Fill Out Your 3643 Form
The 3643 form, utilized by the Texas Department of Aging and Disability Services, serves as a crucial component for documenting and managing restorative care plans for individuals receiving therapy services. This form encompasses multiple sections that outline a resident's personalized plan of care, detailing goals and approaches to be undertaken throughout the therapy. The document captures important dates when restorative programs are initiated, alongside a record of signatures from licensed nursing and therapy staff, affirming accountability and collaboration in patient care. Furthermore, the form includes sections for monitoring the resident's responses and progress toward the established goals over a five-week period. Adjustments to the care plan can be made based on weekly assessments, ensuring the program remains tailored to the resident's evolving needs. Monthly reviews prompt staff to evaluate the appropriateness of the plan and recommend any necessary modifications. Comments can be added to provide additional context or insights. The comprehensive design of the 3643 form promotes effective communication among care team members while maintaining a focus on enhancing patient outcomes.
3643 Example
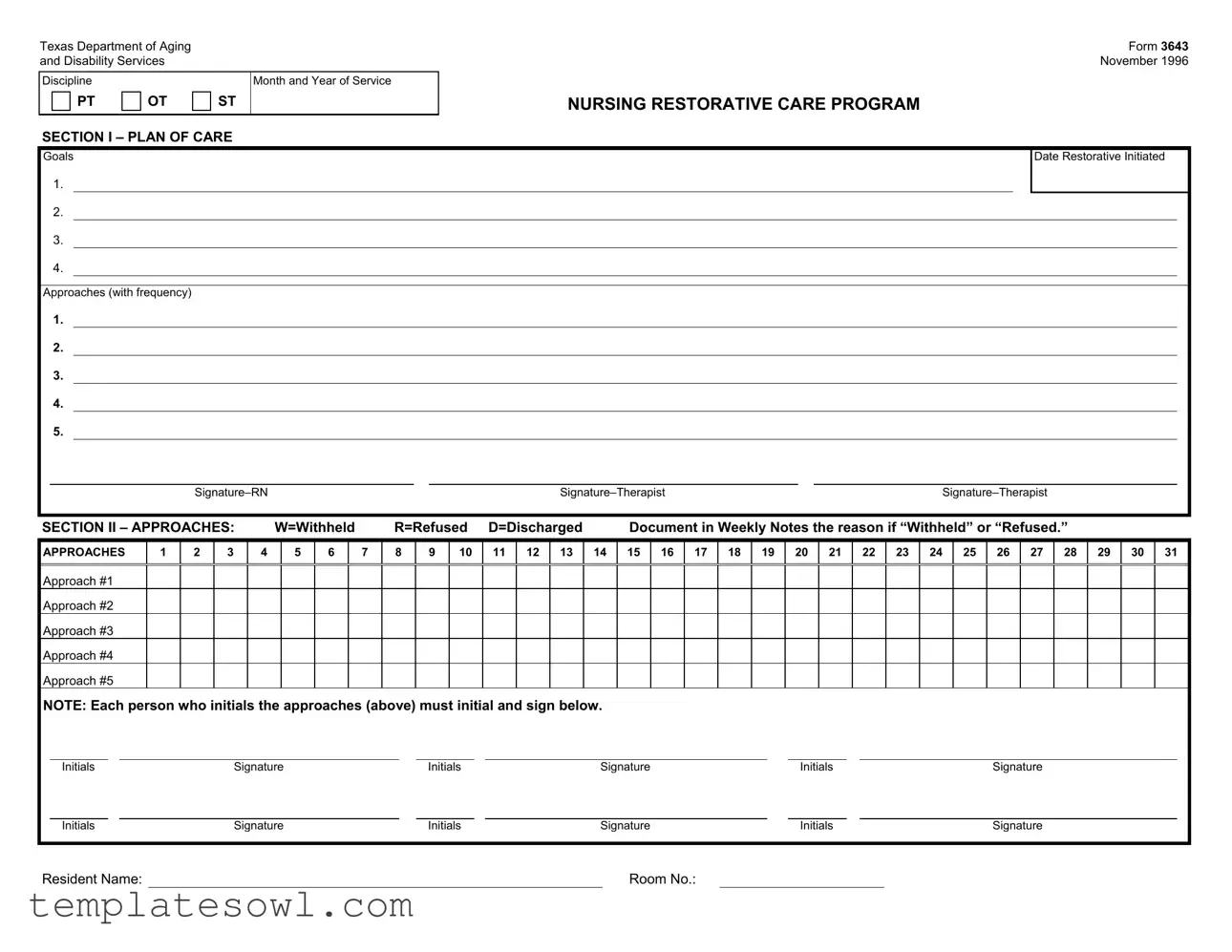
Texas Department of Aging
and Disability Services
Discipline |
|
|
Month and Year of Service |
PT |
OT |
ST |
|
|
|
|
|
SECTION I – PLAN OF CARE
Form 3643
November 1996
NURSING RESTORATIVE CARE PROGRAM
Goals
1.
