similar to the Florida Medicaid Provider Application, this document outlines the qualifications and processes for healthcare providers to enroll in the Medicare program, including required documentation and steps for application submission.
-
State Medicaid Provider Enrollment Form: Many states have their own forms for enrolling in Medicaid programs, similar in structure and purpose to Florida's form, detailing eligibility, necessary information, and verification processes.
-
Insurance Credentialing Application: This application is used by providers to obtain credentials with insurance companies. It requires similar identifying information and supporting documentation as the Florida Medicaid application.
-
National Provider Identifier (NPI) Application: Used to apply for a unique identification number required for healthcare providers, this application shares information requirements like personal details and practice location.
-
Clinical Laboratory Improvement Amendments (CLIA) Application: Providers seeking to operate a laboratory must complete this application, which similarly requires documentation demonstrating compliance with federal regulations and operational standards.
-
Telehealth Provider Registration Form: This form is required for healthcare providers offering telehealth services, incorporating similar qualifications and identification processes as the Medicaid provider application.
-
Substance Abuse and Mental Health Services Administration (SAMHSA) Provider Application: This application is required for providers seeking to serve patients with substance use disorders, characterized by similar enrollment criteria and documentation requirements.
-
Emergency Medical Services (EMS) Provider Application: This form outlines the requirements for providers looking to offer EMS services, mirroring the basic enrollment and qualification processes found in the Florida Medicaid application.
-
Home and Community-Based Services (HCBS) Provider Application: This document is designed for providers delivering services in home and community settings, sharing fundamental information-gathering and qualification components with the Medicaid application.
-
Managed Care Organization (MCO) Contract Application: Providers wishing to contract with MCOs must complete this application, which, like the Medicaid provider application, includes detailed disclosures about the provider's qualifications, history, and operational practices.
Dos and Don'ts
Completing the Florida Provider Application form requires careful attention to detail. Here are four important do's and don'ts to keep in mind.
- Do verify that all personal and business information is accurate before submission.
- Do ensure that your practice is fully operational and meets all Medicaid provider qualifications.
- Don't leave any sections blank; fill out every required field completely.
- Don't use outdated forms; always refer to the latest version of the application guide for updates.
Misconceptions
Misconceptions about the Florida Provider Application form can lead to confusion and delays in the enrollment process. Here are nine common misunderstandings:
- Anyone can apply without qualifications. Some believe that anyone can enroll as a Medicaid provider. In reality, providers must meet specific requirements and qualifications before they can apply.
- All information can be estimated. Many think it's acceptable to provide estimated information on the application. However, the application requires accurate details, and any inaccuracies can result in rejection.
- Social Security Numbers are optional. Some applicants are under the impression that providing a Social Security Number is optional. This is incorrect; it is a requirement for verification purposes.
- Supporting documents are not necessary. There is a belief that one can submit an application without accompanying documents. Supporting documentation is crucial for approval and must be included.
- Enrollment can happen after services are rendered. Some providers think they can enroll after providing services. Enrollment must occur before any services are rendered to receive Medicaid reimbursement.
- Submit one application for all services. There's a misconception that a single application covers all types of service. Each provider type may require a separate application based on specific qualifications.
- Corrections can be made easily after submission. Some applicants think they can make corrections effortlessly post-submission. While it is possible to submit corrections, it may complicate the review process.
- Online resources are not important. Many underestimate the value of online resources. These resources provide essential guidance and can help avoid mistakes during the application process.
- Application status updates are instant. A common myth is that applicants will receive immediate updates on their application status. In reality, it can take time for the review process to be completed.
Understanding these misconceptions can facilitate a smoother enrollment process for Florida Medicaid providers.
Key takeaways
Here are some key takeaways about filling out and using the Florida Provider Application form:
- Complete Enrollment: To get reimbursed by Medicaid, you must be enrolled as a provider and meet all requirements at the time services are provided.
- Gather Documentation: Ensure you have all necessary supporting documents before starting the application process. This will help avoid delays.
- Follow Instructions: Carefully read each section of the application guide. This will ensure you complete the form accurately and efficiently.
- Check Your Information: Double-check all entries. Any inaccuracies could lead to a rejection or delay in processing your application.
- Verification: After submission, you can verify the status of your application online. Stay proactive to ensure timely processing.
Browse Other Templates
Csd-1 Certification - This form is intended for manufacturers and installing contractors to provide safety device information.
Va Form 4659 - It highlights an instance of potential corruption that merits further scrutiny.