2.
3.
4.
Approaches (with frequency)
Date Restorative Initiated
1.
2.
3.
4.
5.
|
||||
|
|
|
|
|
SECTION II – APPROACHES: |
W=Withheld |
R=Refused D=Discharged |
Document in Weekly Notes the reason if “Withheld” or “Refused.” |
|
APPROACHES
1
2
3
4
5
6
7
8
9
10 |
11 |
12 |
13 |
14 |
15 |
16 |
17 |
18 |
19 |
20 |
21 |
22 |
23 |
24 |
25 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
26 27 28 29 30 31
Approach #1
Approach #2
Approach #3
Approach #4
Approach #5
NOTE: Each person who initials the approaches (above) must initial and sign below.
Initials |
|
Signature |
|
Initials |
|
Signature |
|
Initials |
|
Signature |
|
|
|
|
|
|
|
|
|
|
|
Initials |
|
Signature |
|
Initials |
|
Signature |
|
Initials |
|
Signature |
Resident Name: |
|
Room No.: |
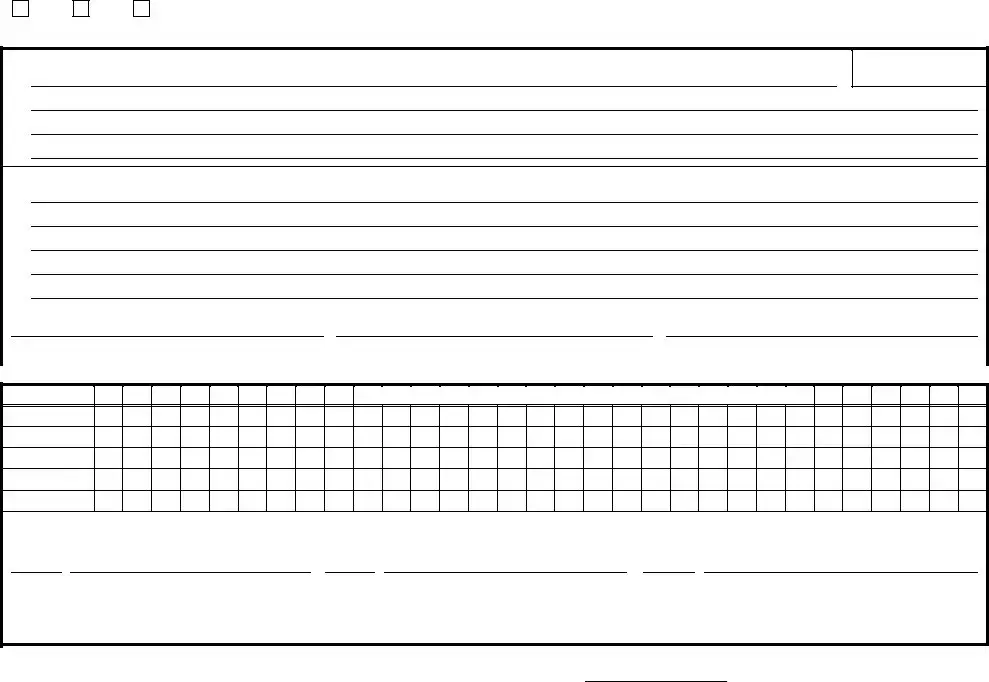
Form 3643
Page 2
SECTION III – DOCUMENT RESIDENT’S RESPONSE AND PROGRESS TOWARD GOALS(S):
Week 1 – Response
|
|
|
|
|
|
|
|
|
|
Signature |
|
|
|
Date |
|||||
Week 2 – Response |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Signature |
|
|
|
Date |
|||||
Week 3 – Response |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Signature |
|
|
|
Date |
|||||
Week 4 – Response |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Signature |
|
|
|
Date |
|||||
Week 5 – Response |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Signature |
|
|
|
Date |
|||||
SECTION IV – MONTHLY REVIEW |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
A. Is the Plan of Care appropriate? |
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
No |
||||
|
B. Are changes to the Restorative Program recommended? |
|
|
|
|
|
|
|
Yes |
No |
|||||||||
|
Are changes recommended to the Goals? |
|
|
|
|
|
|
|
|
|
|
Yes |
No |
||||||
|
Are changes recommended to the Approaches? |
|
|
|
|
|
|
|
|
|
Yes |
No |
|||||||
|
If YES to any items in B, update next month’s SECTION |
|
|
|
|
|
|
||||||||||||
|
Comments: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
C. Continue Program? |
|
|
Yes |
No |
D. Discharge to basic nursing? |
|
|
|
|
Yes |
No |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Date |
||||||
Form Characteristics
| Fact Name | Description |
|---|---|
| Document Purpose | The Form 3643 is used by the Texas Department of Aging and Disability Services to assess and document the plan of care for individuals receiving restorative services. |
| Governing Law | This form is governed by the Texas Health and Safety Code, Subchapter B, which pertains to long-term care services. |
| Service Types | The form specifically covers various types of therapy including physical therapy (PT), occupational therapy (OT), and speech therapy (ST). |
| Goals Section | Providers must set and document specific goals, allowing for tailored care plans that meet individual needs. |
| Approaches Documentation | Approaches to therapy must be recorded along with their frequencies, enabling ongoing assessment of their effectiveness. |
| Weekly Monitoring | The form requires weekly documentation of the resident’s response, ensuring consistent progress monitoring. |
| Monthly Review | A comprehensive monthly review is critical, assessing whether the care plan remains appropriate and if modifications are needed. |
| Signatures Required | Signatures from licensed staff and therapists are necessary to validate the approaches taken and the plan of care. |
| Discharge Options | The form includes sections to evaluate whether to continue or discontinue the restorative program, based on the resident’s progress. |
Guidelines on Utilizing 3643
Filling out the 3643 form is an important task that helps document the plan of care and progress for patients in restorative care programs. Completing this form accurately ensures that all relevant information is captured for ongoing assessments and adjustments. Below are the steps to guide you through the process of filling out the form.
- Step 1: Begin with Section I, where you will enter the patient's name and room number at the top of the form.
- Step 2: List the goals for the patient in the designated space (Goals 1-4).
- Step 3: Specify the approaches along with their frequency in the corresponding spaces provided (1-5).
- Step 4: Indicate the date each restorative approach was initiated (1-5).
- Step 5: Obtain the signatures of the RN and therapists involved in the care.
- Step 6: Move to Section II. For each approach from 1 to 30, mark whether it was withheld, refused, or discharged as per the patient’s response.
- Step 7: Initial and sign next to each approach to confirm participation by all who worked on it.
- Step 8: Proceed to Section III to document the resident’s response and progress towards goals for each week (Week 1-5). Record responses and obtain signatures along with the respective dates.
- Step 9: In Section IV, review the plan of care and address each question (A-D). Indicate "Yes" or "No" as needed.
- Step 10: If any changes are required, make notes as necessary and plan to update the next month’s plan of care.
- Step 11: Ensure a final signature by licensed staff, along with the date at the end of Section IV.
By following these steps, you'll ensure that the 3643 form is filled out comprehensively and accurately, setting the stage for effective patient care and monitoring.
What You Should Know About This Form
What is Form 3643 and its purpose?
Form 3643 is used by the Texas Department of Aging and Disability Services as part of the Nursing Restorative Care Program. It serves as a structured outline for documenting a resident's plan of care, which helps professionals track and assess the goals and approaches for each individual's care. The form ensures a comprehensive approach to restorative care and fosters communication among staff members involved in the resident's care.
Who is responsible for filling out Form 3643?
The form must be completed by qualified healthcare professionals involved in the resident’s care, typically Registered Nurses (RNs) and therapists. These individuals will gather the necessary information, set goals, document approaches, and ensure the ongoing revision of the plan as needed.
What information is included in the Plan of Care section of Form 3643?
The Plan of Care section includes specific goals for the resident, approaches to achieve those goals, and the date when restorative care was initiated. This section is critical as it outlines the customized strategy for the resident’s rehabilitation and well-being.
How should changes to the Plan of Care be documented?
If changes are recommended during the monthly review, they must be documented by updating the Plan of Care in the next edition of Section I on Form 3643. It is essential to capture all necessary adjustments to ensure that care remains appropriate and tailored to the resident's needs.
What should be done if an approach is withheld or refused?
When an approach is withheld or refused, it is crucial to document the reason in the weekly notes. This transparency aids in understanding the resident’s preferences and needs, which can influence future care strategies.
How is the resident’s response monitored throughout the program?
Section III allows staff to document the resident's response and progress towards goals on a weekly basis. Each week, the responses are signed and dated by staff, providing a clear record of changes over time and facilitating ongoing evaluations of the care provided.
Can the program be discontinued, and how is this determined?
Yes, the program can be discontinued if it has been determined that it is no longer appropriate for the resident. This decision is made during the monthly review based on the staff's assessment of the Plan of Care's effectiveness. If the decision is made to discontinue the program, it should be documented appropriately in Section IV.
What are the signature requirements for Form 3643?
Every professional who initials the specific approaches must also sign the form below those initials. This requirement ensures accountability and indicates that all professionals are aware of the resident's care plan and their contributions to it.
Is there a specific date for which the form was originally designed?
Form 3643 was designed in November 1996. While the content and structure are still relevant, periodic updates may occur to reflect current best practices in restorative care and services for residents.
Common mistakes
Filling out Form 3643 can be a straightforward process, but it is essential to avoid common mistakes to ensure accuracy and compliance. A frequent error occurs when individuals forget to complete all sections. Each part of the form serves a purpose, and leaving some areas blank can lead to incomplete reporting or misunderstandings regarding the care plan.
Another common mistake is neglecting the resident’s name and room number. This information is crucial for identifying the specific resident being assessed. Without it, tracking responses and documenting progress becomes challenging, potentially leading to complications in care delivery.
In Section I, participants often fail to articulate clear goals. Vague goals can confuse caregivers and hinder effective monitoring of progress. Goals should be specific, measurable, achievable, relevant, and time-bound. Incomplete or unclear goals may result in inadequate care and dissatisfaction.
Incorrect signatures or initials is another issue that arises frequently. Each approach listed on the form must have corresponding initials and signatures from all involved therapists. Missing signatures can delay the review process and create accountability issues later on.
When documenting the resident's response and progress, individuals sometimes overlook the importance of consistency. Records should reflect a standardized format across all weeks. Inconsistent documentation can make it hard to assess the resident’s journey and might raise questions during reviews.
Additionally, some people do not adequately address the questions in Section IV—Monthly Review. Making sure to provide clear feedback on whether the plan remains appropriate or if changes are recommended is vital. These assessments allow for necessary adjustments to enhance the restorative program.
Finally, failing to update the Plan of Care in the next month if changes are recommended constitutes a critical oversight. Proper updates ensure that all involved caregivers are aware of any modifications and can implement them effectively. Keeping the plan current is essential for the continued success of the resident’s care.
Documents used along the form
The Form 3643 is a crucial document utilized in nursing restorative care programs. It outlines the plan of care for residents, ensuring that their rehabilitation goals are effectively tracked and monitored. Alongside this form, there are several other documents that are often used to support and complement the information contained in Form 3643. Below is a list of these forms, each accompanied by a brief description.
- Patient Assessment Instrument (PAI): This document provides a comprehensive assessment of a resident's medical, physical, and psychological needs. It helps create a tailored care plan that addresses the individual’s unique circumstances.
- Daily Progress Notes: These notes are filled out by nursing staff and therapists to record daily activities, observations, and any changes in the resident’s condition. They serve to keep track of the effectiveness of the restorative care provided.
- Care Plan Review Form: This form facilitates regular evaluations of the existing care plan, ensuring that it remains relevant and effective. It often prompts discussions among care team members about necessary adjustments based on the resident's progress.
- Incident Report Form: If there are any unexpected events or issues concerning the resident's care, this form is completed to document the incident. It helps identify trends or areas needing improvement in care practices.
- Discharge Summary: Once a resident is ready to transition out of restorative care, a discharge summary provides a comprehensive overview of the care provided, progress made, and recommendations for ongoing care or support.
These additional documents ensure that every aspect of a resident's care is systematically recorded, facilitating effective communication among the care team and prioritizing the well-being of the individual in care. Using these forms together helps create a holistic approach to maintaining and improving residents' quality of life.
Similar forms
-
Form 3644: Similar to Form 3643, this document includes a plan for care and tracks the progress of therapeutic approaches over time. It also requires signatures from professionals, ensuring accountability in care delivery.
-
Form 3645: This form serves to document the resident's goals and the frequency of services provided. Much like Form 3643, it includes a section for progress notes and requires staff members' initials and signatures for verification.
-
Form 3646: This document aligns with Form 3643 in that it captures monthly reviews of care plans. It asks similar questions about the appropriateness of goals and whether changes are required, promoting ongoing evaluation.
-
Form 3647: Like Form 3643, this form documents approaches and the resident's responses. It emphasizes communication among staff and specifies the importance of tracking each interaction with the resident, creating a comprehensive record.
-
Form 3648: This document shares similarities by outlining a detailed action plan for restorative care. It focuses on goals and includes necessary signatures from staff members, ensuring a collaborative effort in the resident's care.
Dos and Don'ts
When filling out the 3643 form, certain practices can help ensure that the process goes smoothly and that the information provided is clear and accurate. Here are five things to do and five things to avoid:
- Double-check all entries for accuracy before submitting the form.
- Use clear and concise language when documenting responses and progress.
- Ensure all signatures are collected from the required personnel, including initials on the approaches.
- Follow up on any withheld or refused approaches by documenting the reasons clearly.
- Regularly review and update the Plan of Care based on monthly reviews or changes in resident condition.
- Do not skip any sections, as incomplete forms may lead to processing delays.
- Avoid using abbreviations or jargon that may not be understood by all staff members.
- Do not neglect to document any resident responses in a thorough manner.
- Refrain from signing without thoroughly reviewing the entries to ensure accuracy.
- Do not overlook the importance of updating the Plan of Care if changes are needed.
Misconceptions
Misconceptions about the Texas Department of Aging and Disability Services Form 3643 can lead to confusion regarding its purpose and usage. Below are ten common misunderstandings along with clarifications to address them.
- This form is only for nursing facilities.
Actually, Form 3643 can be utilized in various settings, including home health care and rehabilitation centers, involving restorative care programs.
- Form 3643 requires only the RN’s signature.
In fact, multiple signatures are needed for verification. Both therapists involved in the care plan must also sign the form.
- The plan of care is static and doesn't change.
This is a myth. The form encourages regular reviews and updates to ensure that the care plan continues to meet residents' needs.
- All approaches must be implemented as written without exception.
This form allows for modifications. If an approach is refused or withheld, it must be documented, and adjustments can be made.
- Responses and progress toward goals are only noted once a month.
Conversely, responses are documented weekly. This allows continuous monitoring of the resident's progress and responsiveness to the plan.
- Form 3643 is not important for compliance reviews.
This form is crucial for compliance. It serves as documentation that can be critical during regulatory inspections and audits.
- Families do not need to be involved with the plan of care.
On the contrary, involving families is encouraged. Their insights can enhance the effectiveness of the care provided.
- Changes in approaches can be made without documentation.
This is incorrect. Any changes must be documented in the next month's section to ensure transparency and accountability in care.
- Only one goal can be set at a time.
In reality, multiple goals can be established. This approach allows for a comprehensive plan tailored to the resident’s individual needs.
- The form can be completed without staff collaboration.
Collaboration is essential. Input from all relevant staff members ensures a holistic approach to the resident's care.
Understanding the correct use of Form 3643 is vital for optimizing restorative care. Addressing these misconceptions can lead to better care outcomes and compliance with regulations.
Key takeaways
Here are key takeaways regarding the completion and use of the 3643 form from the Texas Department of Aging and Disability Services:
- The 3643 form is essential for documenting the plan of care for residents receiving nursing restorative care services.
- Goals and approaches must be clearly defined in the plan of care section, with sufficient detail on frequency and initiation dates.
- Thoroughly document any withheld or refused approaches in weekly notes, specifying reasons for clarity and accountability.
- Each professional involved must initial and sign beside their respective approaches, ensuring that all team members acknowledge their responsibilities.
- Conduct a monthly review to determine if the plan remains appropriate, updating the goals and approaches as necessary based on resident progress.
- Discharge decisions and continuation of the program should be supported by careful documentation and signatures from licensed staff.
Browse Other Templates
Sales and Use Tax Florida - The DR-15EZ form includes provisions for taxpayers to provide any changes in location or mailing address.
Va Unemployability - Witness signatures are required if your application contains a mark instead of a traditional signature.
End Stage Renal Disease Enrollment Form,ESRD Medicare Application,Medicare Kidney Disease Certification,Chronic Kidney Disease Registration Document,Renal Disease Patient Entitlement Form,ESRD Patient Medical Evidence Report,Kidney Transplant Eligibi - Information about prior treatments and care must be disclosed.